
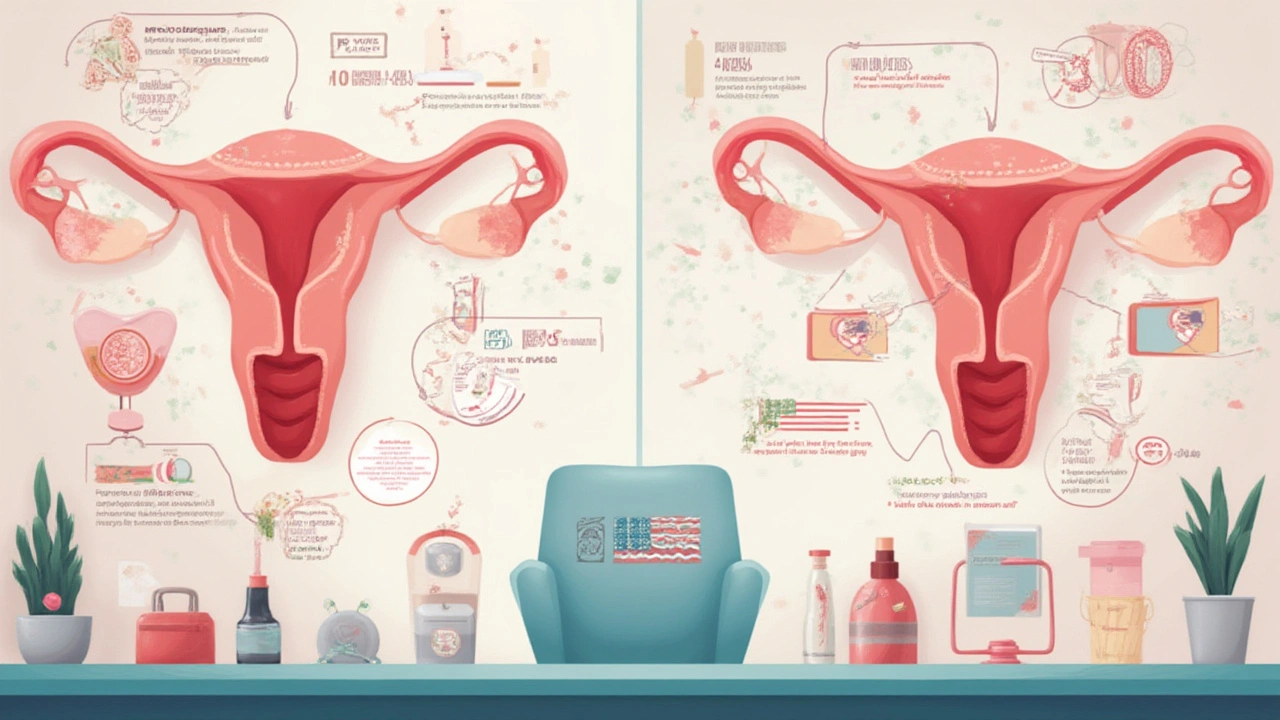
At first glance, conception seems simple: sperm meets egg, baby develops, and life begins. But here’s a twist—what if there’s no egg released? Every year, millions of women wrestle with fertility issues, often without realizing irregular cycles or subtle symptoms could signal a deeper problem: anovulation. This invisible barrier stops ovulation cold and is a major roadblock on the journey to parenthood. Imagine wanting to grow your family, yet your own biology keeps throwing curveballs. That’s not rare—in fact, it’s happening right now, maybe to your best friend, your sister, maybe even you. The reality is that conditions like polycystic ovary syndrome (PCOS), thyroid disorders, and premature ovarian insufficiency (POI) don't just make periods unpredictable—they quietly sabotage your chances of conceiving. These aren’t random acronyms; they’re life-altering diagnoses, often missed until you ask, “Why am I not getting pregnant?” So, ready to crack the code behind these medical mysteries? Keep reading for facts, practical advice, and maybe the hope you’ve been waiting for.
