Lipid-Based Medications: How Fat-Soluble Drugs Work and Why They Matter
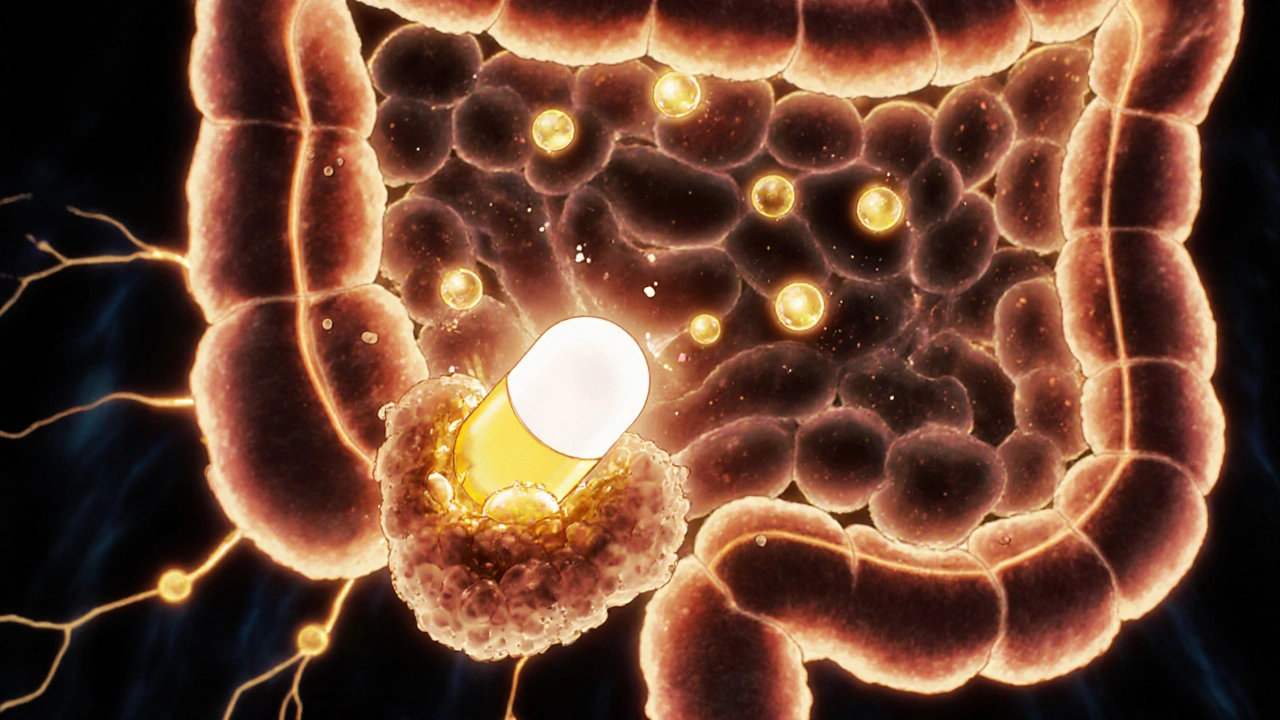
When a drug needs to slip through your cell membranes but won’t dissolve in water, lipid-based medications, pharmaceutical formulations designed to dissolve in fats rather than water. Also known as fat-soluble drug systems, they’re the quiet heroes behind many treatments that would otherwise fail to reach their target. Think of them as tiny oil-coated capsules that sneak past your body’s natural barriers—something water-soluble drugs just can’t do. These aren’t just fancy packaging; they’re engineered solutions for drugs that are too stubborn to be absorbed on their own.
Bioavailability, how much of a drug actually enters your bloodstream and becomes active is the biggest hurdle for many modern medications. Without lipid-based delivery, drugs like certain antivirals, cancer treatments, and even some vitamins would be useless. That’s why drug delivery, the science of getting medicines where they need to go in the body has become one of the most critical fields in pharmacy. Lipid-based systems aren’t just about solubility—they help drugs cross the blood-brain barrier, reach liver cells, or penetrate thick tumor tissue. They’re used in everything from HIV protease inhibitors to cholesterol-lowering agents.
It’s not magic—it’s chemistry. These formulations often use oils, phospholipids, or surfactants to wrap the drug in a fat-friendly shell. That shell lets the medicine ride through your digestive system without breaking down too early. Once it hits the right spot, your body breaks the shell open and releases the active ingredient where it’s needed. This is why some pills work better than others, even if they contain the same chemical. The delivery method changes everything.
You’ll find lipid-based systems in treatments for chronic diseases where precision matters: diabetes, heart conditions, neurological disorders, and even infections that hide deep in tissues. They’re behind many of the newer generics that finally make expensive brand drugs affordable—because once the delivery tech is cracked, manufacturers can copy it without reinventing the wheel. That’s why you see so many posts here about drug costs, generic access, and interactions—lipid-based delivery plays a silent role in all of it.
And while these systems boost effectiveness, they also come with trade-offs. Some require refrigeration. Others need to be taken with food. A few can interact with other fat-soluble substances—like St. John’s Wort or certain supplements—which is why drug interactions show up so often in our collection. Getting the dose right isn’t just about milligrams; it’s about how the drug is built.
What you’ll find below isn’t just a list of articles. It’s a practical guide to how modern medicine actually works under the hood. From how generics get approved to why some drugs need special handling, every post ties back to the same truth: the way a drug is delivered can be just as important as what’s inside it. Whether you’re managing diabetes, fighting infection, or just trying to understand why your prescription works (or doesn’t), this collection gives you the real story behind the pill.
How Fatty Foods Boost Absorption of Lipid-Based Medications
Fatty foods enhance absorption of lipid-based medications by triggering bile release and fat-digesting enzymes that help dissolve poorly soluble drugs. This food effect can boost bioavailability by up to 300% for certain drugs like cyclosporine and fenofibrate.