
Blood Sugar Impact Calculator
Calculate Your Meal's Impact
Select your food and portion to see how it affects blood sugar levels.
Select food and portion to see results
Managing diabetes is a chronic condition where the body struggles to regulate blood glucose levels requires more than medication-it’s about shaping a diabetes management plan that fits everyday life.
Quick Takeaways
- Focus on low‑glycemic carbs, fiber and protein to keep blood sugar steady.
- Combine aerobic and resistance exercise at least 150 minutes a week.
- Use a monitoring tool-finger‑stick or continuous glucose monitor-to spot trends.
- Prioritise sleep, stress relief and foot care as part of the routine.
- Keep a simple daily checklist to stay on track.
Understanding the Basics
At its core, blood glucose refers to the amount of sugar circulating in your bloodstream is the primary fuel for cells. In people with diabetes, the body either doesn’t produce enough insulin the hormone that moves glucose into cells (type 1) or the cells become resistant to it (type 2). The long‑term health marker HbA1c measures average blood sugar over the past two to three months gives a picture of overall control; the target is usually under 7% for most adults.
Food Choices That Stabilize Blood Sugar
Carbohydrates are the biggest influence on glycemic index a scale that ranks foods by their impact on blood glucose. Choosing low‑glycemic options helps avoid spikes.
| Food | Glycemic Index | Typical Impact on Blood Sugar |
|---|---|---|
| Steel‑cut oats | 55 | Gradual rise, sustained energy |
| Quinoa | 53 | Steady, minimal spikes |
| Apple (with skin) | 36 | Gentle increase |
| White bread | 73 | Quick surge, rapid drop |
| Regular soda | 80 | Sharp spike, crash later |
Include plenty of fiber-vegetables, nuts, legumes-and pair carbs with protein or healthy fat. A simple plate rule works: half non‑starchy veg, a quarter lean protein, a quarter whole‑grain or low‑glycemic carb.
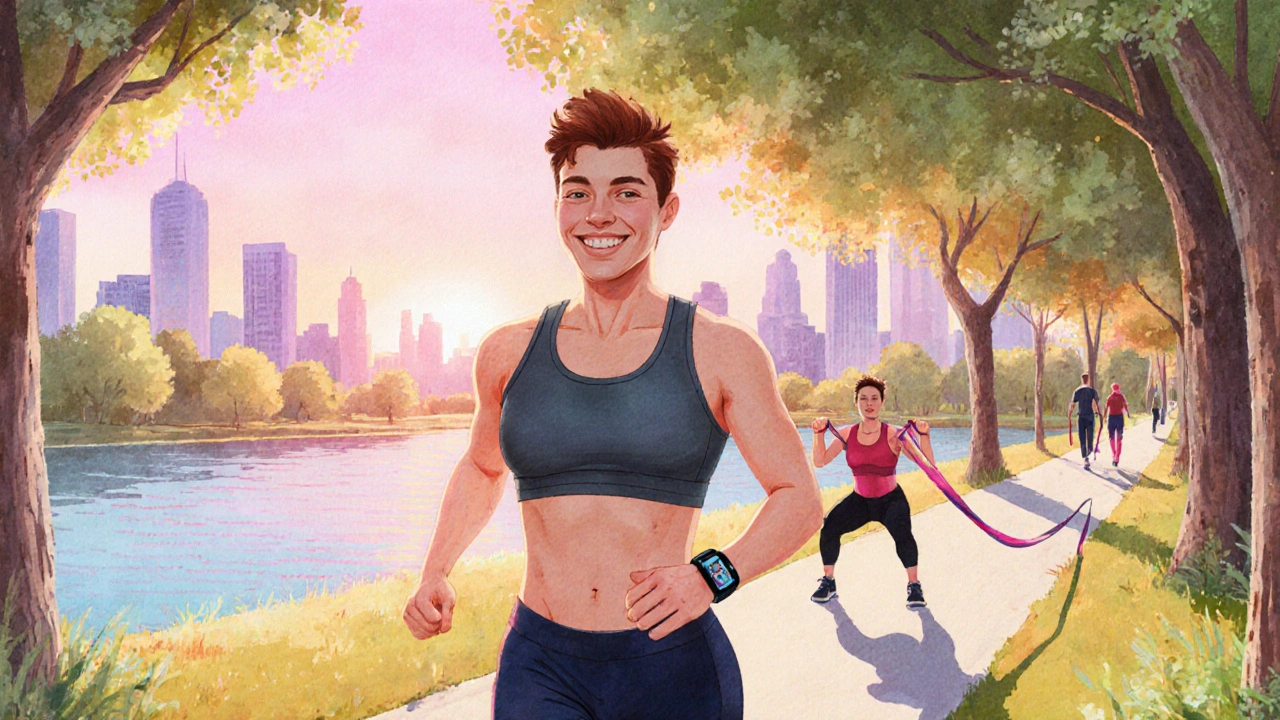
Building an Exercise Routine
Physical activity improves insulin sensitivity, meaning your cells need less insulin to absorb glucose. Aim for a mix:
- Aerobic: brisk walking, cycling, swimming-20‑30 minutes most days.
- Resistance: body‑weight squats, dumbbell rows, resistance bands-2‑3 sessions weekly.
- Flexibility: yoga or gentle stretching to reduce stress.
