
When you have an autoimmune disease, it’s not just the pain or fatigue that wears you down-it’s the slow, silent loss of ability to do the things you once took for granted. Buttoning a shirt. Carrying groceries. Standing long enough to make coffee. These aren’t just inconveniences; they’re daily battles that chip away at independence. For millions living with conditions like rheumatoid arthritis, lupus, or Sjögren’s syndrome, functional impairment is the real enemy-not just the inflammation on a lab report.
What Functional Impairment Really Looks Like
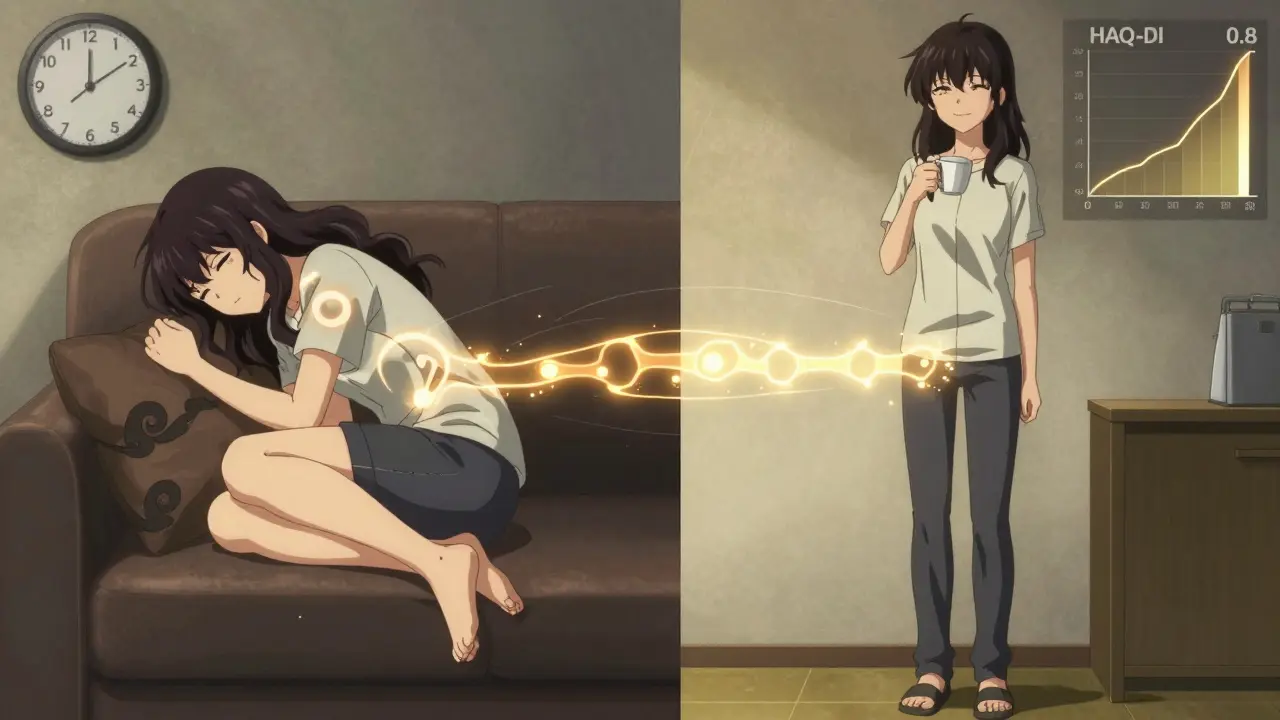
Functional impairment doesn’t mean you can’t walk. It means you can walk, but only if you skip lunch. It means you can wash your hair, but then you have to lie down for three hours afterward. It means your hands hurt so badly that opening a jar feels like a marathon. This isn’t laziness. It isn’t "just being tired." It’s the direct result of chronic inflammation damaging joints, nerves, and muscles, combined with the side effects of medications and the body’s own energy depletion. Studies show that 5-8% of people worldwide live with an autoimmune condition, and women make up 75% of that number. Among them, nearly two-thirds experience some level of functional decline within the first year of diagnosis. The Health Assessment Questionnaire Disability Index (HAQ-DI) measures this decline on a scale from 0 (no difficulty) to 3 (completely unable). A score above 1.5 means you’re struggling with basic tasks like dressing, bathing, or preparing meals. That’s not mild. That’s life-changing.Rehabilitation Isn’t Optional-It’s Essential
For too long, rehab was seen as something you did after surgery or injury. But for autoimmune diseases, it’s a frontline defense. The goal isn’t to "cure" the disease-it’s to keep you living your life despite it. And the evidence is clear: structured rehabilitation improves functional capacity by 35-42% when started early. The key? Timing. Starting rehab within the first 12 months of symptoms makes the biggest difference. After that, it’s still helpful-but harder to reverse the damage. Think of it like managing diabetes: you don’t wait until your foot is infected to start monitoring blood sugar. You start early, consistently, and adjust as needed.Physical Therapy: Rebuilding Strength Without Triggering Flares
Physical therapy (PT) focuses on movement, strength, and endurance. But here’s the catch: the wrong kind of exercise can make things worse. High-impact workouts, heavy lifting, or pushing through pain? That’s a recipe for a crash. Research shows 37% of patients who start intense programs without guidance end up with injuries that set them back weeks. Good PT for autoimmune conditions follows a careful, phased approach:- During flares: Gentle isometric exercises-muscle contractions without joint movement-at 20-30% of your max effort. No sweating. No strain.
