
Every year, about 6 million women in the U.S. get pregnant. And about 80% of them take at least one medication during that time-antidepressants, asthma inhalers, thyroid pills, even antibiotics. But here’s the problem: pregnancy registries are the only real way we know what these drugs might do to a developing baby. Clinical trials don’t include pregnant women. Ethically, they can’t. So when a drug hits the market, we’re flying blind-until a registry starts collecting real-world data.
Why Pregnancy Registries Exist
Pregnancy registries weren’t created out of curiosity. They came out of tragedy. After thalidomide caused thousands of babies to be born with missing limbs in the 1960s, regulators realized they needed a system to catch dangerous side effects after a drug was already on the market. Today, both the FDA and the EMA require pregnancy registries for certain medications-especially biologics, psychiatric drugs, and antiseizure medicines-when there’s a high chance women of childbearing age will use them. These aren’t passive databases. They’re active, ongoing studies. Women are enrolled as soon as they start taking a medication during pregnancy. Researchers collect exact details: what drug, what dose, when they took it, whether they smoked or drank, if they have diabetes or high blood pressure. Then they follow the pregnancy all the way through-tracking miscarriages, preterm births, low birth weight-and check the baby for birth defects at birth and sometimes up to a year later.What We’ve Learned So Far
Some of the most important safety insights have come from registries focused on psychiatric medications. The National Pregnancy Registry for Psychiatric Medications, run by Massachusetts General Hospital, has tracked over 2,000 pregnancies since 1999. What did they find? For most antidepressants like sertraline and citalopram, the risk of major birth defects is no higher than the general population’s baseline of 3%. That’s reassuring. But for some older drugs, like valproic acid (used for epilepsy and bipolar disorder), the risk of neural tube defects jumps to 10% or more. That’s why doctors now avoid it in pregnancy unless there’s no alternative. For biologics-drugs like Humira or Enbrel used for autoimmune diseases-registries have shown that many are safe. In fact, stopping these drugs during pregnancy can be riskier than taking them. Uncontrolled inflammation from conditions like Crohn’s disease or rheumatoid arthritis can lead to preterm birth or low birth weight. Registries helped flip the script: sometimes, staying on medication is the safer choice. Even vaccines are now being tracked. The CDC and FDA launched a registry for COVID-19 vaccines in pregnancy in 2021. Over 100,000 women enrolled. The data showed no increased risk of birth defects, preterm birth, or stillbirth. That helped calm fears and boosted vaccination rates among pregnant women.The Limits of Registries
Here’s the hard truth: registries can’t tell you everything. They’re great at spotting big risks-like a drug that causes a pattern of severe defects. But they’re terrible at catching small increases in rare problems. Let’s say a birth defect happens in 1 out of 1,000 babies. If a drug doubles that risk, you’d need over 1,200 exposed pregnancies just to detect it with statistical confidence. Most registries only enroll a few hundred women. Many enroll far fewer. That’s why you’ll often hear doctors say, “We don’t know for sure, but the data looks reassuring.” That’s not evasion-it’s honesty. Registries don’t prove safety. They help rule out major dangers. A drug that’s been studied in 500 pregnancies and shows no red flags isn’t “proven safe.” It just means if there’s a serious risk, it’s probably rare. Another problem? Enrollment. Only 15 to 20% of eligible women actually join. Some are afraid of being treated like lab rats. Others don’t want to share personal health details. Some don’t even know registries exist. Doctors don’t always bring it up. And even when they do, many women are too anxious to sign up. One woman in the psychiatric registry told researchers, “I just needed to know if my medication would hurt my baby. But the registry didn’t give me an answer right away. That was the hardest part.”
How Registries Compare to Other Methods
You might wonder: why not just use electronic health records or insurance claims? Those systems have millions of records. But they’re messy. They don’t capture exact drug doses. They don’t know if a woman took her pills consistently. They often don’t record why a drug was prescribed-was it for depression? Anxiety? Migraine? That matters because the underlying condition itself can affect pregnancy outcomes. A registry asks: “Why are you taking this?” and records it accurately. Case-control studies-where researchers compare women whose babies had birth defects to those whose didn’t-can be faster. But they rely on memory. Did you take that pill in week 6? You might not remember. Registries collect data in real time. No guesswork. The best approach now? Use registries to find signals, then use big data to confirm them. The FDA’s new Pregnancy Safety Research Network is trying to link registry data with health records from 100+ hospitals. That way, a small registry that spots a possible link between a drug and a rare heart defect can be validated by looking at 50,000 more pregnancies.Who Runs These Registries?
