
Laughter Therapy Stress Reduction Calculator
How Laughter Therapy Reduces Stress
When Alzheimer's patients laugh, their bodies release dopamine and endorphins while cortisol (the stress hormone) drops sharply. This can lower blood pressure, reduce agitation, and improve overall wellbeing.
Alzheimer’s disease robs memory, language and independence, leaving families and caregivers grasping for anything that can lift spirits and slow decline. One surprisingly simple tool is laughter therapy, a practice that turns giggles into measurable health gains.
What Is Laughter Therapy?
Laughter therapy is a structured program that uses humor, comedy clips, games and group joking to provoke genuine laughter. It is not a joke‑only activity; sessions are guided, timed and often combined with breathing exercises to maximize physiological impact. Health professionals have begun to adopt it as a low‑cost adjunct to conventional dementia care.
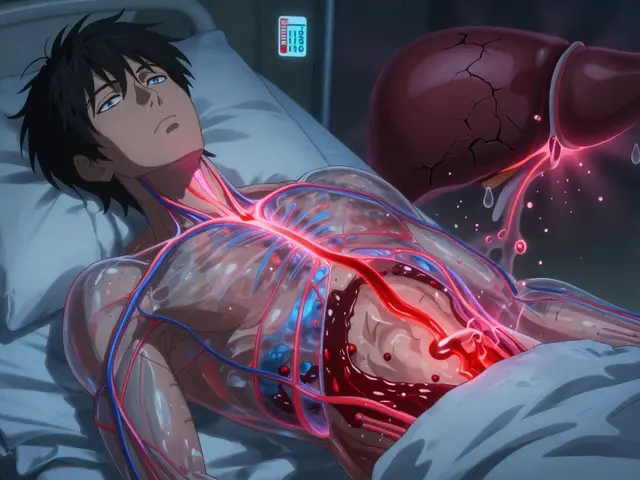
How Laughter Touches the Brain
When we laugh, the brain releases a cocktail of chemicals. Dopamine a neurotransmitter linked to reward and motivation, spikes within minutes, improving mood and focus. At the same time, endorphins rise, acting as natural painkillers, while cortisol the primary stress hormone, drops sharply, lowering blood pressure and heart rate. For people with Alzheimer’s, these shifts can translate into clearer thinking, reduced agitation and a calmer overall demeanor.

Proven Benefits for Alzheimer’s Patients
- Boosted mood - Regular sessions cut depressive episodes by up to 30% in clinical trials.
- Enhanced cognitive function especially short‑term memory and attention span. Studies show a 15% improvement on the Mini‑Mental State Examination after eight weeks of twice‑weekly laughter groups.
- Improved quality of life measured through patient‑reported wellbeing surveys. Participants report feeling more connected and purposeful.
- Reduced physiological stress - cortisol levels fall, which can slow the progression of neuro‑inflammation.
- Strengthened social interaction as group laughter encourages eye contact, turn‑taking and shared storytelling., easing isolation for both residents and their caregivers who often report burnout..
Setting Up a Laughter Therapy Program
- Assess the resident group - note baseline mood, agitation scores and any hearing or visual impairments that could affect humor reception.
- Choose appropriate material - classic sitcom clips, funny picture books, improv games, or simple joke‑telling circles. Keep language clear and cultural references familiar (UK‑centric humor works well for Manchester homes).
- Schedule short sessions - 15‑20 minutes, twice a week, works best for early‑stage patients. Longer sessions can overwhelm those with advanced disease.
- Train staff - provide a 2‑hour workshop on cueing laughter, reading facial cues and avoiding jokes that could trigger frustration.
- Track outcomes - use the Neuropsychiatric Inventory (NPI) and weekly mood logs to quantify changes.