- During remission: Low-impact aerobic training at 40-60% of your heart rate reserve. That’s about brisk walking or cycling where you can still talk but not sing.
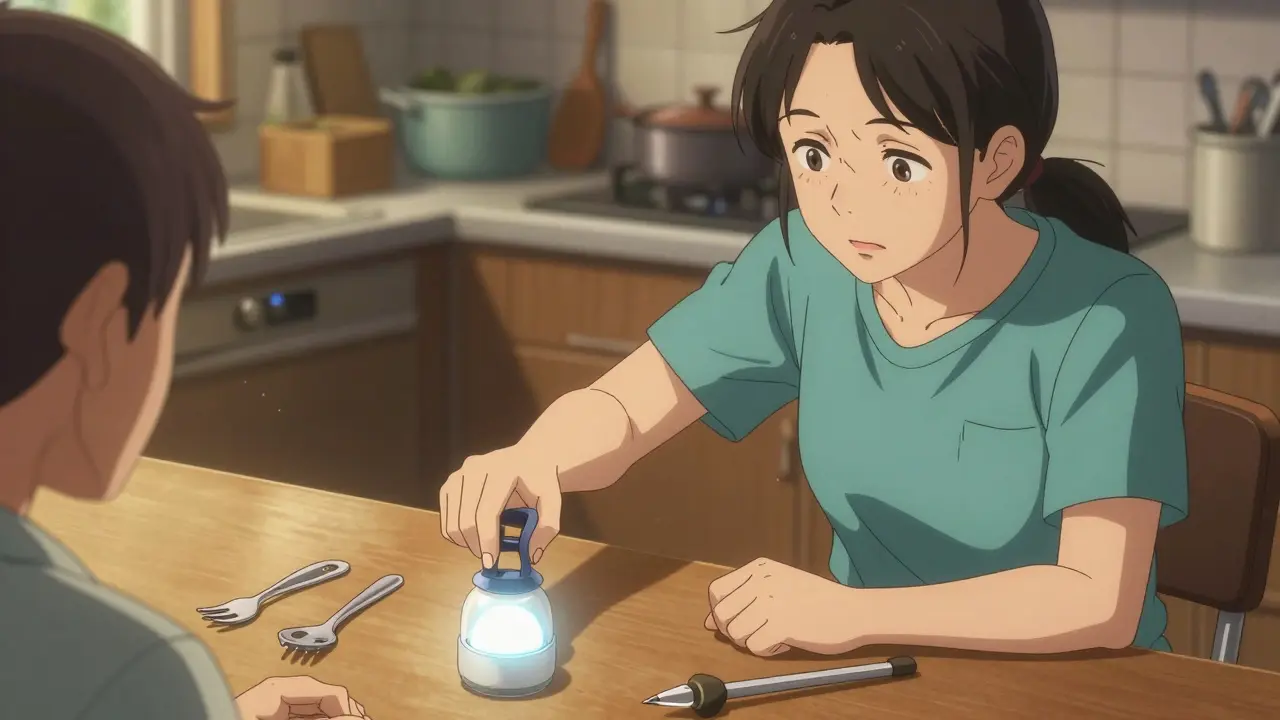
Occupational Therapy: Reclaiming Daily Life
While PT works on your legs, OT works on your hands, your brain, and your routine. It’s about adapting your environment and your habits so you can still cook, clean, work, and care for yourself-even with stiff fingers, fatigue, or brain fog. The cornerstone of OT is the 4 Ps:- Prioritize: What tasks matter most? Save energy for what you can’t skip.