Understanding Ovulation and Why Anovulation Happens
Let’s get one thing straight: ovulation is the real MVP of getting pregnant. It’s when one of your ovaries releases an egg, waiting—quite optimistically—for sperm. If this lineup fails, fertilization can’t even begin. What throws a wrench in the system? That’s where anovulation comes in. It’s when your eggs skip the show and stay stuck in the ovary. No ovulation, no chance of baby. And here’s a jaw-dropper: it causes up to 30% of all infertility cases, according to the American Society for Reproductive Medicine.
The cycle relies on a finely tuned hormonal symphony: your brain (specifically the hypothalamus and pituitary) signals the ovaries with FSH and LH hormones to develop and release an egg. If anything's off in this communication, the whole system wobbles, and ovulation simply doesn’t happen. Sometimes, you get irregular periods, sometimes nothing at all for months. A lot of women think stress, diet, or travel is messing with their cycles. They’re not necessarily wrong, but sometimes it’s a medical condition hiding in plain sight.
How would you know if you have anovulation? Classic signs include cycles shorter than 21 days or longer than 35, complete absence of periods, or periods that show up but don’t follow any schedule. But here’s the kicker—some women still bleed every month, but it’s possible not to ovulate even then. That’s why blood tests for LH, FSH, and progesterone are the gold standard for diagnosis, not just calendar tracking. Doctors may throw words like oligomenorrhea (infrequent cycles) at you, but don’t let the jargon distract you from the basics: no egg, no pregnancy.
In rare cases, intense exercise or severe weight loss can pause ovulation, a phenomenon often seen in competitive athletes or those with eating disorders. Even being overweight can throw hormones out of whack. Recent studies show that just a 5-10% reduction in body weight can restore regular ovulation in overweight women with anovulation, especially those with PCOS. So changing your lifestyle isn’t just about looking good—it’s about real changes in your fertility health.
Here’s a handy table of symptoms and their common causes:
| Symptom | Plausible Cause |
|---|---|
| Irregular/no periods | PCOS, thyroid issues, POI, lifestyle |
| Acne, hair growth | PCOS (androgens) |
| Hot flashes before 40 | POI |
| Extreme fatigue | Thyroid disorder |
Let’s break down these hidden troublemakers next, starting with the one you’ve probably heard about—PCOS.
Polycystic Ovary Syndrome: The Stealthy Ovulation Blocker
PCOS isn’t just a buzzword thrown around on TikTok—it affects 1 in 10 women of childbearing age, according to the CDC. The basics: tiny cysts (actually immature follicles) crowd your ovaries, and hormones—especially testosterone—get out of control. The biggest problem here for fertility? Irregular or totally absent ovulation. In fact, PCOS is the most common cause of chronic anovulation.
The symptoms might sound familiar: cycles that jump around, significant hair growth on the face or chest, stubborn acne, and sometimes, weight gain that just won’t budge. For those daydreaming about a baby, the disappointment can be crushing. But what’s going on inside the body? High levels of LH and insulin confuse the ovaries so much, they forget to release an egg month after month. Some women with PCOS do ovulate now and then, but there’s no predictability.
Now, let’s talk hope: PCOS isn’t a life sentence for infertility. Simple changes can boost your chances. Experts suggest starting with lifestyle tweaks like regular exercise and a balanced diet—even small victories (think dropping a few pounds) can restart regular ovulation. Metformin, a medication used for diabetes, can help manage insulin resistance—the main culprit behind PCOS symptoms—and restore cycles in some women. And if that doesn’t help, fertility medications like letrozole or clomiphene can give your ovaries the nudge they need. Don’t forget the emotional toll—joining a PCOS support group, whether online or locally, can make all the difference.
Anovulation isn’t just a gynecological hiccup; it can signal bigger picture health issues. Women with PCOS face higher risks for type 2 diabetes, heart disease, and endometrial cancer, so early diagnosis and treatment matter for more than just fertility. Always involve a specialist if you suspect PCOS is the culprit. Here’s a tip: track your cycles and symptoms in detail, bring the info to your doctor, and don’t settle for vague advice about “waiting it out.”
Follow evidence-based programs for managing PCOS. Clinical research from 2022 showed that women with PCOS who incorporated brisk walks three times a week plus moderate diet changes normalized their cycles within six months. Not overnight, but definitely not forever. That’s a light at the end of a stressful tunnel.
