Every year, hundreds of thousands of patients experience unexpected side effects, device malfunctions, or product failures with medications, medical devices, or even dietary supplements. But most never report them. If you’ve had a bad reaction to a drug, noticed a faulty insulin pump, or found your baby formula had foreign particles in it, you’re not alone-and you can help protect others by filing a direct report with the FDA.
What counts as a reportable issue?
You don’t need to be a doctor or a scientist to know when something’s wrong. The FDA accepts reports for three main types of problems:- Serious adverse reactions-like hospitalization, life-threatening events, birth defects, or permanent disability linked to a product.
- Product quality issues-contaminated pills, broken device parts, expired products, or mislabeled packaging.
- Therapeutic failure or use errors-a diabetes drug that stops working, a pacemaker that misfires, or a patient using a device incorrectly because instructions were unclear.
Even if you’re not sure it’s serious, report it. The FDA doesn’t require proof-just your experience. In fact, many safety alerts start with just a few patient reports. One example: in early 2024, 287 patients reported insulin pens not working properly after being stored in hot cars. That led to a nationwide safety notice.
How to file a report: 4 ways to submit
The FDA gives you several options. Pick the one that works best for you.- Online via the Safety Reporting Portal (SRP)-This is the fastest method. Go to fda.gov/safety/reporting-problems-fda and fill out the form. It takes 15-20 minutes. You’ll need: product name, lot number, expiration date, your symptoms, when they started, and what other meds you take.
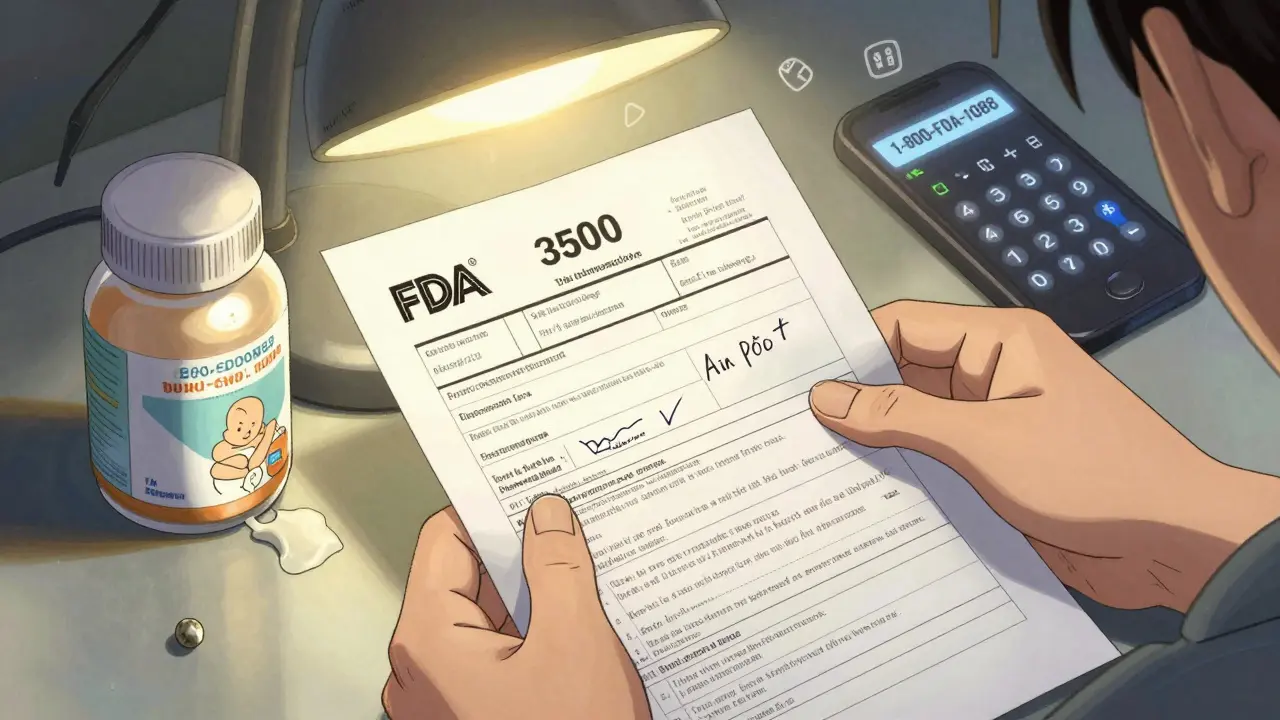
- Print and mail the FDA 3500 form-Download the PDF from the FDA website. Fill it out by hand or type it in. Mail it to: MedWatch, 5600 Fishers Lane, Rockville, MD 20852. This is a good backup if the online portal crashes-which it still does often. Since August 2024, users have reported repeated system failures.
