
When you’re on medication, the goal isn’t just to treat the condition-it’s to do it without making you feel worse. Many people know the frustration: you take a pill for high blood pressure, but now you’re dizzy. You take one for diabetes, but your stomach is in knots. What if there was a way to get the same or better results with fewer side effects? That’s where combination therapy comes in.
Why Stack Pills Instead of Cranking Up the Dose?
For decades, doctors reached for higher doses when a single drug wasn’t enough. But increasing the dose doesn’t always mean better results-it often means more side effects. Take blood pressure meds: doubling the dose of an ACE inhibitor might lower your pressure a little more, but it also doubles your risk of cough, swelling, or kidney issues. That’s not a trade-off most people are willing to make. Combination therapy flips that logic. Instead of one drug at full strength, you use two or more drugs, each at half-or even a third-of their usual dose. The trick? They work in different ways. One relaxes blood vessels. Another helps your kidneys flush out salt. Together, they hit the problem from multiple angles. The result? Better control, fewer side effects. Studies back this up. In a 2023 trial with over 15,000 patients, those started on a combination of two low-dose blood pressure drugs reached their target pressure in 63 days. Those on single drugs took nearly twice as long-117 days. And they were 34% less likely to have a heart attack or stroke.Real-World Examples: What This Looks Like in Practice
This isn’t theory. It’s standard care now in several major conditions.High Blood Pressure
The European Society of Cardiology recommends starting with a low-dose ACE inhibitor plus a calcium channel blocker for most patients with stage 2 hypertension. For example: lisinopril 5 mg + amlodipine 2.5 mg. That’s half the usual dose of each. In real patients, this combo lowers systolic pressure by nearly 9 mmHg more than a full dose of either drug alone. And side effects? Swelling drops from 14% to 4%. Cough goes from 10% to 2%.Diabetes
Metformin used to be the only first-line drug. But many people can’t tolerate 2,000 mg a day-nausea, bloating, diarrhea. Now, guidelines from the American Diabetes Association say: start metformin 1,000 mg with a low-dose SGLT2 inhibitor like empagliflozin 10 mg. Together, they drop HbA1c by 1.35%, just like the higher metformin dose. But GI side effects? Cut in half. And you get extra benefits: weight loss and lower heart failure risk.Cancer
In breast cancer, giving a lower dose of doxorubicin (60 mg/m²) with cyclophosphamide (600 mg/m²) works just as well as a higher dose of doxorubicin alone. But severe drops in white blood cells? Halved. Heart damage? Cut by more than two-thirds. That’s huge. Cancer treatment is brutal enough-reducing toxicity without losing effectiveness changes lives.Single Pills, Better Adherence
One big reason combination therapy works so well is simplicity. Instead of four separate pills, you take one. That’s called a fixed-dose combination (FDC). In a 2023 American Heart Association survey, 68% of patients took their FDC blood pressure pill regularly. Only 52% stuck with multiple pills. Why? “Easier to remember,” said 74% of them. No more mixing up which pill goes when. No more juggling different schedules. There’s even a famous example: the “polypill.” In India and parts of Europe, a single pill combines aspirin, a statin, and two blood pressure drugs-all at low doses. A major trial called UMPIRE followed 12,200 people without heart disease. Those on the polypill had 53% fewer heart attacks, 51% fewer strokes, and 49% lower death risk over five years. All from one pill, once a day.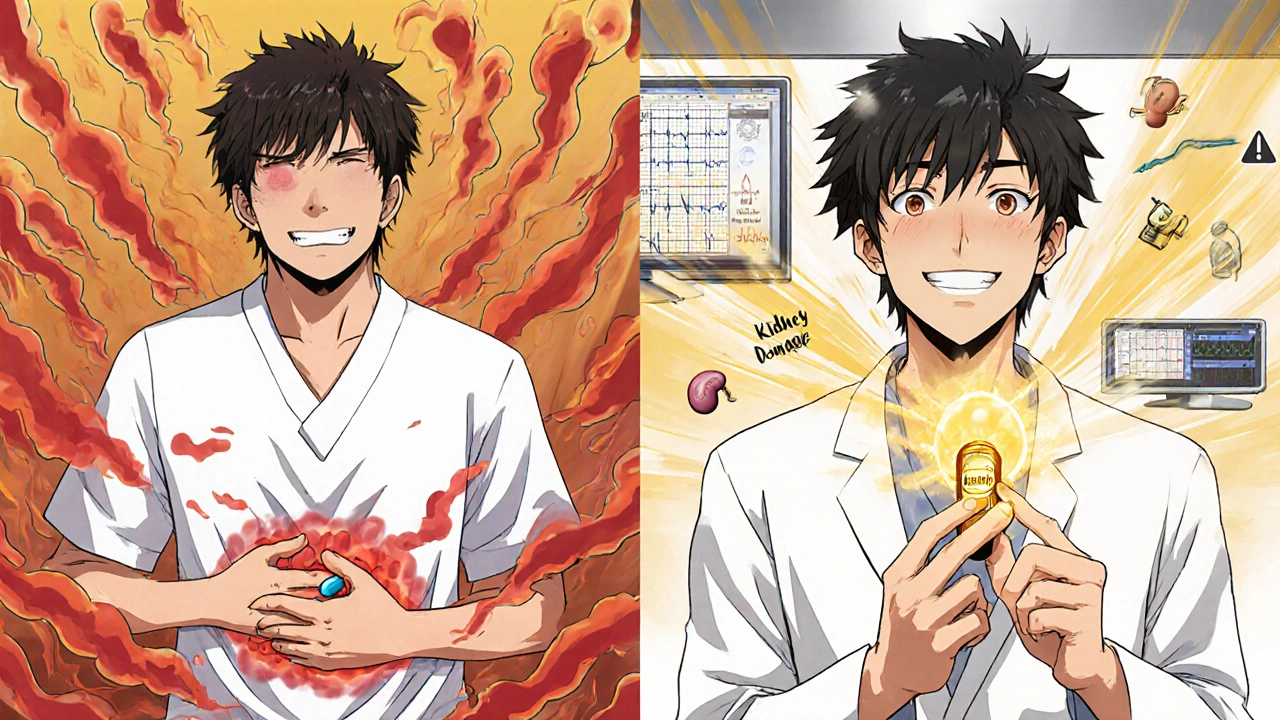
The Catch: When It Doesn’t Work
