
INR Safety Checker
INR Safety Checker
Check if your INR is within safe therapeutic range based on your medical condition. This tool provides guidance on what action to take if your INR is outside your target range.
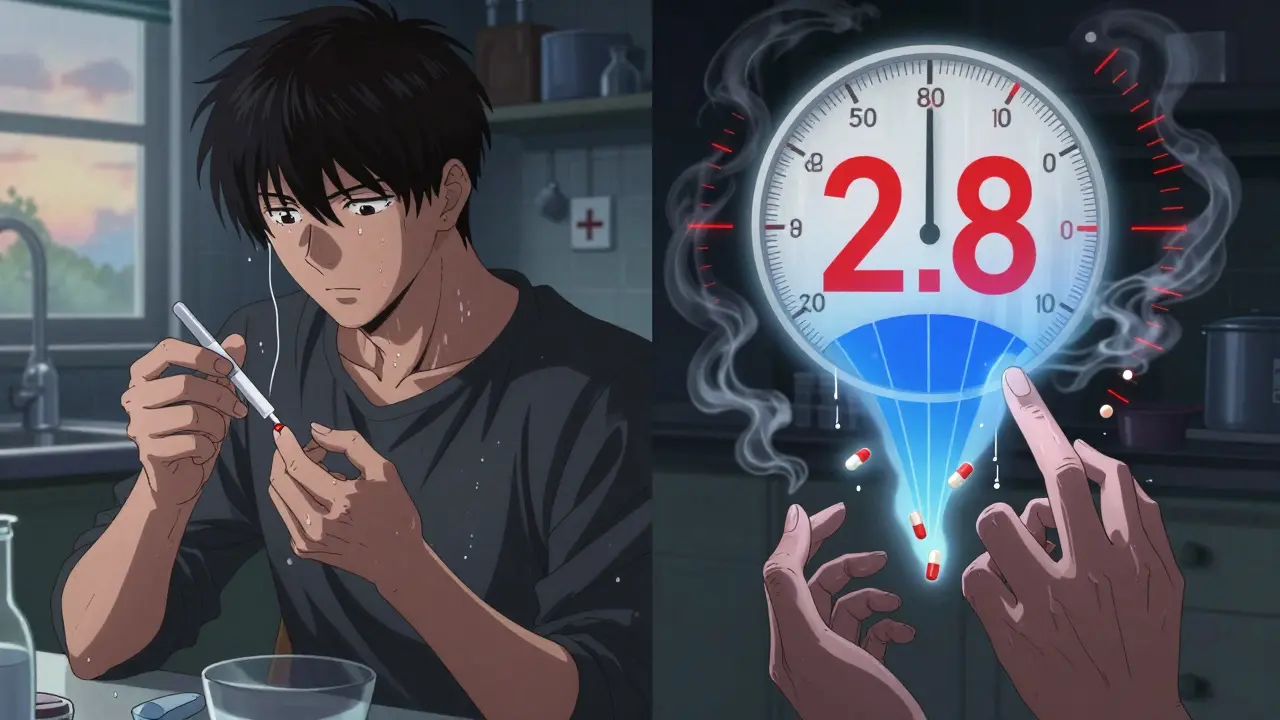
When you're on a blood thinner like warfarin, your life doesn't revolve around pills - it revolves around a number: your INR. It's not just a lab result. It's the difference between staying safe at home and ending up in the ER with internal bleeding. Or worse - having a stroke because your blood is too thick. This number tells your doctor if your medication is working just right. Too low? Clots form. Too high? You bleed. And that narrow window? It’s smaller than most people realize.
What Is INR, Really?
INR stands for International Normalized Ratio. It’s a standardized number that tells doctors how long it takes your blood to clot. Before INR existed, every lab used different reagents to test blood clotting time. One hospital’s ‘normal’ could be completely different from another’s. That meant a patient moving between clinics could get dangerously wrong doses. The WHO created INR in 1983 to fix that. Now, whether you’re tested in New York or Nebraska, an INR of 2.5 means the same thing everywhere.