- Plan: Break big tasks into small steps. Don’t try to clean the whole house in one day.
- Pace: Work for 15-20 minutes. Rest for 5-10. Repeat. This isn’t laziness-it’s strategy.
- Position: Use ergonomic tools, seated positions, and supportive devices to reduce strain.
Hydrotherapy: The Secret Weapon
Water changes everything. Warm water (92-96°F) reduces joint pressure, eases muscle spasms, and lets you move more freely than on land. Hydrotherapy cuts pain by 22% more than land-based exercise, dropping Visual Analog Scale scores from 7.2 to 4.1 on average. But here’s the problem: 68% of rural rehab centers don’t have underwater treadmills or therapy pools. Access is uneven. If you can’t get to a facility, ask your therapist about home-based water exercises-like seated leg lifts in a warm bath or gentle arm circles in a tub. It’s not the same, but it’s better than nothing.What Doesn’t Work-and Why
Not all rehab is created equal. Too many therapists treat autoimmune patients like they’re recovering from a sprained ankle. Pushing through pain? That’s a myth. Pain is your body’s warning light, not a badge of effort. Common failures:- Therapists ignoring the "boom-bust cycle"-where patients overdo it on good days, then crash for days afterward. 63% of patients experience this.
- Not accounting for central fatigue (fatigue from the brain/nervous system, not muscles). 19% of programs miss this entirely, making symptoms worse.
- Skipping the "70% rule"-never pushing beyond 70% of your perceived maximum effort. Exceeding that leads to flares.
How to Find the Right Therapist
Not every PT or OT knows how to handle autoimmune diseases. Look for someone with specialized training. The Academy of Pelvic Health Physical Therapy offers a 120-hour Autoimmune Specialty Certification. Only 78% pass it. That’s a good sign. Ask questions:- "Do you use the HAQ-DI or COPM to track progress?" (The Canadian Occupational Performance Measure is the gold standard.)
- "How do you adjust sessions during a flare?"
- "Do you use heart rate variability monitoring or activity diaries to personalize intensity?"
The Real Barriers: Cost, Access, and Misunderstanding
Insurance often covers only 12-15 sessions per year. But research shows you need 24-30 to see lasting results. That’s a gap most patients can’t bridge. And 31 U.S. states still don’t have specific billing codes for autoimmune rehab. That means 22% of claims get denied-just because the paperwork doesn’t match a "standard" diagnosis. Telehealth has helped. Since 2020, 68% of patients now use virtual sessions. Home-based programs with video coaching, activity trackers, and digital diaries are filling the gap. But they’re not perfect. You still need someone who understands your disease.What’s Next? The Future of Autoimmune Rehab
The NIH launched the Autoimmune Rehabilitation Registry in January 2023, tracking 5,000+ patients across 47 clinics. The goal? To personalize rehab using real-time data. New research is using blood markers like IL-6 to adjust exercise intensity weekly. If your inflammation spikes, your workout gets lighter. If it’s low, you can safely push harder. Early results show 39% better outcomes. And AI is coming. Apps like "PacePartner," now in Phase 3 trials, use wearable sensors to predict your flare risk with 82% accuracy. Imagine getting a notification: "Your body is showing early signs of a flare. Today, stick to 10 minutes of gentle stretching."Final Thought: It’s Not About Fixing You. It’s About Supporting You.
Autoimmune diseases don’t disappear. But they don’t have to steal your life either. Rehab and occupational therapy aren’t about making you "normal." They’re about helping you stay you-no matter how your body changes. The best outcomes come from patience, precision, and partnership. Work with a therapist who listens. Use tools that fit your life. Respect your limits. And remember: progress isn’t measured in how much you can do-it’s measured in how much of your life you get to keep.Can physical therapy make autoimmune symptoms worse?
Yes-if it’s done incorrectly. Pushing too hard, ignoring flares, or using high-impact exercises during active disease can trigger crashes and worsen inflammation. Effective rehab is tailored to your current condition. During flares, exercise should be gentle and non-jarring. The goal is to maintain function without provoking a flare, not to push through pain.
