
Sick Day Medication Advisor
How to Use This Tool
Answer the questions below to get personalized guidance based on the latest ADA guidelines. This tool will help you determine if you should stop or continue specific diabetes medications when sick.
When you’re sick with a cold, flu, or stomach bug, your body is under stress. For people with diabetes, that stress can turn a minor illness into a medical emergency. The wrong move with your diabetes meds-like skipping a dose or keeping one you shouldn’t-can trigger diabetic ketoacidosis (DKA) or acute kidney injury (AKI). Both are life-threatening. And they happen more often than you think: nearly 1 in 8 diabetes-related hospital stays is caused by improper medication use during illness, according to CDC data from 2023.
Why Illness Changes Everything for Diabetes Meds
Your body doesn’t care if you’re sick or not-it reacts the same way. When you’re ill, your liver pumps out extra glucose. Your stress hormones rise. Your kidneys work harder. And if you’re not eating or drinking enough, your meds can turn dangerous.
Take metformin, for example. It’s safe when you’re healthy. But during vomiting, diarrhea, or fever, your kidneys can’t clear it properly. That builds up lactic acid in your blood-leading to lactic acidosis. Studies show this risk jumps 8.3 times when creatinine levels rise above 1.5 mg/dL. That’s why stopping metformin during illness isn’t optional-it’s essential.
Same goes for SGLT2 inhibitors like dapagliflozin or empagliflozin. These drugs make your kidneys flush out sugar through urine. Sounds good, right? But when you’re dehydrated from illness, they can trigger euglycemic DKA-even when your blood sugar looks normal. The FDA flagged this in 2021 after 1,247 adverse events. Waiting even 24 hours after vomiting to stop these meds increases DKA risk by 300%.
And don’t forget your blood pressure meds. ACE inhibitors and ARBs (like lisinopril or losartan) are common for people with diabetes. But when you’re not drinking enough fluids, they can cause your kidneys to shut down. A 2022 meta-analysis found a 40% spike in AKI when fluid intake drops below 1,500 mL a day. That’s just six 8-oz glasses. Easy to miss when you’re too sick to eat or drink.
What to Do When You’re Sick: The Medication Breakdown
There’s no one-size-fits-all rule. Your meds matter. Here’s what you need to know, based on the latest ADA and IDF guidelines (2023-2025):
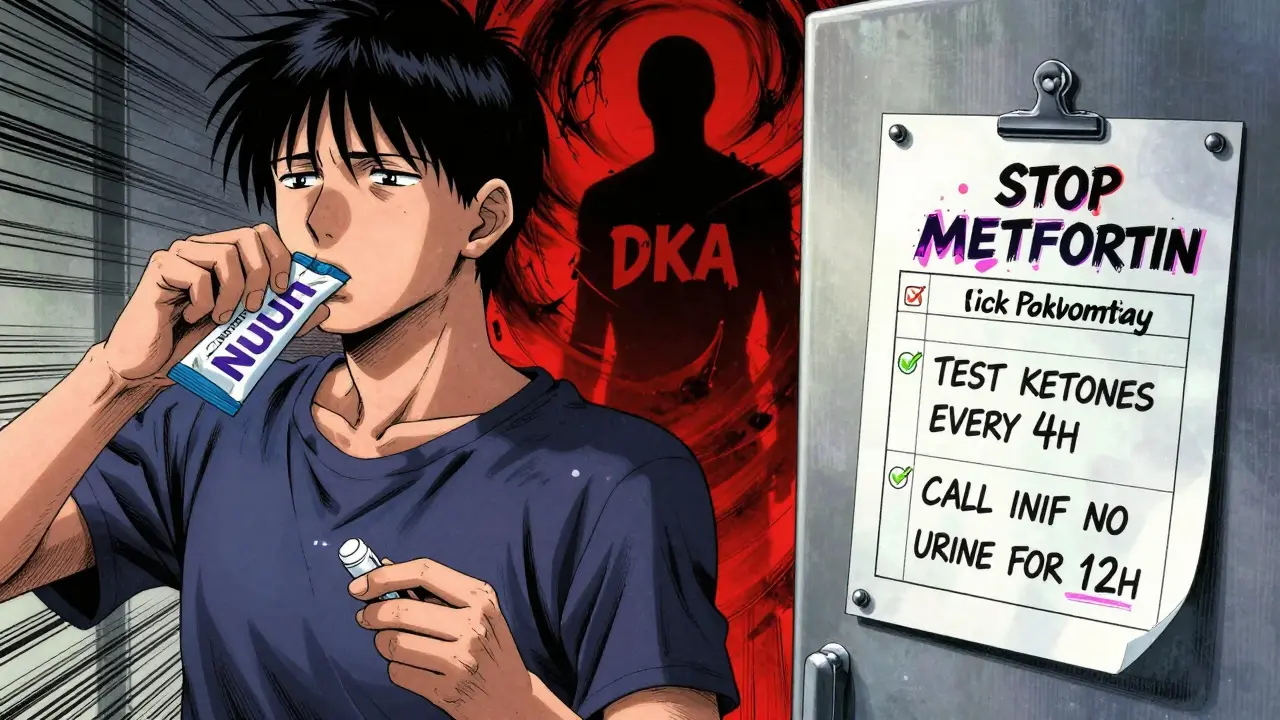
- Metformin: Stop immediately if you’re vomiting, have diarrhea, or have a fever above 100.4°F (38°C). Don’t restart until you’ve eaten normally for 24 hours and your doctor says it’s safe.