The test starts with a simple blood draw - or sometimes a finger prick if you’re using a home monitor. The machine measures how long it takes your plasma to clot after adding tissue factor. That time gets plugged into a formula that adjusts for the specific reagent used in the test. The result? A clean, universal number. For someone not on blood thinners, INR is always 1.0. For you? It’s likely between 2.0 and 3.0 - but that’s not set in stone.
Your Target INR: It Depends on Why You’re on Blood Thinners
Not everyone on warfarin has the same goal. Your target INR isn’t chosen randomly. It’s based on your condition.
- If you have atrial fibrillation or a deep vein thrombosis, your target is usually 2.0 to 3.0.
- If you have a mechanical mitral valve, you need a tighter, higher range: 2.5 to 3.5.
- For a mechanical aortic valve, it’s still 2.0 to 3.0 - but your doctor might adjust it based on your age, other conditions, or the exact type of valve you have.
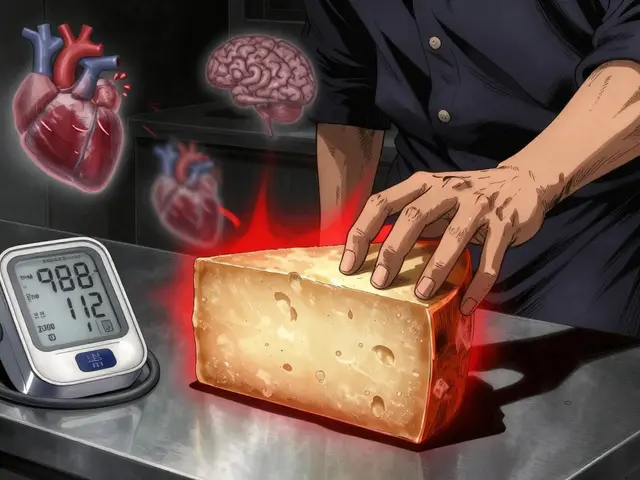
These ranges aren’t guesses. They come from decades of clinical trials showing what reduces strokes and clots without causing too much bleeding. Going above 3.0? Your risk of major bleeding jumps 27% for every 0.5-point increase. Dropping below 2.0? Your risk of stroke goes up by nearly half. That’s why hitting your target matters more than you think.
Why Home Testing Is Changing the Game
Going to the lab every week for a blood test is exhausting. Waiting two days for results? Stressful. Many people now use home INR monitors - small devices that use just a drop of blood from your finger. Devices like the Abbott Acelis or Roche CoaguChek give you results in under a minute. No more scheduling, no more waiting, no more missing work.
And it works. Studies show people who test at home stay within their target range 72% of the time. Clinic-based patients? Only 58%. That difference means 34% fewer clots and 21% fewer major bleeds. The FDA approved these devices in 2017, and since then, they’ve become standard for stable patients.
But it’s not for everyone. If you have shaky hands, poor eyesight, or trouble remembering steps, home testing can be risky. About 25-30% of patients aren’t good candidates. Training takes 2-4 sessions with a nurse to learn how to prick your finger correctly, load the strip, and report results. One user on Reddit said, “After three years, I still miss the tube one in five times - and each strip costs $6.” That adds up.
Cost, Insurance, and What You Really Pay
Warfarin itself costs about $4 a month. That’s cheap. But the monitoring? That’s where the bill piles up.
A home monitor costs around $299 upfront. Each test strip runs $5.99. Medicare Part B covers 100% of the cost for eligible patients - no deductible, no copay. Private insurance? Usually covers it too, but you might pay 20% coinsurance. Annual out-of-pocket caps can hit $7,500. And yes - 31% of patients get denied at first. You’ll need your doctor to appeal.
Compare that to DOACs like apixaban or rivaroxaban. They don’t need INR checks. But they cost $550-$650 a month. For many, especially older adults on fixed incomes, warfarin with home testing is still the most affordable option. Especially if you have a mechanical valve - DOACs don’t work for those.