How long does it take to see results from rehab for autoimmune diseases?
Most patients notice small improvements in energy and mobility within 4-6 weeks. Meaningful gains-like being able to cook without resting afterward or walking to the mailbox without fatigue-typically take 3-6 months. The biggest improvements happen when therapy starts early and is consistent. Skipping sessions or stopping too soon often leads to setbacks.
Why is occupational therapy better than physical therapy for hand function?
Occupational therapy focuses specifically on how you use your hands in daily life-not just strength or range of motion. OTs teach adaptive techniques, recommend assistive tools, and modify tasks to reduce strain. For example, they might suggest a rocker knife for cutting food or a weighted pen for writing. PT improves muscle strength, but OT makes that strength useful in real-world tasks.
Is hydrotherapy worth it if I don’t have access to a pool?
Hydrotherapy is highly effective, but you don’t need a professional pool to benefit. Warm baths (92-96°F) with gentle range-of-motion exercises-like leg lifts, arm circles, or seated marching-can mimic many of the benefits. The warmth reduces stiffness and pain, and water’s buoyancy reduces joint pressure. While a pool is ideal, consistent home-based water exercises are better than no movement at all.
What’s the "70% rule" in autoimmune rehab?
The "70% rule" means never pushing yourself beyond 70% of your perceived maximum effort on any given day. This prevents overexertion, which often leads to a flare-up days later. It’s not about how you feel at the start-it’s about how you feel at the end. If you’re exhausted after a session, you went too far. Stay below 70% to avoid the "boom-bust" cycle.
Can I do rehab at home, or do I need to go to a clinic?
You can absolutely do effective rehab at home-especially with telehealth support. Many patients now use video sessions with certified therapists, activity trackers, and digital logs to monitor progress. Home programs are especially helpful for those in rural areas or with limited mobility. The key is working with a therapist who guides you remotely and adjusts your plan based on your daily symptoms.
Why do some therapists dismiss autoimmune fatigue?
Many therapists are trained in orthopedic or post-surgical rehab, where fatigue isn’t a primary concern. They may mistake central fatigue (a neurological symptom of autoimmune disease) for laziness or lack of motivation. This is a knowledge gap. Look for therapists who understand the difference between deconditioning and disease-related fatigue-and who use tools like heart rate variability or activity diaries to track real limits.
How do I know if my rehab program is working?
Ask for measurable tools: the Health Assessment Questionnaire Disability Index (HAQ-DI) or the Canadian Occupational Performance Measure (COPM). A 2-point improvement on the COPM is clinically significant. Track changes in daily tasks: Can you now shower without resting? Can you carry your own groceries? Progress isn’t always about strength-it’s about reclaiming control over your routine.
Write a comment
Your email address will not be published.



2 Comments
Love this breakdown. The HAQ-DI and COPM metrics are gold standards, but so few clinicians actually track them longitudinally. I’ve seen patients get discharged after 6 sessions because "they’re improving," but without objective data, you’re just guessing. The 70% rule is non-negotiable-I’ve had flares triggered by PT sessions that pushed past that threshold. And don’t even get me started on how often TENS units are misconfigured. 50-100Hz is the sweet spot for neuropathic pain, but I’ve seen therapists set them to 2Hz because "it feels better."
Also, the hydrotherapy stats? 22% pain reduction? That’s huge. But access is still a joke. My clinic in rural Ohio has one underwater treadmill, and it’s booked 3 weeks out. Home water exercises are underrated-seated leg lifts in a 94°F tub can be just as effective if you’re consistent. Just don’t use Epsom salts. They dehydrate you and worsen Sjögren’s dryness.
As someone who’s been in this game for 8 years, I can confirm: timing is everything. Starting rehab within the first 12 months? That’s the difference between maintaining independence and needing help to button a shirt. I went from HAQ-DI 2.3 to 0.9 in 5 months because my OT knew to prioritize the 4 Ps-especially pacing. You don’t "get stronger" by pushing through. You get stronger by conserving energy for what matters.
Also, voice-activated lights? Game changer. I used to drop things every time my fingers locked up. Now I say "Hey Google, turn on the kitchen light" and I don’t have to reach. Simple tech, massive ROI. Stop thinking rehab is just about exercise. It’s about redesigning your environment.