- Call 1-800-FDA-1088-If you’re not comfortable typing or have trouble reading the form, call. Representatives are available Monday through Friday, 8 a.m. to 8 p.m. Eastern Time. They’ll take your report over the phone and mail you a form to sign.
- Use the Spanish version (FDA 3500B)-If you’re more comfortable in Spanish, use the bilingual form. It’s identical to the English version but written in Spanish. No other languages are officially supported yet.
Pro tip: If you’re reporting a medical device, write down the lot number and expiration date. They’re usually on the packaging or the device itself. But here’s the hard truth: only 62% of consumer-packaged devices have these details printed clearly. If you can’t find them, write “unknown” and describe where you bought it.
What information do you need?
You don’t need a medical degree, but you do need basic details. The FDA asks for:- Your age, sex, and weight (optional but helpful)
- The name of the product (brand and generic if you know it)
- Lot number and expiration date (if available)
- When the problem started and how long it lasted
- A clear description of what happened (e.g., “My heart started racing after taking the new blood pressure pill”)
- Any other medicines or supplements you were taking
- Whether you went to the doctor or hospital
- Your contact info (so they can follow up if needed)
Don’t worry if you don’t have all the details. The FDA says most patient reports are incomplete-but still valuable. In fact, a 2023 study found patient reports included 37% more detail about symptom timing than doctor-submitted ones. Your lived experience matters.
Why your report matters
Clinical trials test drugs on 500 to 3,000 people. But once a drug hits the market, millions use it. That’s when rare side effects show up-like one in 10,000 or even rarer. These are invisible to trials but visible to you.Patient reports have directly led to:
- Stronger warnings on antidepressants about suicidal thoughts in teens
- Recalls of faulty glucose monitors that gave false readings
- Changes in how insulin pens are labeled after patients reported confusion
And it’s not just drugs. In 2024, patient reports were 2.3 times more likely than provider reports to identify new ways people were misusing medical devices-like using a nebulizer with the wrong solution or wearing a continuous glucose monitor under a tight sleeve.
What the FDA does with your report
Your report goes into the FDA Adverse Event Reporting System (FAERS), a database with over 25 million reports dating back to 1969. About 15-20% of those come from patients like you.Here’s what happens next:
- Trained analysts review your report for patterns. If 10 other people report the same issue with the same product, it gets flagged.
- If the signal is strong enough, the FDA may issue a safety alert, update product labels, or even pull the product off the market.
- They may contact the manufacturer to investigate.
Processing used to take 15-30 days. Now, thanks to a new AI system launched in late 2024, the initial review takes just 9 business days. The FDA aims to cut that to 5 days by the end of 2026.
What won’t work
Some people think they should call their doctor or the drug company first. That’s not enough. Manufacturers are required to report problems to the FDA-but they often delay, downplay, or bury them. Your direct report bypasses that middleman.Also, don’t wait for confirmation that it’s “serious enough.” The FDA says: if you’re worried, report it. You don’t need to be certain. They’ll sort it out.
And no, you won’t get a response unless they need more info. That’s normal. Most reports are anonymous and used for trend analysis, not individual follow-up.
Common problems patients face
The system isn’t perfect. Here’s what users report:- The portal crashes-Since August 2024, users have had repeated issues logging in or submitting forms. The FDA admits this. If it fails, use the phone or mail.
- Lot numbers are missing-Only 62% of products list them clearly. If you can’t find it, write “unknown” and note where you bought it.
- Medical terms are confusing-Don’t guess. Use plain language: “I felt dizzy,” not “I experienced orthostatic hypotension.” The FDA’s new symptom wizard (released in late 2024) helps with this.
- Most people don’t know they’re protected-Your name and contact info are confidential under FDA rules. They can’t share it without your permission. But 68% of patients don’t know this.