What Happens When Your INR Is Off?
INR below 1.5? That’s dangerous. Your blood isn’t thin enough. You’re at risk for clots - heart attack, stroke, pulmonary embolism. Call your doctor immediately.
INR above 4.9? Major bleeding risk skyrockets. Above 5.0, you should skip your next warfarin dose and call your provider within 24 hours. If you’re dizzy, bruising easily, or have blood in your urine or stool - go to the ER. Don’t wait.
Here’s the reality: most people don’t panic over a single high or low reading. One bad number doesn’t mean disaster. But if your INR is consistently out of range for weeks, your doctor will adjust your dose. Sometimes, it’s as simple as skipping a pill. Other times, you need vitamin K or a blood transfusion.
When You Should Test - And When You Shouldn’t
Testing too often doesn’t help. Testing too rarely is dangerous.
When you first start warfarin? You might test twice a week. Your dose is being fine-tuned. Once you’re stable? Monthly is enough - unless something changes. New meds? Antibiotics? Diet changes? Travel? Weight gain? Then test sooner. The American College of Physicians found that 38% of patients get tested weekly even when they’re stable. That’s unnecessary stress and cost.
Time of day matters too. Test between 8 a.m. and 12 p.m. Fasting for 4-6 hours before helps keep results consistent. Don’t test right after a big meal or when you’re dehydrated. Even alcohol can throw off your INR. And if you’re on vacation? Bring your monitor. Don’t skip a test.
Warfarin vs. Newer Blood Thinners: The Trade-Off
There’s a reason DOACs (direct oral anticoagulants) are now the first choice for most people. No INR checks. No dietary restrictions. Fewer drug interactions. They’re easier. And safer - for most.
But here’s what you won’t hear in ads: DOACs don’t work for everyone. If you have a mechanical heart valve, you must stay on warfarin. If you have severe kidney disease, DOACs can build up to toxic levels. And if you’re on Medicaid or Medicare with no extra drug coverage? Warfarin is the only realistic option.
Also, DOACs can’t be reversed easily if you bleed. Warfarin can be reversed with vitamin K or fresh plasma. That’s a big deal for older patients or those with fall risks.
So it’s not about which is better. It’s about which is right for you.

What the Experts Say - And Where They Disagree
Dr. Jack Ansell, a leading hematologist, says maintaining your INR within 10% of your target reduces stroke risk by 60%. That’s huge. The American Heart Association found hospitals with over 65% time in therapeutic range (TTR) had 42% fewer clots than those below 50%.
But not everyone agrees on how often to test. Dr. Amir Qaseem from the American College of Physicians says: “Stable patients don’t need weekly tests.” Yet many clinics still order them out of habit. And the FDA found that 12% of home devices give inaccurate readings above INR 4.0. That’s a real danger.
Telehealth is helping. 78% of anticoagulation clinics now use remote monitoring. Patients miss fewer appointments. Adherence jumped from 76% to 92% with text reminders and automatic result uploads. That’s the future - but it’s not available everywhere.
The Bigger Picture: Who’s Left Behind?
Home INR testing is a win - but only if you can access it. Rural areas? Only 35% of clinics offer full anticoagulation management. Urban centers? 82%. That gap means rural patients are more likely to have dangerous INR swings.
Seniors over 65? Only 3.1 out of 5 satisfaction with home testing, mostly because of vision or dexterity issues. Younger patients? 4.3 out of 5. And for people with mechanical valves? They’ll pay more, drive farther, and test more often - because they have no choice.
The market for INR devices is growing fast - projected to hit $2.14 billion by 2028. But growth doesn’t mean equity. Until access is universal, the people who need it most will keep falling through the cracks.
What You Can Do Today
Don’t wait for your next appointment to understand your INR. Ask your doctor:
- What’s my exact target range - and why?
- Am I a candidate for home testing?
- Does my insurance cover it? What’s the process to get approved?
- What should I do if my INR is too high or too low?
- Are there any new meds, supplements, or foods I should avoid?