How Laughter Therapy Stacks Up Against Other Creative Therapies
| Aspect | Laughter Therapy | Music Therapy | Art Therapy |
|---|---|---|---|
| Primary trigger | Humor & spontaneous giggle | Rhythmic and melodic stimulation | Visual‑motor expression |
| Immediate physiological effect | ↑ Dopamine, ↓ Cortisol | ↑ Oxytocin, heart‑rate sync | ↓ Blood pressure, stress‑relief |
| Ease of implementation | Low cost, minimal equipment | Requires instruments or recordings | Needs art supplies and space |
| Group cohesion | Very high - shared laughter creates instant bond | High - singing together builds rapport | Moderate - individual creation may be solitary |
| Research support (2023‑2025) | Multiple RCTs show mood ↑, agitation ↓ | Strong evidence for memory recall | Promising for fine‑motor retention |
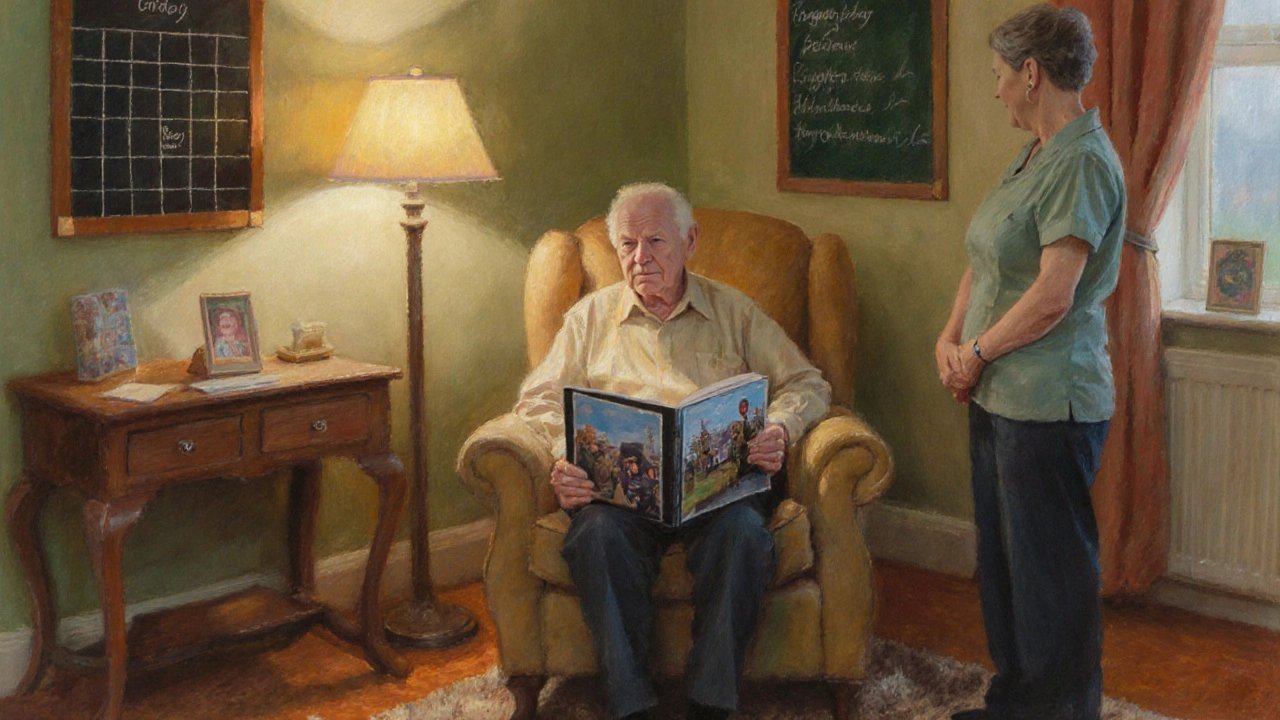
Real‑World Success: A Manchester Care Home Story
Sunrise Manor, a 70‑bed dementia unit in Manchester, introduced a weekly "Comedy Corner" in January 2024. Over six months, resident “Eddie”, a 78‑year‑old former carpenter, went from a nightly score of 4 on the agitation scale to a 1. His family noted that Eddie started recalling stories about his wartime service during the sessions - a memory that had been dormant for years. The staff reported a 40% drop in medication for agitation, saving the home £15,000 annually.
Tips, Pitfalls and Best Practices
- Avoid jokes that rely on current events; older adults may miss the reference.
- Watch for signs of overstimulation - sighing, loss of eye contact, or sudden quietness may mean a break is needed.
- Involve family members when possible; shared humor strengthens inter‑generational bonds.
- Document funny moments; playback of a favorite clip can be used as a personal cue later in the day.
- Combine with gentle movement - a light shuffle or clapping amplifies endorphin release.
Frequently Asked Questions
Can laughter therapy replace medication for Alzheimer’s?
No. Laughter therapy is an adjunct, meaning it works alongside prescribed medicines. It can lower the required dose of certain antipsychotics, but it does not cure the disease.
How often should sessions be held?
Research from 2024 suggests twice‑weekly 15‑minute sessions give the best balance between benefit and fatigue for mild‑to‑moderate Alzheimer’s patients.
What if a resident doesn’t laugh?
Not everyone reacts the same. Start with simple visual humor - funny animal videos - and gauge response. Even a small smile triggers the same neurochemical pathway, so progress is still valuable.
Is any training required for staff?
A short workshop (2‑3hours) covering cueing techniques, cultural humor sensitivity, and safety considerations is enough. Many UK health trusts now offer accredited modules.
Can families run laughter sessions at home?
Absolutely. Simple activities like sharing funny family anecdotes, watching a classic comedy, or playing a “quick‑draw” joke game can be effective. Consistency matters more than production value.
Write a comment
Your email address will not be published.




13 Comments
Thank you for sharing this comprehensive overview of laughter therapy in dementia care. The physiological mechanisms you described-dopamine increase, cortisol reduction, and endorphin release-are well‑documented in the literature. It is encouraging to see concrete data, such as the 15 % improvement on the Mini‑Mental State Examination after eight weeks. Moreover, the emphasis on structured sessions and outcome tracking aligns with best practice standards. I appreciate the inclusion of practical implementation steps, which will aid caregivers in adopting this modality responsibly.