What’s changing in 2025 and beyond
The FDA is working on big upgrades:- Next Generation Safety Reporting System (NGSRS)-Launched in January 2025, this new system automatically checks lot numbers and uses AI to code symptoms faster.
- Multilingual support-By 2027, the FDA plans to add reporting in Spanish, Mandarin, French, Vietnamese, and Tagalog.
- One portal for everything-Right now, you need different forms for drugs, devices, and supplements. By 2028, they plan to merge all reporting into one system.
Also, companies like Medtronic are now letting patients report directly through their apps. That’s a big step forward.
What to do after you file
After you submit:- You should get a confirmation email within 5 business days-if you gave an email address.
- Keep a copy of your report or the mailing receipt.
- If you have follow-up symptoms, keep notes. You may be asked later.
- Don’t expect a call or update. Most reports are used for trends, not individual cases.
And if you’re still unsure? Call the FDA’s help line: 1-800-FDA-1088. They answer 92% of calls during business hours.
Why this isn’t just a form-it’s a tool for change
You might think, “One report won’t make a difference.” But think about it: every major safety alert started with one person saying, “This isn’t right.”That’s how the FDA found the link between a popular migraine drug and heart valve damage. That’s how they learned some insulin pumps were failing in cold weather. That’s how they fixed instructions for a pediatric asthma inhaler after parents reported kids choking on the mouthpiece.
Your voice isn’t just heard. It’s used to protect millions.
Can I report a problem with a dietary supplement or cosmetic?
Yes. The FDA accepts reports for dietary supplements, cosmetics, infant formula, and tobacco products. Just use the same FDA 3500 form or online portal. These products aren’t approved before sale, so patient reports are often the first warning sign of contamination or dangerous ingredients.
Do I need to tell my doctor before reporting to the FDA?
No. You don’t need permission or a doctor’s note. In fact, many patients report because their doctor didn’t take their symptoms seriously or didn’t know how to file. Your report is independent and confidential.
What if I don’t remember the product name?
Describe it as best you can: color, shape, packaging, where you bought it, or what condition it was for. The FDA can often identify it using your description and date of use. If you still have the bottle or box, take a photo and keep it.
Will my report lead to a recall?
Not usually on its own. Recalls happen only after many reports show a clear pattern. But your report helps build that pattern. Even one report can trigger an investigation that leads to a recall later.
Is there a deadline to file a report?
There’s no strict deadline for patients. The FDA recommends reporting within 15 days for serious events, but reports filed months or even years later are still reviewed. The sooner you report, the better-but it’s never too late.
Can I report anonymously?
Yes. You can leave your name and contact info blank. But if you want a confirmation email or if the FDA needs to follow up, you’ll need to provide it. Your identity is protected by law and won’t be shared without your consent.
What if I report and nothing happens?
That’s normal. Most reports don’t lead to immediate action. But they’re added to a growing database. One report might not change anything-but 500 like it can. Your report contributes to the bigger picture of drug and device safety.
Are patient reports taken seriously compared to doctor reports?
Yes, but differently. Doctors provide clinical details; patients provide real-world context. The FDA values both. Patient reports are especially valuable for spotting misuse, off-label use, and symptoms that don’t show up in clinical trials.
Write a comment
Your email address will not be published.





4 Comments
I filed a report last year after my insulin pump stopped working during a hike. No response, no call, just a confirmation email. But I know it went somewhere. Keep doing it.
It matters.
The real win here isn’t the form-it’s the mindset shift. We’ve been trained to think doctors are the only ones who can speak for us. But the FDA doesn’t need a medical degree to understand pain, confusion, or fear. Your story is data. Your voice is a signal. And right now, the system is listening more than it ever has.
Don’t wait for permission to speak up.
The AI-driven triage system launched in Q4 2024 has significantly improved signal detection velocity in FAERS. Patient-submitted reports now contribute 18.7% of Class I recalls, up from 12.3% in 2022. The NGSRS integration with structured ontologies (SNOMED CT, MedDRA) is accelerating symptom coding by 40%.
Still, the 62% lot number visibility gap remains a systemic failure in consumer packaging compliance. Manufacturers need to be held accountable for legible labeling under 21 CFR 801.15.
So let me get this straight-I’m supposed to spend 20 minutes filling out a form that crashes half the time, just so some bureaucrat in Rockville can add my story to a 25-million-entry graveyard? And you call this 'change'?