- SGLT2 inhibitors (Jardiance, Farxiga, Invokana): Stop at the first sign of illness-even if you feel fine. No exceptions. Restart only after your provider clears you, usually after 2-5 days of being symptom-free.
- ACE inhibitors / ARBs: Pause if you’re drinking less than 1,500 mL (about 6 cups) of fluid in 24 hours. This includes water, broth, or sugar-free drinks. Don’t wait for symptoms like swelling or reduced urine output.
- Insulin: Never skip insulin, even if you’re not eating. Type 1 patients need 10-20% more basal insulin every 4 hours if blood sugar is above 15 mmol/L (270 mg/dL). Type 2 patients on insulin often need higher doses too-68% do, according to a 2023 Diabetes Care trial. Use your correction factor, but check with your provider if you’re unsure.
- Sulfonylureas (glipizide, glyburide): These can cause dangerous lows when you’re not eating. Talk to your doctor about reducing the dose or skipping it if you’re not eating solid food.
- GLP-1 agonists (Ozempic, Mounjaro): These are new, and guidelines are still catching up. Most experts recommend holding them during illness until you’re eating normally again. Check with your provider-don’t guess.
Monitoring: What You Must Track Every Day
When you’re sick, your usual routine goes out the window. But your monitoring can’t. Here’s what you need to check-and how often:
- Blood glucose: Test every 2-4 hours. That’s at least 6 times a day. Set alarms on your phone if you have to. Target range during illness: 100-180 mg/dL (5.6-10 mmol/L). Don’t panic if it’s a little high-focus on trends.
- Ketones: Test when your blood sugar hits 240 mg/dL (13.3 mmol/L) or higher. Use either urine strips or a blood ketone meter. If blood ketones are above 0.6 mmol/L or urine ketones are above 1.5 mmol/L, call your doctor or go to the ER. Don’t wait.
- Fluid intake: Aim for at least 1,500 mL (6 cups) of fluids daily. Water, sugar-free tea, broth, or electrolyte drinks like Nuun. Avoid sugary drinks unless you’re treating a low.
- Urine output: If you’re peeing less than usual-or not at all-that’s a red flag for AKI. So is swelling in your ankles or face.
- Body temperature: Fever above 100.4°F (38°C) means it’s time to stop metformin and SGLT2 inhibitors.
Emergency Signs: When to Call 999 or Go to A&E
These aren’t suggestions. These are alarms.
- Blood sugar below 70 mg/dL and doesn’t improve after 30g of fast-acting carbs (like juice or glucose tabs)
- Ketones above 1.5 mmol/L that don’t drop after 2 hours of fluids and insulin
- Vomiting for more than 4 hours
- Diarrhea for more than 6 hours
- Confusion, extreme fatigue, or fruity-smelling breath (signs of DKA)
- Little or no urine for 12+ hours, or swelling in legs/face (signs of AKI)
If any of these happen, don’t wait. Call 999 or go to your nearest emergency department. Say: “I have diabetes and I think I’m in DKA or AKI.” They’ll know what to do.