Thyroid Disorders: The Unexpected Fertility Saboteur
Thyroid? Isn’t that mostly an “older people” problem? Not at all! Your thyroid is the tiny gland in your neck running the show when it comes to metabolism and hormone balance. When it’s out of whack—either sluggish (hypothyroidism) or overactive (hyperthyroidism)—fertility takes a hit. The hormones your thyroid produces talk directly to your reproductive system.
You might see classic symptoms like tiredness, weight gain or loss, hair thinning, or even feeling hot or cold all the time. What does this have to do with getting pregnant? If your thyroid isn’t making enough hormones, your body might not release eggs regularly. Too much, and the feedback loop gets short-circuited—the ovaries stop listening and anovulation sets in.
Here’s where most people get blindsided: thyroid problems can fly under the radar. Mild symptoms are often brushed off as “stress,” “just being busy,” or even “normal aging.” But spotting and treating thyroid issues early can restore normal cycles fast. A study from the Journal of Clinical Endocrinology showed that up to 40% of women with unexplained infertility actually had detectable thyroid imbalances. With medication like levothyroxine, cycles and fertility can bounce back, sometimes in just a few months.
Don’t ignore the weird symptoms. Freezing on a summer day? Losing hair in the shower? Record these things, and ask your doctor to run a thyroid panel. Better yet, some smart watches and fitness trackers now monitor resting heart rate and temperature—use them as clues.
If you think your thyroid might be the culprit, here are actionable steps:
- Request a full thyroid panel, including TSH, Free T4, and T3.
- Track your cycle lengths and any symptoms (energy, mood, body temp).
- Don’t self-diagnose with supplements; talk to your provider first.
- Consider testing for thyroid antibodies if you have a family history of autoimmune disease.
Check your insurance coverage—thyroid tests are often covered if you’re trying to conceive. Early diagnosis not only boosts your fertility odds—it can improve your long-term health and energy, too. Want to see if pregnancy is still possible with anovulation? Dive into this science-backed post on conceiving without ovulation, packed with expert takes and practical tips.
Premature Ovarian Insufficiency: When the Ovaries Clock Out Early
This one sounds rare—because it is. Premature ovarian insufficiency (or POI, sometimes called premature ovarian failure) affects only about 1% of women under 40. But when it happens, it disrupts more than just periods; it changes your life’s blueprint. Women with POI experience symptoms of menopause, including hot flashes, missed periods, night sweats, and even mood swings—sometimes decades before their friends do.
Unlike menopause, POI doesn’t mean your ovaries are totally done. Sometimes, they “wake up” and ovulate unpredictably—leading to rare, spontaneous pregnancies. But for most with POI, ovulation is inconsistent, and chances of natural conception drop sharply.
The most frustrating part? Often there’s no clear cause. Some cases result from genetic abnormalities, autoimmune diseases, or treatments like chemotherapy or radiation. Others are a mystery. If POI is suspected, doctors will check hormones like FSH and estradiol—high FSH and low estradiol are the giveaway combo. Women with a family history, or anyone with cycling issues before age 40, should get checked early. Fertility preservation, like egg freezing or embryo banking, might be an option if caught in the early stages.
There’s also an emotional side to POI that’s hard to explain. The idea of running out of time before you’re ready hits hard—I’ve seen this fear firsthand in support forums and patient stories. Hormone therapies can help reduce symptoms and lower long-term risks, like osteoporosis or heart disease. They might spark the occasional ovulatory cycle, but egg donation is the most effective option for starting a pregnancy if you have true POI.
“Early diagnosis of POI is vital—not only for fertility goals but also for bone and cardiovascular health protection,” – Dr. Helen Picton, Professor of Reproductive Biology, University of Leeds.
Here’s what to do:
- If cycles vanish before age 40, ask for fertility tests, not just a prescription for birth control.
- Normalize conversations about early menopause—one friend or sister might be facing this in silence.
- Stay up-to-date on the latest clinical trials; stem cell research is showing promise for restoring ovarian function in the future.