Most are run by academic medical centers-like Harvard, Johns Hopkins, or Massachusetts General-with funding from drug companies and government grants. The companies pay for them because regulators require it. But the research is independent. Data is analyzed by scientists, not the drug makers. There are over 80 active registries in the U.S. alone. The biggest ones focus on:- Psychiatric medications (12 registries)
- Antiepileptic drugs (8 registries)
- Biologics for autoimmune diseases (15 registries)
- Diabetes medications
- Antivirals and HIV treatments
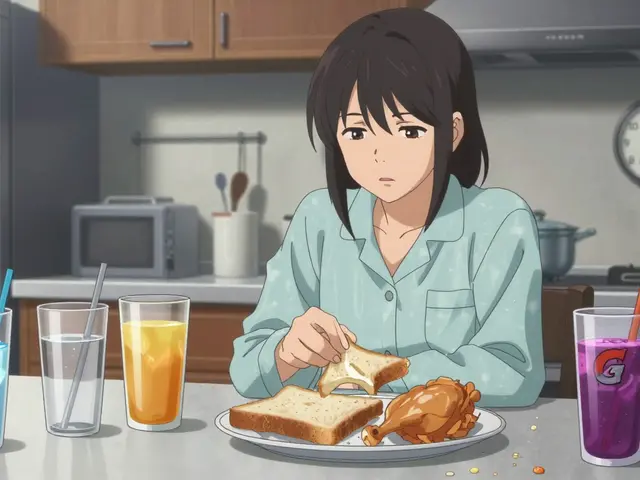
What It’s Like to Participate
If you’re pregnant and taking a medication, you might be asked to join a registry. It usually starts with a phone call or online form. You’ll answer questions about your health, your meds, your family history. You might get follow-up calls at 28 weeks, after delivery, and at 6 or 12 months postpartum. Some ask for permission to pull your medical records. Others just want to know how you and your baby are doing. Most women say they’re glad they joined. MotherToBaby, which runs several registries, found that 78% of participants felt they were helping future moms. Many appreciated getting personalized updates-like, “Based on the data we’ve collected, your medication doesn’t appear to raise the risk of heart defects.” That kind of info reduces anxiety. But it’s not easy. Some women drop out. Others feel guilty if they can’t complete follow-ups. One participant said, “I missed my 6-month check-in because my baby was sick. I felt like I failed the study.” Registries are trying to be more flexible now-offering text reminders, home visits, telehealth check-ins.The Future of Pregnancy Safety
The field is changing. In 2024, the National Pregnancy Registry for Psychiatric Medications added 18 new drugs to its list, bringing the total to 45. The FDA is pushing for longer follow-ups-tracking children up to age 5 to look for learning delays or behavioral issues. And there’s growing pressure to include more diverse populations. Most registry participants are white, middle-class, and insured. That’s a problem. We need data from Black, Hispanic, Indigenous, and low-income women too. Registries won’t replace other tools. They’re one piece of a bigger puzzle. But for now, they’re the most reliable source we have. Every time a woman joins, she’s not just protecting her own baby. She’s helping the next woman who takes the same pill.So if your doctor mentions a pregnancy registry-don’t dismiss it. It’s not just research. It’s the closest thing we have to a safety net.
Write a comment
Your email address will not be published.




8 Comments
Man, I never realized how much we’re flying blind with meds in pregnancy. It’s wild that we’ve been giving women drugs for decades without knowing the real risks. I get why trials exclude pregnant people-it’s ethical-but it leaves everyone in this weird limbo. I had a friend who took sertraline while pregnant and was terrified every week. She didn’t even know registries existed until her OB mentioned it. Honestly? If this is the best we’ve got, we need to make it way easier to join. No one should feel like a lab rat just trying to protect their kid.
Love this breakdown. Seriously. I work in public health and the fact that we’re using real-time, longitudinal data instead of messy EHRs? Genius. And yeah, the 15-20% enrollment rate is a disaster. But here’s the thing-drug companies are the ones funding this, and they’re not doing it out of the goodness of their hearts. They’re scared of lawsuits. So if we want better data, we need to stop treating registries like optional charity and start treating them like mandatory safety infrastructure. Period.
Okay but let’s be real-this whole registry thing feels like a PR stunt wrapped in science. They say ‘we don’t know for sure’ but then act like the data’s gospel. Meanwhile, 80% of pregnant women are on meds and we’re still using 1990s-era tracking. And don’t even get me started on the diversity problem. You think a white, middle-class woman in Boston is representative of a Latina mom in El Paso with no insurance? Nope. This isn’t science. It’s a luxury for people who can afford to care. Also, why are we still using ‘birth defects’ as a term? Sounds so 1950s. Just say ‘adverse outcomes.’
Registries are statistically underpowered, methodologically flawed, and ethically compromised. The reliance on self-reported data, even if real-time, introduces massive recall bias. The lack of control for confounders-like maternal BMI, prenatal care access, socioeconomic stressors-is egregious. And the funding model? Pharma-sponsored academic research is an oxymoron. The FDA’s ‘safety net’ is a house of cards built on convenience, not evidence. We need RCTs. Or at least a national cohort. This is not science. It’s performative diligence.
U.S. leads the world in pregnancy safety research. Other countries? They’re still guessing. We’ve got 80+ registries, real-time tracking, and data going back 25 years. Meanwhile, Europe just shrugs and says ‘maybe it’s fine.’ And now some woke activist wants to ‘include more diverse populations’ like that’s the issue? The problem isn’t race-it’s compliance. If women don’t show up for follow-ups, that’s not systemic racism, that’s personal responsibility. We don’t need more studies. We need women to stop being paranoid and start participating.
OMG I JUST JOINED A REGISTRY!!! 🤰💖 I was so scared about my anxiety med but now I get monthly updates and they even sent me a little sticker pack?? I feel like a superhero for helping other moms!! 🌟💊 #PregnancyRegistryHero 🏆
My sister joined a registry when she was pregnant with twins and on insulin. She said the hardest part wasn’t the calls-it was the guilt when she missed one because her baby was in the NICU. We need to stop treating participation like a checklist and start treating it like community care. Text reminders? Home visits? Translation services? That’s not extra-it’s essential. And if we’re gonna ask women to share their most vulnerable moments, we owe them more than a dry data sheet. We owe them connection.
As someone from India where prenatal care is still a luxury for many, I see this as a global privilege. In my village, women take whatever pills are sold at the pharmacy with no follow-up, no registry, no info. We need to think beyond Western academic models. Mobile-based registries. Voice-based surveys in local languages. Community health workers collecting data. This isn’t just about better science-it’s about justice. If safety data only helps the insured, then we’ve already lost.