Bioavailability: What It Means for Drug Effectiveness and Your Health
When you take a pill, not all of it reaches your bloodstream—that’s where bioavailability, the percentage of a drug that enters circulation and becomes active in the body. Also known as drug absorption rate, it’s the silent factor that decides whether a medication works, fails, or causes side effects. Two pills with the same label can behave completely differently in your body because of bioavailability. That’s why a generic version of a drug might not feel the same as the brand—even if they contain the same active ingredient.
Bioavailability isn’t just about the drug itself. It’s shaped by how it’s made, what’s in it, and even what you eat before taking it. For example, some drugs need fat to be absorbed properly. Others break down too fast in the stomach. And if a generic manufacturer changes the filler ingredients, it can drop bioavailability by 20% or more—enough to make a diabetes pill less effective or an antibiotic fail to clear an infection. This is why the FDA requires generics to prove they match the original in bioavailability, usually within 80–125% of the brand. But real-world results? They don’t always line up. Patients on epilepsy meds, blood thinners, or HIV drugs often report changes after switching to generics—not because the active ingredient changed, but because the body absorbed it differently.
It also ties into how doctors choose treatments. A drug with low bioavailability might need a higher dose, which increases side effects. Or it might need to be taken with food, which messes with daily routines. That’s why combination therapies, like those for hypertension or diabetes, often use lower doses of multiple drugs: each one has better bioavailability when paired, reducing the burden on your body. And when you’re dealing with kidney issues, aging, or pregnancy, bioavailability shifts again. A drug that worked fine last year might need a dose change now because your body’s absorbing it differently.
What you’ll find below are real stories and clear breakdowns of how bioavailability affects everything from HIV treatment and anticonvulsants to generic substitutions and pregnancy safety. You’ll see why a simple change in formulation can lead to viral rebound, why some antibiotics work better than others for UTIs, and how a supplement like St. John’s Wort can tank the levels of life-saving drugs. These aren’t theoretical concerns—they’re daily realities for people managing chronic conditions. This isn’t about chemistry lectures. It’s about making sure your medication actually does what it’s supposed to.
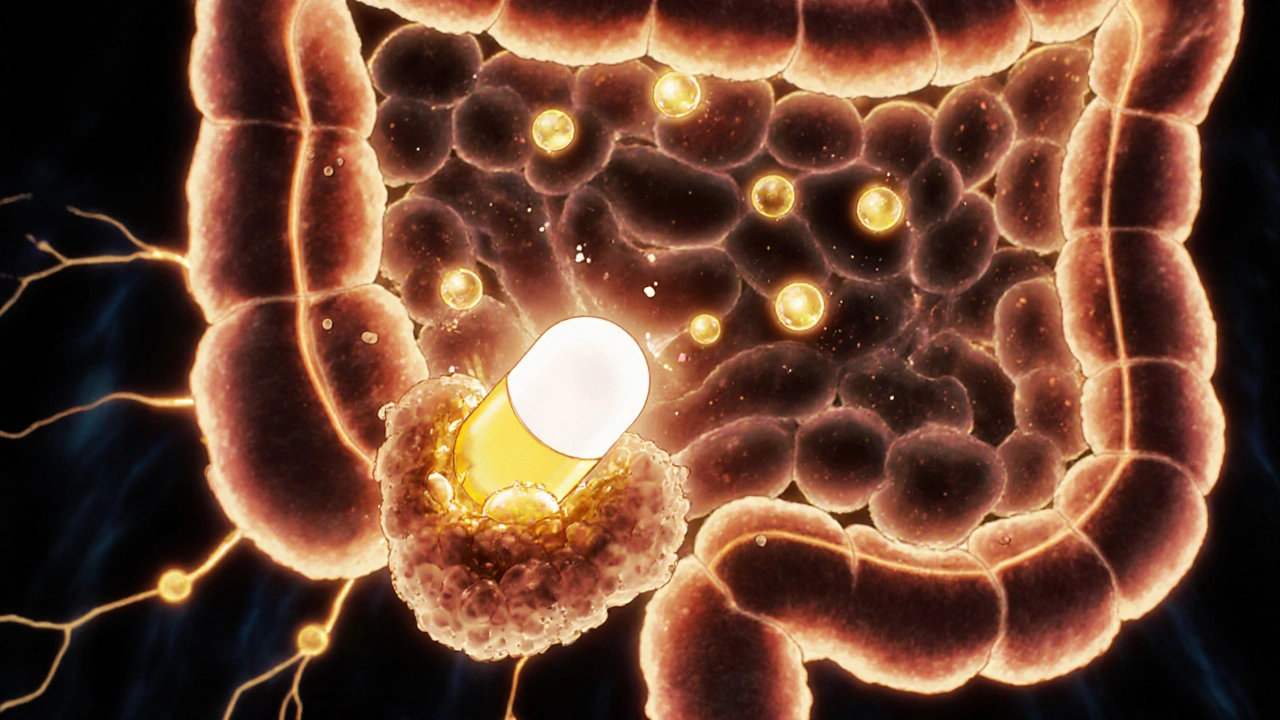
How Fatty Foods Boost Absorption of Lipid-Based Medications
Fatty foods enhance absorption of lipid-based medications by triggering bile release and fat-digesting enzymes that help dissolve poorly soluble drugs. This food effect can boost bioavailability by up to 300% for certain drugs like cyclosporine and fenofibrate.