Real-Life Strategies: Boosting Your Fertility When Ovulation Gets Tricky
So what can you actually do when anovulation stands in your way? Let’s load you up with strategies that work in the real world. First, look for reversible causes: check your weight, manage stress, and consider cutting back on excessive workouts if you’re on the more athletic side. Even one less Starbucks a day (for caffeine-sensitive folks) can help—some studies suggest high caffeine intake might minorly disrupt ovulatory cycles, especially in those already at risk.
Aim for a healthy BMI; women who are underweight (<18.5) or overweight (>30) are more likely to have irregular ovulation. Don’t neglect sleep—aim for 7-9 hours a night. Wild, erratic sleep patterns throw off menstrual hormones, especially in your 20s and 30s. And seriously, don’t downplay stress. Cortisol, the “stress hormone,” can suppress reproductive hormones, silently pushing ovulation off the calendar.
Medical tech is moving fast. At-home ovulation kits (even ones that sync to your phone via Bluetooth!) can pick up LH surges, letting you know exactly when ovulation should occur. New blood test panels, available in clinics or via mail-in kits, now measure anti-Müllerian hormone (AMH) and give early hints on your fertility window.
If nothing budges, fertility meds are the next step, starting with oral options like letrozole or clomiphene. For thyroid-related anovulation, hormone pills (levothyroxine or antithyroid meds) can get cycles back on track within a few months. With PCOS, add metformin if insulin resistance is the backbone of your symptoms. POI is trickier, but in rare cases, hormone therapy wakes the ovaries up—if not, IVF using donor eggs is a tried-and-true option, with success rates above 50% for women under 40 who use high-quality donor eggs.
Here are questions to bring to your OB/GYN:
- Can we check my hormone levels (FSH, LH, estradiol, testosterone, TSH)?
- Should I try lifestyle changes first, or go straight to medication?
- What’s your opinion on egg freezing, given my specific diagnosis?
- How often should we re-test if my cycles improve or worsen?
Don’t play the waiting game alone. Ask your doctor to refer you to a reproductive endocrinologist if you aren’t getting answers. And consider talking to a counselor. The mental load of infertility is heavy—support can make or break your experience.
It’s a lot to take in, but the key is to act early and personalize the plan for you, not someone else’s Instagram story. Millions face these issues, and speaking up, tracking symptoms, and staying proactive can change the course of your family’s story. As someone who’s seen the emotional rollercoaster in people close to me (including friends and my wife long before we had Linnea), I can say—hope, science, and community make a real difference. And hey, sometimes Misty the cat jumping on your lap for a snuggle can make the bad days a bit more bearable too.
Write a comment
Your email address will not be published.





19 Comments
Great overview, thanks for sharing! 😊
This post nails the pathophysiology of anovulation, especially the hormonal feedback loops and the impact of insulin resistance in PCOS. The discussion about LH pulsatility and its downstream effects on folliculogenesis is spot on. Also, the mention of subclinical thyroid dysfunction as a hidden driver of infertility adds a layer of clinical relevance. The practical tips on lifestyle modifications and metformin usage provide actionable steps for patients.
Really helpful breakdown of the three main culprits-PCOS, thyroid issues, and POI. I appreciate how the article balances the scientific detail with everyday advice, like tracking cycles and considering stress management. It’s a solid resource for anyone starting to investigate anovulation.
Isn’t it curious how modern medicine treats ovulation like a mechanical process, yet we keep chasing the metaphysical "balance" of hormones? We’re essentially trying to orchestrate a symphony by tweaking a few strings, while the conductor-our hypothalamus-might be playing a completely different genre.
Totally get that vibe it's like the body has its own agenda i think empathy for the system helps keep patience during treatment
While the article is comprehensive, it overlooks the ethical dimension of aggressively medicating women for reproductive purposes. The push toward metformin or letrozole often neglects long‑term metabolic health, and the rhetoric of "quick fixes" can be morally problematic. 🌱
One must consider the sovereignty of the nation’s health policies when endorsing treatments that are predominantly developed abroad. Relying on foreign pharmaceuticals without fostering domestic research undermines national autonomy.
