
Emotional Coping Assessment Tool
Emotional Assessment
This assessment helps you identify emotional challenges related to your pancreatic duct blockage and suggests appropriate coping strategies.
Rate your symptoms
Please select the option that best describes how you've felt in the past two weeks
When a pancreatic duct blockage prevents digestive enzymes from reaching the intestine, causing pain, nausea, and weight loss shows up, the physical symptoms can feel overwhelming. Yet the emotional toll often goes unnoticed, especially for patients and their families who suddenly have to navigate uncertainty, frequent medical appointments, and lifestyle changes.
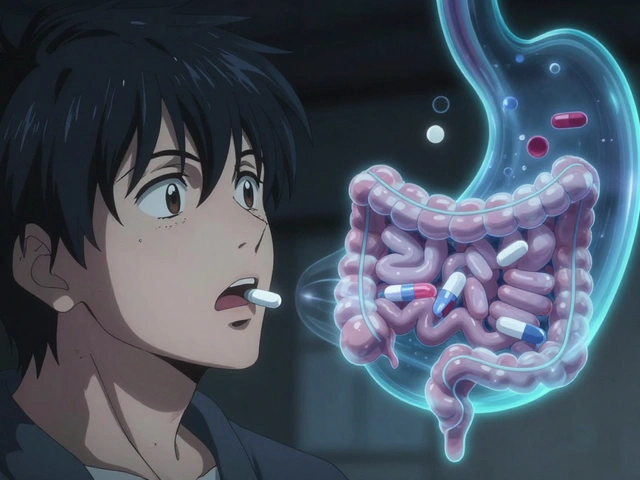
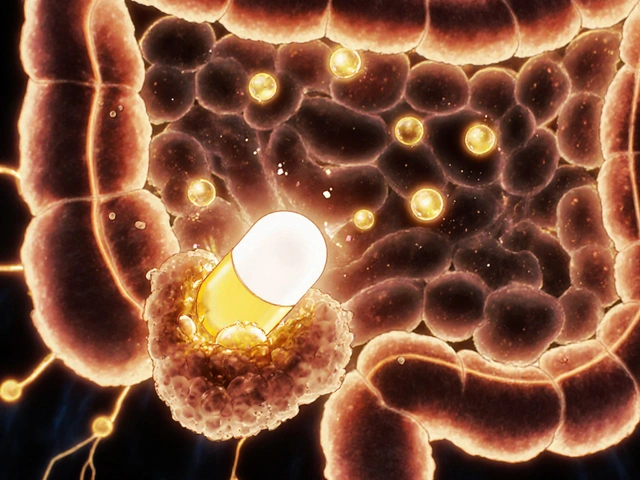
What Exactly Is a Pancreatic Duct Blockage?
The pancreas is a gland located behind the stomach that produces digestive enzymes and hormones like insulin has a network of tiny tubes called ducts. When one of these ducts gets clogged-whether by scar tissue, a stone, or a tumor-the flow of enzymes stops. This condition often leads to pancreatitis inflammation of the pancreas that can be acute or chronic, and in severe cases, it can signal the early stages of pancreatic cancer a malignant growth that develops in the pancreas. Treatment may involve procedures like endoscopic retrograde cholangiopancreatography (ERCP) a minimally invasive endoscopic technique to diagnose and sometimes clear blockages or placing a stent a small tube that keeps the duct open to allow enzyme flow.
Why the Emotional Side Matters
Living with a pancreatic duct blockage can feel like a roller coaster. The sudden onset of intense abdominal pain, fatigue, and dietary restrictions can trigger a cascade of feelings:
- Fear about the seriousness of the condition and possible cancer risk.
- Anxiety over upcoming medical procedures, hospital stays, and test results.
- Depression that creeps in when daily activities become limited and enjoyment fades.
- Guilt for worrying loved ones or feeling like a burden.
- Isolation because friends may not understand the complexity of the disease.