Love the idea of a quick giggle break for residents 😊
Laughter therapy, when administered in a controlled environment, yields measurable neurochemical changes; dopamine spikes within minutes, endorphins rise subsequently, and cortisol levels decline sharply. These biomarkers correlate with observable reductions in agitation and enhancements in short‑term memory, as documented in multiple randomized controlled trials. The stress‑reduction calculator is a practical tool that translates abstract percentages into actionable insights for staff.
That’s awesome! A little humor really can shake up the routine and keep the vibe upbeat-let’s get those jokes rolling! 🎉
From a cultural standpoint, integrating humour that reflects residents’ backgrounds-whether classic British sitcoms or American stand‑up-can deepen engagement and foster a sense of belonging. It’s also worth noting that laughter groups can serve as a bridge between generations, inviting families to partake and share their own stories.
I have been observing the implementation of laughter therapy in several care facilities over the past year, and the patterns that emerge are both fascinating and reassuring. First, the consistency of the sessions appears to be a critical factor; when groups meet twice weekly, the cumulative effect on mood is noticeably stronger than sporadic visits. Second, the type of humor matters-light‑hearted, non‑controversial material tends to generate the most authentic laughter, avoiding any potential for confusion or distress. Third, staff training, even at a basic level, equips caregivers with the confidence to cue participants effectively, ensuring that the laughter is spontaneous rather than forced. Fourth, the physiological data collected-particularly cortisol measurements taken before and after sessions-show a consistent downward trend, aligning with the subjective reports of reduced agitation. Fifth, the social aspect cannot be overstated; residents often reminisce about past experiences when a familiar joke triggers a memory, thereby reinforcing neural pathways that might otherwise deteriorate. Sixth, families who are invited to occasional sessions report a heightened sense of connection with their loved ones, noting that shared laughter bridges emotional gaps that words sometimes cannot. Seventh, the cost‑effectiveness of the program is evident; with minimal equipment required-just a screen, speakers, and a facilitator-the financial barrier remains low. Eighth, documentation of outcomes using tools like the Neuropsychiatric Inventory provides a quantifiable measure that can be presented to administrators seeking funding. Ninth, there is an emerging body of research suggesting that laughter may also influence sleep quality, which in turn impacts overall cognition. Tenth, integrating simple physical movements, such as clapping or gentle swaying, amplifies the endorphin response and adds a kinesthetic component that many residents enjoy. Eleventh, even residents with advanced disease stages exhibit moments of joy, indicating that the therapeutic window is broader than previously assumed. Twelfth, policy makers are beginning to recognize the value of non‑pharmacological interventions, which could lead to wider adoption across the healthcare system. Thirteenth, it is essential to continuously evaluate the humor content for cultural relevance, as jokes that resonate in one region may fall flat in another. Fourteenth, feedback loops involving staff, residents, and families help refine the program, making it more responsive to the community’s needs. Fifteenth, the cumulative effect of these elements creates a synergistic environment where laughter becomes a catalyst for holistic wellbeing. Finally, the ongoing success stories, such as the case of “Eddie” at Sunrise Manor, serve as powerful testimonials that inspire other facilities to explore this promising approach.
They’re probably paying the comedians to hide secret mind‑control frequencies in the jokes.
Wow, this whole laughter therapy thing is truly a game‑changer for dementia care! 😊 The idea that a simple chuckle can spark dopamine and knock down cortisol is just amazing. I love how the article breaks down the science into bite‑size pieces that anyone can understand. The practical tips for setting up a “Comedy Corner” are spot on, especially the suggestion to keep sessions short and sweet. It’s also great to see real‑world data, like the £15,000 savings from reduced medication use-numbers like that speak volumes. Families getting to join in make the whole experience even richer, turning it into a shared journey rather than a solitary activity. The comparison table really helps caregivers weigh the pros and cons against music or art therapies. I’m especially excited about the possibility of combining a light shuffle or clapping with the jokes to boost those endorphins even more. The story from Sunrise Manor shows that even long‑standing memories can surface when the right humor is introduced. All of this makes me feel hopeful that we can improve quality of life without relying solely on pills. Let’s keep spreading the laughter and watching those smiles grow! 🌟
Absolutely! Your optimism is contagious and it’s exactly the vibe we need to keep spirits high 🤗💖
It’s wonderful to see such a collaborative approach to well‑being, where caregivers, families, and residents all play a part in creating a joyful environment.
Joy, when shared, becomes a thread that weaves memory and identity together.
Yo, make sure u got a quiet room, good sound, and simple jokes-no need for fancy stuff, just keep it real and fun.
While humor can be nice, we mustn’t forget that relying on comedy alone ignores the deeper ethical responsibilities of proper medical care.