Combination therapy isn’t magic. It doesn’t work for everyone. Older adults with kidney problems are at higher risk. A 2022 study found that triple-drug combinations increased kidney injury risk by 80% in people over 75 with low kidney function. And in cancer, a 2023 Harvard study showed that nearly 4 in 10 approved drug combos had no real synergy-patients just got more side effects for no extra benefit. Cost is another issue. A combination pill can cost $4,200 a year versus $2,900 for a single drug. But here’s the twist: those extra costs are often offset. In diabetes, combination therapy cuts hospital visits, dialysis, and amputations so much that the net savings are $7,800 per patient per year. And then there’s the psychological hurdle. One in three patients on combination therapy quit within a year-not because it doesn’t work, but because they feel overwhelmed. “Too many pills,” they say on Reddit forums. Even if it’s one pill, they think: “I’m on five drugs now. I’m a pill-popping mess.”Who Should Consider This?
If you’re dealing with one of these, talk to your doctor about combination therapy:- You’ve tried one drug but still aren’t at target (blood pressure, HbA1c, cholesterol)
- You’re experiencing side effects from a single high-dose drug
- You’re on multiple medications already and want to simplify
- You’re newly diagnosed with high-risk hypertension, type 2 diabetes, or certain cancers
It’s not for everyone. If you’re stable on one drug with no side effects, there’s no need to change. But if you’re stuck between poor control and bad side effects, this might be your best shot.

What to Ask Your Doctor
Don’t just accept a combo prescription. Ask these questions:- Why this combination? What’s the science behind it?
- Are there fixed-dose options? (They’re cheaper and easier to take)
- What side effects should I watch for? (Some combos can cause unexpected interactions)
- How will we know if it’s working? (Regular checks-BP, HbA1c, kidney function-are key)
- What if I can’t afford it? Are there generics or patient assistance programs?
Pharmacists are your allies here. Many clinics now have medication therapy management programs where pharmacists review all your pills, check for interactions, and help you switch to FDCs. One 2023 study found this reduced adverse events by 28%.
The Future: Smarter, Lighter, Faster
Doctors aren’t stopping at two drugs. The American Heart Association now supports starting with four low-dose drugs for high-risk patients. And trials are testing five-drug combos at ultra-low doses-each at 20-30% of normal. Early results suggest we might cut heart disease risk by 70% with almost no side effects. There’s also a new idea: “response-adaptive sequencing.” Instead of giving you five drugs from day one, we start with one, see how you respond, then add the next only if needed. This could cut unnecessary drug exposure by 40% without losing effectiveness. The market is moving fast. In 2023, the FDA approved 47 new combination drugs-up from 32 the year before. By 2030, over 60% of new drug approvals are expected to be combinations.Bottom Line: Less Is More
Combination therapy isn’t about taking more drugs. It’s about taking smarter drugs. Lower doses. Better timing. Fewer side effects. More control. It’s not a new idea-it’s been proven for over 20 years. But it’s still underused. Too many doctors still start with one pill and wait until it fails. Too many patients think more pills = more danger. The truth? Sometimes, the safest and most effective way forward is to use less of each, together.Is combination therapy safe for older adults?
It can be, but it requires careful monitoring. For patients over 75 with kidney problems (eGFR below 45), triple-drug combinations can increase the risk of acute kidney injury by nearly 80%. Always start with two drugs, not three, and check kidney function every 4-6 weeks. Single-pill combinations with low doses are generally safer than stacking multiple separate pills.