Prepare Ahead: The Sick-Day Kit
Waiting until you’re sick to figure this out is too late. Build your kit now-ideally by October, before flu season hits.
Here’s what to keep in your kit:
- Glucose meter with 50+ test strips
- Ketone strips (urine or blood-get both if you can)
- 7-day supply of all your diabetes meds (in original bottles)
- 6 sugar-free drinks (12 oz each)-water, tea, electrolyte drinks
- 10 packets of electrolyte replacement (Nuun, DripDrop, or similar)
- Fast-acting carbs: juice boxes, glucose tabs, honey packets
- ADA Sick Day Log (print it from ada.org)
- Written plan from your doctor: who to call, what meds to stop, emergency numbers
Keep this kit in one place-like your medicine cabinet or fridge. And make sure someone in your household knows where it is.

Conflicting Advice? You’re Not Alone
Here’s the messy part: not every doctor agrees. Some say keep metformin. Others say stop it. One endocrinologist told a Reddit user to “always take your meds unless told otherwise”-but that’s not what the ADA says.
A 2024 survey of 1,200 patients found 28% were confused by conflicting advice. And 41% got different instructions from their GP versus their diabetes specialist. That’s dangerous.
So here’s what to do:
- Ask your doctor for a written sick day plan before you get sick.
- Keep a copy on your phone and in your sick-day kit.
- If you’re unsure, call the ADA helpline: 1-800-DIABETES (available 24/7).
- Don’t rely on Google. Don’t trust random forum advice. Go to the source: ada.org or diabetes.org.uk.
Why This Matters More Than Ever
The number of people with diabetes in the U.S. is rising-34.2 million in 2023. And the flu season of 2024 saw a 27% jump in diabetes-related hospitalizations compared to 2022. Older adults, especially those with kidney disease or heart failure, are at highest risk. By 2030, nearly half of all diabetes patients will be over 65.
Current guidelines were made for healthy adults. They don’t fully account for frailty, multiple meds, or kidney decline. That’s why personalized plans matter. Your dose of metformin (300mg vs. 2,000mg) changes your risk. Your age, your other meds, your kidney function-these all change the rules.
That’s why the next big push in diabetes care is AI-driven tools. Apps like Glooko’s Illness Advisor (in beta as of late 2024) can suggest real-time dose changes based on your glucose trends. But until then, you’ve got to be your own advocate.
Bottom Line: Know Your Meds, Know the Signs, Act Fast
Being sick with diabetes doesn’t have to mean a hospital stay. But it does require preparation. You can’t wing it. You can’t hope for the best. You need a plan-and you need to follow it.
Stop metformin and SGLT2 inhibitors at the first sign of illness. Never skip insulin. Test your blood sugar and ketones often. Drink fluids. Know your emergency signs. And never hesitate to call for help.
It’s not about being perfect. It’s about being prepared. And that’s the difference between staying home-and ending up in the ER.
Should I stop my metformin if I have a cold?
Yes-if you have a fever, vomiting, or diarrhea. Even a mild cold can reduce your fluid intake and stress your kidneys. Metformin builds up in your system when you’re dehydrated, raising your risk of lactic acidosis. Stop it immediately if you’re not keeping fluids down. Restart only after you’ve eaten normally for 24 hours and your doctor says it’s safe.
Can I still take my blood pressure pills when I’m sick?
Not if you’re drinking less than 1,500 mL (about 6 cups) of fluids in 24 hours. ACE inhibitors and ARBs (like lisinopril or losartan) can cause acute kidney injury when you’re dehydrated. If you’re vomiting, have diarrhea, or can’t keep fluids down, pause them until you’re eating and drinking normally again. Check your urine output-if it’s low or you’re swollen, get medical help.
Do I need to test for ketones even if my blood sugar is normal?
Yes, especially if you’re on an SGLT2 inhibitor. These drugs can cause euglycemic DKA-where ketones rise even when blood sugar is under 200 mg/dL. If you’re sick and feeling unwell, test ketones when your blood sugar hits 180 mg/dL or higher. If ketones are above 0.6 mmol/L (blood) or 1.5 mmol/L (urine), call your doctor or go to the ER.
What if my doctor says to keep taking my SGLT2 inhibitor?