Start with what you enjoy; consistency beats intensity. If you’re new, a continuous glucose monitor tracks glucose in real time and can show how exercise affects levels helps fine‑tune timing and intensity.
Monitoring & Technology
Regular checks are the compass of any plan. Finger‑stick meters remain reliable, but CGMs provide trend arrows and alerts that prevent unnoticed lows.
When reviewing data, look for patterns:
- Do spikes occur after specific meals?
- Does activity consistently lower afternoon readings?
- Are bedtime numbers stable?
Use this insight to adjust meal timing, portion sizes or workout windows.
Everyday Habits That Matter
Beyond food and exercise, three habits often get overlooked:
- Sleep: Aim for 7‑9 hours. Poor sleep raises cortisol, which can raise glucose.
- Stress Management: Mindfulness, deep breathing, or short walks reduce hormones that push sugar up.
- Foot Care: Check feet daily for cuts or redness. Good circulation and controlled glucose reduce infection risk.

Common Pitfalls & How to Avoid Them
Skipping Meals-even if you’re counting carbs-can cause lows. Keep a snack handy, like a handful of nuts.
Over‑reliance on “diet” labels-some “low‑fat” products hide added sugars. Read the nutrition facts.
Ignoring Hydration-dehydration concentrates blood sugar. Aim for 6‑8 glasses of water daily.
Daily Checklist for Success
- ☑️ Log meals with carb count and glycemic rating.
- ☑️ Record blood glucose before and after meals.
- ☑️ Move for at least 30 minutes (walk, stretch, lift).
- ☑️ Review CGM or meter trends each evening.
- ☑️ Practice a stress‑relief technique (5‑minute breathing).
- ☑️ Check feet, hydrate, and get adequate sleep.
Frequently Asked Questions
Can I eat fruit if I have diabetes?
Yes, whole fruit provides fiber and nutrients. Choose low‑glycemic options like berries, apples with skin, or kiwi, and keep portions around one small piece or a half‑cup serving.
How often should I check my blood sugar?
For most adults on medication, test fasting, before meals, and 1‑2 hours after eating. If you use a CGM, trend data reduces the need for multiple finger‑sticks.
Is alcohol safe for people with diabetes?
In moderation, yes. Stick to one standard drink and consume with food to avoid sudden drops. Always monitor afterward.
Do I need a dietitian?
A registered dietitian can tailor a meal plan to your preferences, medication schedule, and cultural foods, making it easier to stay consistent.