These emotions aren’t just "in the head"-they affect sleep, appetite, and even the body’s ability to heal. Acknowledging them early is the first step toward effective coping.
When to Seek Professional Mental‑Health Support
It’s normal to feel uneasy, but certain signs suggest it’s time to talk to a therapist, counselor, or psychiatrist:
- Persistent sadness or hopelessness lasting more than two weeks.
- Loss of interest in activities you once loved.
- Sleep disturbances-insomnia or oversleeping.
- Changes in appetite leading to significant weight loss or gain.
- Thoughts of self‑harm or feeling like a burden.
If any of these appear, reach out to a mental‑health professional promptly. Many hospitals have psychologists on staff who specialize in chronic illness, and they can provide tailored strategies that respect your medical regimen.
Build a Personal Coping Toolkit
Below is a menu of evidence‑based techniques you can mix and match. The goal is to create a routine that feels doable, even on bad days.
| Technique | How It Helps | Time Needed | Best For |
|---|---|---|---|
| Mindfulness breathing | Reduces acute anxiety, lowers cortisol | 5‑10 minutes daily | Immediate stress relief |
| Cognitive behavioral therapy (CBT) | Identifies negative thought patterns, builds coping statements | Weekly 50‑minute sessions | Persistent anxiety or depression |
| Guided imagery | Creates mental safe space, eases pain perception | 10‑15 minutes | Pain flare‑ups |
| Light exercise (walking, stretching) | Boosts endorphins, improves sleep | 20‑30 minutes most days | Overall mood lift |
| Journaling | Provides outlet for emotions, tracks triggers | 10‑15 minutes | Self‑reflection |
Start with one or two items that feel manageable. Consistency beats intensity; a short daily mindfulness practice often outweighs a sporadic hour‑long session.
Adopt Lifestyle Adjustments That Support Mental Health
Physical well‑being and emotional health are intertwined. Simple changes can make a huge difference:
- Nutrition: Work with a dietitian to create a low‑fat, enzyme‑supplemented meal plan that reduces pain after eating.
- Sleep hygiene: Keep a regular bedtime, limit screens, and use white noise if hospital noises disturb you.
- Pain management: Keep a log of pain levels, medication timing, and triggers; share it with your doctor to fine‑tune prescriptions.
- Hydration: Staying hydrated helps keep the ducts clearer and improves mood.
Even small wins-like a 15‑minute walk after a light meal-signal to your brain that you’re still in control.

Leverage Support Networks
Isolation is a common trap, but you don’t have to go it alone. Here are practical ways to connect:
- Support groups: Look for local pancreatic disease meet‑ups or online forums. Hearing others’ stories normalizes your feelings and often yields practical tips.
- Family and friends: Be clear about the type of help you need-whether it’s a grocery run, a listening ear, or help with medical paperwork.
- Professional counselors: Many therapists offer sliding‑scale fees or telehealth options, making access easier.
- Patient advocacy organizations: Groups like the Pancreatic Cancer Action Network provide resources, webinars, and occasionally one‑on‑one peer mentors.
When you share your experience, you also give others permission to speak up, creating a ripple effect of emotional support.
Work Closely With Your Medical Team
Open communication with doctors, nurses, and gastroenterologists reduces anxiety caused by uncertainty. Keep these habits:
- Prepare questions before each appointment. Write down symptoms, medication side effects, and emotional concerns.
- Ask for clarification on procedures like ERCP or stent placement; knowing what to expect diminishes fear.
- Request a care coordinator if the hospital offers one. They can streamline appointments and ensure you’re not missing follow‑up labs.
- Document progress in a simple notebook or app so you can track both physical and emotional changes over time.
When the medical team sees you’re proactive, they’re more likely to address the mental‑health aspect as part of the overall treatment plan.
Quick Checklist for Daily Emotional Care
- Practice 5‑minute mindfulness breathing each morning.
- Log pain, mood, and food intake after every meal.
- Schedule at least one brief social interaction-phone call, support‑group chat, or coffee with a friend.