Keep a log. Write down your INR, your dose, what you ate, and how you felt. Patterns matter. If your INR keeps dipping after eating kale or spinach, your doctor can adjust your dose - not your diet.
And if you’re on home testing? Practice your finger prick. Don’t be afraid to ask your nurse for help. One wrong test can cost you $6 - and more importantly, it can make you lose confidence. You’ve got this. But you don’t have to do it alone.
INR isn’t just a number. It’s your lifeline. Get it right - and you live longer. Get it wrong - and everything changes in seconds.
Write a comment
Your email address will not be published.



6 Comments
Man, I wish I'd known all this when I first started on warfarin. Home testing was a game-changer for me - no more waiting two days for results while my anxiety spiraled. I keep a little notebook now: INR, dose, what I ate, even how much coffee I drank. Turns out my INR dips every time I have a big spinach salad. My doc adjusted my dose instead of telling me to quit eating greens. Best advice? Don't be afraid to track patterns - your body talks, you just gotta listen.
And yeah, strips cost a fortune, but compared to an ER visit? Worth every penny.
Let me guess - the FDA approved these devices because Big Pharma wanted to keep you hooked on warfarin and make you pay for strips forever. Did you know the same companies that make the monitors also manufacture the blood thinners? Coincidence? I think not. And don’t get me started on how they ‘adjust’ the formula to make INR seem more volatile than it really is - they want you scared, so you keep testing, keep buying, keep dependent.
Meanwhile, vitamin K2 supplements can stabilize your INR naturally - but you won’t hear that from your doctor. Why? Because supplements don’t have patent numbers.
Wake up. This isn’t medicine. It’s a revenue stream.
Oh, how utterly charming - Americans treating their blood like a spreadsheet. We in the UK have been managing anticoagulation since the 1950s without needing a $300 gadget and a PhD in finger-pricking. You Americans turn every medical necessity into a tech product with a subscription model. How quaint.
My mum’s on warfarin, lives in rural Wales, and gets her blood drawn once a month at the local clinic. No strips, no panic, no ‘home monitoring.’ Just a nurse, a vial, and a cup of tea. We don’t need to ‘optimize’ our clotting - we just need competent healthcare.
Stop glorifying consumerism disguised as innovation. You’re not ‘empowered’ - you’re being exploited.
Okay but seriously - who lets their doctor just say ‘2.0 to 3.0’ without explaining WHY? I had a guy on my team who thought his INR was ‘just a number’ until he had a mini-stroke. Turns out his target was 2.5 because of his mechanical valve - but no one ever told him the difference between ‘2.0’ and ‘2.5’ was the difference between walking into work and being carried out in a stretcher.
And don’t even get me started on people who skip tests because ‘they feel fine.’ Feeling fine doesn’t mean your blood isn’t turning to concrete. Your body doesn’t send notifications when you’re one pill away from disaster.
Stop treating your INR like a suggestion. It’s your life’s thermostat.
The entire premise of INR management is a statistical illusion. The ‘target ranges’ are derived from population averages, not individual physiology. You’re being told your INR must be 2.5 - but your clotting cascade may operate optimally at 2.1 or 2.9. The system doesn’t care. It’s a one-size-fits-all algorithm designed for efficiency, not biology.
And home monitors? They’re calibrated using the same reagents as the labs - meaning they’re measuring the same flawed proxy. The real variable is not your INR - it’s your doctor’s willingness to think beyond the number.
There is no ‘therapeutic range.’ There’s only your body, your meds, and a system that refuses to listen.
So let me get this straight - you’re telling me I can spend $6 every time I poke my finger to avoid a stroke… but if I don’t, I might die? And the alternative is a pill that costs $20 a day but doesn’t need testing? Huh. So… we’re paying for convenience or for survival? Either way, I’m paying.
At least with warfarin, I get to feel like a scientist. I’m not just swallowing a pill - I’m managing a system. It’s weirdly empowering. Like being the pilot of your own blood.
Also - kale is a traitor. I swear it’s sabotaging me.