What’s the best type of exercise for lowering HbA1c?
Combining aerobic activity (like brisk walking) with resistance training yields the biggest reduction in HbA1c, especially when done regularly for at least 150 minutes per week.
Write a comment
Your email address will not be published.




18 Comments
Honestly everyone thinks carbs are the enemy but that’s just hype. Eat what you want and watch the numbers not the myths.
The body is smarter than any diet plan.
Absolutely! You can totally crush those sugar spikes by moving more 🚀! Short walks after meals are game‑changers, keep that heart pumping!
In contrast to popular advice, excessive fiber intake may occasionally destabilize glucose homeostasis for certain individuals, thus moderation remains prudent.
Oh sure, because the universe obviously cares about your insulin levels – sarcasm aside, the only thing that truly controls blood sugar is your willingness to ignore it, isn’t it?
Listen, if you think a few cookies won’t hurt, you’re living in a fantasy land. Our nation’s health depends on real discipline, not sugar‑coated lies.
Look mate, the body’s like a well‑tuned engine – feed it crap and expect it to sputter. Simple maths: carbs in, insulin out, repeat.
Behold the epic saga of a plate piled high with polished grains, a tale as old as civilization itself; yet within that humble mound lies the silent tyrant of glucose, waiting to rise like an unwelcome tide, threatening the peace of your bloodstream, demanding vigilance, demanding balance, demanding sacrifice, and yet offering the fleeting pleasure of taste.
Oh yeah, because stuffing yourself with sugary snacks is a brilliant strategy – NOT. Grab a fruit, sip water, and watch those numbers behave.
I think its important to note that not every low‑carb fad works for everybody; some folks actually feel worse, so listen to your own body.
Honestly, when I first tried counting carbs I thought it was a punishment from the gods, but over time I realized it’s just a tool, like a hammer for a carpenter – you can build a healthy life if you swing it right, and you don’t have to become a monk to do it.
Keep moving!
From a metabolic perspective, glycemic load is the real KPI, not just simple carbs – you need to calibrate your macro‑nutrient ratios accordingly.
Managing diabetes is less about strict prohibition and more about mindful negotiation with your own physiology.
Each meal becomes a dialogue where you propose macronutrients and your body replies with insulin pulses.
When you respect that exchange, the resulting blood glucose curve tends to stay within a comfortable corridor.
Regular physical activity serves as a translator, making the language of glucose more fluent.
Even modest walks after dinner can reduce postprandial spikes with surprising efficiency.
Dietary fiber, especially soluble types, acts like a buffering agent, slowing absorption and smoothing peaks.
Conversely, refined sugars act as noise, disrupting the signal and forcing the pancreas to overreact.
Sleep quality is a silent moderator; poor rest amplifies hormonal stress, which in turn elevates glucose.
Stress management techniques, whether meditation or hobbies, further stabilize the endocrine environment.
Hydration should not be overlooked, as adequate water helps kidneys process excess glucose.
Routine self‑monitoring provides feedback, allowing you to adjust portions before patterns become entrenched.
Technology, such as continuous glucose monitors, offers real‑time insights that were once unimaginable.
Nevertheless, data alone is insufficient without the will to act on it consistently.
Community support, whether online forums or local groups, reinforces accountability and motivation.
Ultimately, the journey is incremental; small, sustainable choices accumulate into lasting health improvements.
Wow, because apparently the only way to stay alive is to turn every snack into a calculus problem – how thrilling.
Seriously – if you think you can cheat the system by hiding cookies in the pantry, think again; the body will find out and rant.
Did you know the food industry secretly funds research to keep us glued to sugary drinks? Wake up and question the labels!
While we acknowledge differing nutritional philosophies, it is essential to integrate evidence‑based glycemic indices, macronutrient distribution, and patient‑centered counseling-this holistic approach fosters consensus.
Agree, balancing carbs with activity is key, and staying consistent makes the biggest difference.