- Review upcoming medical appointments; write down any worries to discuss with your doctor.
- Engage in light movement (walk, stretch) for 20 minutes.
Ticking these items off daily creates a sense of accomplishment and slowly builds resilience against the emotional roller coaster.
Can depression be a direct result of a pancreatic duct blockage?
Yes. Chronic pain, digestive issues, and the stress of repeated medical procedures can trigger depressive symptoms. It’s important to screen for depression early and involve a mental‑health professional as part of the treatment plan.
Is it safe to use over‑the‑counter anti‑anxiety meds while on enzyme supplements?
Generally, yes, but you should always check with your gastroenterologist or pharmacist. Some anxiolytics can affect stomach motility, which might alter how well enzyme supplements work.
How often should I attend a support group?
Frequency varies. Many patients find weekly virtual meetings helpful, while others prefer monthly in‑person gatherings. Try a few formats and stick with what feels most supportive.
What role does CBT play in managing chronic pain from a blockage?
CBT helps reframe pain‑related thoughts, reducing the emotional amplification of physical discomfort. By practicing coping statements and activity pacing, patients often report lower pain intensity scores.
Can diet alone relieve the emotional stress of this condition?
Diet is crucial for physical symptoms, but emotional stress usually needs a broader approach-mind‑body techniques, therapy, and social support work together with nutrition to improve overall wellbeing.
Write a comment
Your email address will not be published.




13 Comments
Honestly, these 'mind‑body hacks' are just fluff that therapists love to peddle.
Thank you for sharing such a comprehensive guide.
It is truly uplifting to see a resource that addresses both the body and the heart.
The emotional turbulence described feels like a storm that many of us have weathered.
By acknowledging fear, anxiety, and guilt, the article validates the hidden pain.
The suggested mindfulness breathing exercise offers a beacon of calm in the chaos.
Practicing five minutes each morning can anchor the mind before the day’s challenges arise.
Logging pain and mood after meals turns vague feelings into tangible data.
This data empowers both patients and clinicians to make informed adjustments.
Light movement, such as a gentle walk, releases endorphins that lift spirits naturally.
Connecting with a support group creates a chorus of shared experience that dispels isolation.
The emphasis on open communication with the medical team reduces the dread of the unknown.
When questions are prepared beforehand, appointments become partnerships rather than interrogations.
Scheduling brief social interactions each day nurtures a sense of belonging.
Finally, remembering that small victories, like a 15‑minute stroll, signal resilience is essential.
May everyone who reads this find the strength to apply these tools and reclaim their peace.
I appreciate how the guide weaves cultural sensitivity into dietary suggestions, acknowledging that food traditions vary widely.
Such inclusive advice helps patients feel seen beyond their diagnosis.
Exploring how CBT reframes pain perception reveals a powerful mental shift that complements physical treatment.
The article glosses over the harsh reality that not all patients can access therapy; insurance barriers remain a brutal obstacle.
Ignoring this systemic issue does a disservice to those truly suffering.
I hear your frustration, and indeed the cost and availability of mental‑health services can feel like a second blockade.
Integrating a simple hydration reminder into daily routines can subtly boost both digestion and mood.
While hydration helps, focusing on water alone distracts from the bigger issue of diet quality and medical oversight.
Sharing personal stories in support groups often lightens the emotional load and validates each participant’s experience.
Exactly, and when someone hears a peer describe coping with a similar blockage, it sparks hope and practical ideas you might not find in textbooks.
One must recognize that the medical literature often overlooks the psychosomatic interplay, treating the pancreas as an isolated organ rather than part of a holistic human system.
This reductionist view hampers true recovery.
The author's failure to cite recent neuro‑immune studies exemplifies a careless approach that undermines credibility.
Such omissions weaken the guide’s authority.
While constructive criticism is valuable, we should also acknowledge the practical strengths of the guide, such as its clear checklist format, which can empower patients to take actionable steps toward emotional well‑being.