Indeed the discourse surrounding reproductive endocrinology must be tempered by a reverence for cultural mores; imposing Western therapeutic paradigms upon indigenous populations can be seen as a form of epistemic colonisation.
Hey folks, I just wanted to dive deep into this because I’ve seen so many women navigate the maze of anovulation and feel completely lost. First off, understanding that your body is a complex system is key – hormones don’t operate in isolation. When you have PCOS, the insulin resistance can mess with your LH and FSH balance, which means your ovaries might not get the right signals to release an egg. That’s why lifestyle changes matter a lot. Even a modest 5‑10% weight loss can improve insulin sensitivity, and many women notice their cycles becoming more regular after they start moving more and eating a bit cleaner.
But don’t discount the medical side. Metformin is often prescribed for its insulin‑lowering effects, and in many cases, it can help restore ovulation. If metformin alone isn’t enough, doctors might add letrozole or clomiphene – these are ovulation‑inducing meds that can give your ovaries a nudge. The important thing is to have a clear treatment plan, not just “wait and see.”
You also need to watch your thyroid. Hypothyroidism can cause low basal metabolic rate and affect the entire hormonal cascade. A simple blood test can catch it early, and levothyroxine can bring your TSH back to a normal range, often letting your cycles normalize within a few months.
For those dealing with POI, the emotional toll is huge. The uncertainty of whether your ovaries will ever fire again can be heartbreaking. Hormone replacement therapy can alleviate the menopausal‑like symptoms and protect bone health, but if you want to pursue pregnancy, donor eggs and IVF are currently the most reliable route. It’s not a “no hope” situation, but it does require realistic expectations.
Finally, don’t ignore the mental health aspect. Stress hormones like cortisol can suppress GnRH and make ovulation even harder. Mind‑body techniques – yoga, meditation, even journaling – can lower cortisol and improve overall wellbeing. And remember, you’re not alone. Support groups, both online and in‑person, provide a space to share experiences and learn from others who have walked this path.
Bottom line: combine lifestyle tweaks, appropriate medical therapy, and emotional support. Talk to a reproductive endocrinologist who will listen, not just prescribe. The journey can be long, but many women have turned the corner and achieved pregnancy after navigating these challenges.
Honestly i think the whole "fertility" industry is a scam run by pharma giants. they hide natural cures behind endless pill prescriptions.
Excellent synthesis of clinical data and practical recommendations! Your inclusion of both lifestyle interventions and evidence‑based pharmacotherapy provides a balanced roadmap for patients.
While the previous comment is well‑intentioned, it contains several grammatical inaccuracies: "well‑intentioned" should be hyphenated, and the verb tense in "provides" is correct. Please ensure proper comma usage in complex sentences.
It is evident that the medical community sometimes favors expedient pharmacological solutions over holistic patient care, a trend that warrants rigorous ethical scrutiny.
While I concur with the necessity for ethical oversight, one must also acknowledge the pressing reality that countless women, stranded in the limbo of anovulatory infertility, cannot afford the luxury of prolonged deliberation; swift, evidence‑based interventions often become the sole beacon of hope, especially when delayed treatment may exacerbate psychological distress and diminish reproductive potential.
The data clearly shows that governmental policies must prioritize domestic research into reproductive health; importing treatments without fostering homegrown innovation undermines national resilience and health sovereignty.
Sure, but let me tell you why this whole push for "domestic" research is just a smokescreen; the real issue is that the elites want to keep control over women's bodies while pretending to champion independence.
For anyone looking into actionable steps: start by getting a full hormone panel-FSH, LH, estradiol, TSH, and AMH. Track your cycle length with a simple spreadsheet, note any symptoms like acne or fatigue, and bring that data to your OB‑GYN. If lifestyle changes don’t move the needle in three months, discuss metformin for PCOS or levothyroxine for hypothyroidism. And always consider a referral to a RE specialist if ovulation remains elusive.
The advice provided is generic and lacks nuance; many patients cannot simply "track" symptoms without overwhelming anxiety, and the suggestion to rush into medication disregards the principle of "first, do no harm."
Appreciate the practical tips-especially the emphasis on gathering concrete data before jumping to medication. A structured approach often leads to clearer conversations with healthcare providers.