The FDA and ADA both say to stop SGLT2 inhibitors during illness. If your doctor disagrees, ask for their reasoning. You may need a second opinion. These drugs carry a 7.2-fold higher risk of DKA during illness, according to FDA data. Don’t rely on one doctor’s opinion if it contradicts national guidelines. Your safety matters more than convenience.
I’m on insulin-should I take less if I’m not eating?
No-never skip your basal (long-acting) insulin. Your body still needs it to stop ketone production, even if you’re not eating. You may need to reduce your mealtime (bolus) insulin if you’re not eating carbs. But your basal dose often needs to go up, not down, when you’re sick. Check your blood sugar every 2-4 hours and adjust based on trends, not just food intake. If you’re unsure, call your diabetes team.
How do I know if I’m developing kidney problems?
Early signs of acute kidney injury (AKI) include: urinating much less than usual, swelling in your ankles or face, feeling unusually tired, or nausea. If you’re on ACE inhibitors or ARBs and you’ve been sick for more than 24 hours with low fluid intake, these signs are urgent. Don’t wait for blood tests-call your doctor or go to A&E if you notice any of these.
What should I drink when I’m sick and have diabetes?
Water is best. Sugar-free tea, broth, and electrolyte drinks like Nuun or DripDrop are good too. Avoid sugary sodas unless you’re treating a low blood sugar. If you’re vomiting or have diarrhea, electrolyte replacement is critical. Aim for at least 1,500 mL (6 cups) per day. If you can’t keep fluids down, get medical help-don’t wait.
Can I use over-the-counter cold medicine?
Be careful. Many cold and flu medicines contain sugar, alcohol, or decongestants that raise blood sugar. Look for sugar-free versions. Avoid decongestants like pseudoephedrine if you have high blood pressure. Always check with your pharmacist or doctor before taking anything new. And never take aspirin if you’re on metformin-it can increase lactic acidosis risk.
Write a comment
Your email address will not be published.




8 Comments
Bro. I took my Jardiance while sick last winter. Thought I was fine. Woke up at 3 AM smelling like a bakery that caught fire. 😵💫 Turned out I had euglycemic DKA. Blood sugar was 140. Ketones? 3.8. ER nurse said I was one napkin away from a coma. STOP THE SGLT2s. NO EXCEPTIONS. 🚨
The data is clear but the framing is performative. Illness is a variable. Metformin risk is not binary. You're reducing complex physiology to a checklist. People die from hypoglycemia too. Why isn't that the headline?
I just want to say thank you for writing this. My dad has type 2, kidney issues, and takes metformin + lisinopril. He didn’t know any of this. I printed out your sick-day kit list and put it next to his meds. He’s 72. I’m scared for him. But now? He’s not scared anymore. 🙏
OMG YES. I’ve been on Ozempic for 8 months and got the flu last month. I felt fine but kept my ketone strips handy. Tested at 180 mg/dL - ketones at 0.7. Called my endo at 11 PM. She said STOP IT. I did. Felt better in 12 hours. Don’t be a hero. Your pancreas doesn’t care how cool you think you are. 💪💉
The ADA guidelines are not gospel. They’re consensus documents written by committees who’ve never seen a real patient dehydrate in a nursing home. Your ‘1,500 mL fluid’ rule is laughable for elderly patients with CHF. This is dangerous oversimplification dressed as safety.
I’m just here to say I keep my sick kit in the fridge next to the almond milk. It’s a weird flex but it works. Also, I use DripDrop. Tastes like lemon-lime candy. Not gross. I’m alive because of this post.
In India, most people don't have ketone strips. We use urine dipsticks. They're cheap. But they lie. If you're vomiting and your sugar is normal? Assume ketones are climbing. Drink water. Call your doctor. Don't wait for the strip to turn purple. Your life isn't a lab test.
Look, I get it. You’re trying to save lives. But this post reads like a medical thriller written by someone who’s never met a diabetic who actually works a 60-hour week, has two kids, and can’t afford to miss a shift. I stopped metformin during my flu. Then I got a 300% bill from the ER because I needed IV fluids. And guess what? My doctor said I didn’t need to stop it. So now I’m stuck between a rock and a hard place - and your ‘life-or-death’ advice didn’t account for the fact that I can’t afford to be wrong. Maybe the problem isn’t the patient. Maybe it’s the system that makes us choose between medicine and rent.