Do combination pills cost more than taking drugs separately?
Yes, the upfront cost is often higher-about $4,200 a year versus $2,900 for a single drug. But many combination pills are now available as generics, bringing prices down. More importantly, they reduce hospital visits, complications, and emergency care. In diabetes, the net savings over a year can be over $7,800 per person. Insurance often covers FDCs fully if they’re medically necessary.
Can I switch from my current meds to a combination pill?
Possibly, but don’t switch on your own. Your doctor needs to check for interactions, adjust doses, and monitor your response. If you’re on two separate drugs and doing well, a combination pill might simplify your routine. But if you’re having side effects, switching to a combo might help. Always do it under medical supervision.
Are there any drug interactions I should worry about?
Yes. Combination therapy increases the risk of drug-drug interactions, especially in people taking five or more medications. For example, combining an ACE inhibitor with a potassium-sparing diuretic can raise potassium to dangerous levels. Always tell your doctor and pharmacist about every supplement, OTC drug, and herb you take. A medication review every 6 months is recommended.
Why aren’t more doctors using combination therapy?
Historically, doctors were trained to start with one drug and add others only if needed. That mindset is changing, but slowly. Some are worried about complexity, cost, or liability. Others don’t have time to explain it. But guidelines now strongly support it for hypertension, diabetes, and heart disease. If your doctor hasn’t mentioned it, ask. You’re more likely to stick with treatment if it’s simpler and safer.
Write a comment
Your email address will not be published.





11 Comments
Man i just took my blood pressure pill this morning and now i’m dizzy as hell. why the hell do docs keep pushing single high-dose crap when this combo thing works better???
Oh please. You think this is some revolutionary breakthrough? This has been standard in Europe for over a decade. Americans still think ‘more pills = more medicine’ like it’s 1998. Pathetic. And don’t even get me started on the polypill-India’s been doing it right while we’re still arguing over whether aspirin counts as a ‘real drug.’
so like… one pill for everything? 😍 i’m down. my meds drawer looks like a pharmacy exploded and i’m tired of playing doctor roulette. also… polypill? sounds like a superhero. i want to be the polypill man.
This is not just medicine. This is wisdom. Less is more. Simplicity is power. The body is not a machine to be overloaded. It is a symphony. When you play too many notes at once, the harmony breaks. But when you let each instrument play softly in perfect rhythm, the music becomes divine. This is how nature works. We must learn to listen.
Who the hell is paying for this? I’m on Medicare and my copay for one pill is already $80. Now you want me to pay $4200 a year for some fancy combo? And don’t tell me about savings-I’ve seen the bills. They don’t care about ‘net savings’ when your kidneys are failing and your Social Security check doesn’t cover insulin. This is just corporate greed in a fancy lab coat.
Let me be clear: this is not merely pharmacological innovation. It is a philosophical reorientation of medical authority. The hegemony of the high-dose paradigm has been rooted in a colonialist logic-force, control, dominance. The combination approach, by contrast, is collaborative, humble, and ecological. It acknowledges the body’s complexity rather than attempting to crush it under pharmacological tyranny. In South Africa, we know this truth intimately. Our people do not need more drugs. They need dignity. And this? This is dignity in a pill.
I’ve been on a combo for my diabetes for a year now. Honestly? I feel better than I have in a decade. No more nausea. I lost 12 pounds. My A1c is normal. And I don’t have to juggle five different bottles anymore. I just take one. Every morning. With my coffee. It’s… peaceful. I wish more people knew this was possible.
Let’s be real here. This whole combo thing is just a way for Big Pharma to extend patents and jack up prices. They take two generic drugs, slap them in one pill, call it ‘innovation,’ and charge triple. And now they’re pushing five-drug combos like it’s some kind of miracle? We’re turning medicine into a Russian roulette game with side effects. And don’t get me started on how many people quit because they’re overwhelmed. This isn’t progress. It’s manipulation dressed in white coats.
My dad’s 82 and has kidney issues. His doctor started him on a low-dose combo instead of three separate pills. Kidney numbers stayed stable. BP is under control. He doesn’t have to remember which pill is which. I’m just glad someone listened. Not every patient needs to be a medical expert to benefit from this.
You people are naive. This isn’t about science-it’s about control. The medical-industrial complex wants you dependent on pills. They don’t want you healing. They want you dosing. The polypill? A Trojan horse. One pill to rule them all. And you’re clapping like it’s a gift. Wake up. The real cure is diet, sleep, movement-not a chemical cocktail disguised as convenience.
As a pharmacist, I’ve seen this work. I’ve had patients cry because they finally stopped feeling sick. I’ve seen them switch from four pills to one and start taking them regularly. The science is solid. The adherence data is undeniable. The cost argument? Real-but so are the savings in ER visits and dialysis. Don’t dismiss this because it’s complex. It’s not magic. It’s medicine, done right.