
It’s hard to bring up overdose risk with your doctor-even if you’re taking prescribed pain meds, have a history of substance use, or just want to be prepared. You might fear being labeled, judged, or dismissed. You’re not alone. In fact, 68% of people with substance use disorder report being spoken to in a shaming way by healthcare providers. But you don’t have to accept that. You can have this conversation without shame-and get the help you need.
Start with the right language
The words you use matter. Saying "I’m an addict" or "I can’t control my use" can trigger bias, even if that’s how you feel inside. Instead, use person-first language: "I have a substance use disorder." This isn’t about being politically correct-it’s about science. A 2022 Johns Hopkins study found that doctors are 37% more likely to respond with care when patients use this language. Don’t say: "I’m addicted to opioids."Do say: "I’ve been using oxycodone for my back pain, and I’m concerned about the risk of overdose." This shift helps your doctor see you as a patient, not a stereotype. And it opens the door to real help.
Be specific about your use
Doctors don’t know what you’re not telling them. Vague statements like "I’m worried I might overdose" often get ignored or misinterpreted. Be ready with facts:- What medications you take (name, dose, how often)
- Whether you’ve ever taken someone else’s pills
- If you’ve used alcohol or other substances with your prescription
- Any past experiences where you felt you lost control
Ask for naloxone like you’d ask for an EpiPen
Naloxone reverses opioid overdoses. It’s safe, easy to use, and works in minutes. But many patients don’t ask for it because they think it’s only for "drug users." That’s stigma talking. The American Medical Association compares naloxone to an EpiPen for allergies or a defibrillator for heart issues. If you have a chronic condition, you don’t wait for a crisis to get a safety tool-you plan ahead. Say this: "I’d like to discuss overdose prevention strategies and receive naloxone as a safety measure." A 2021 JAMA Internal Medicine study found that patients who used this exact phrase were 62% more likely to get naloxone than those who said something vague like "I’m scared I’ll overdose." And now it’s cheaper than ever. Since the FDA approved the first generic nasal naloxone in July 2023, the price has dropped from $130 to $25 per kit.
Anticipate the pushback-and stay calm
Not every doctor will respond well. Some still believe myths like: "If you’re using opioids long-term, you deserve what happens." Or worse: "Are you using heroin?" In a 2019 survey, 43% of healthcare providers held negative attitudes toward patients with opioid use disorder. That’s not your fault. But it’s something you can prepare for. If your doctor says something judgmental, try this:- "I understand you might be concerned, but I’m here to stay safe. That’s why I’m asking."
- "I’ve read the CDC guidelines on overdose prevention. They recommend discussing this with all patients on opioids."
- "I’m not asking for more pills-I’m asking for a way to survive if something goes wrong."
Frame it as part of your overall care plan
The CDC updated its opioid prescribing guidelines in August 2023 to say this: "Assessment of overdose risk should be routine for all patients prescribed opioids, regardless of perceived risk." That means it’s not unusual. It’s standard. Say: "As part of my comprehensive health plan, I’d like to discuss overdose prevention, just like we talk about blood pressure, diabetes, or fall risks." This shifts the conversation from morality to medicine. It’s not about whether you "deserve" help-it’s about whether your care team is doing their job.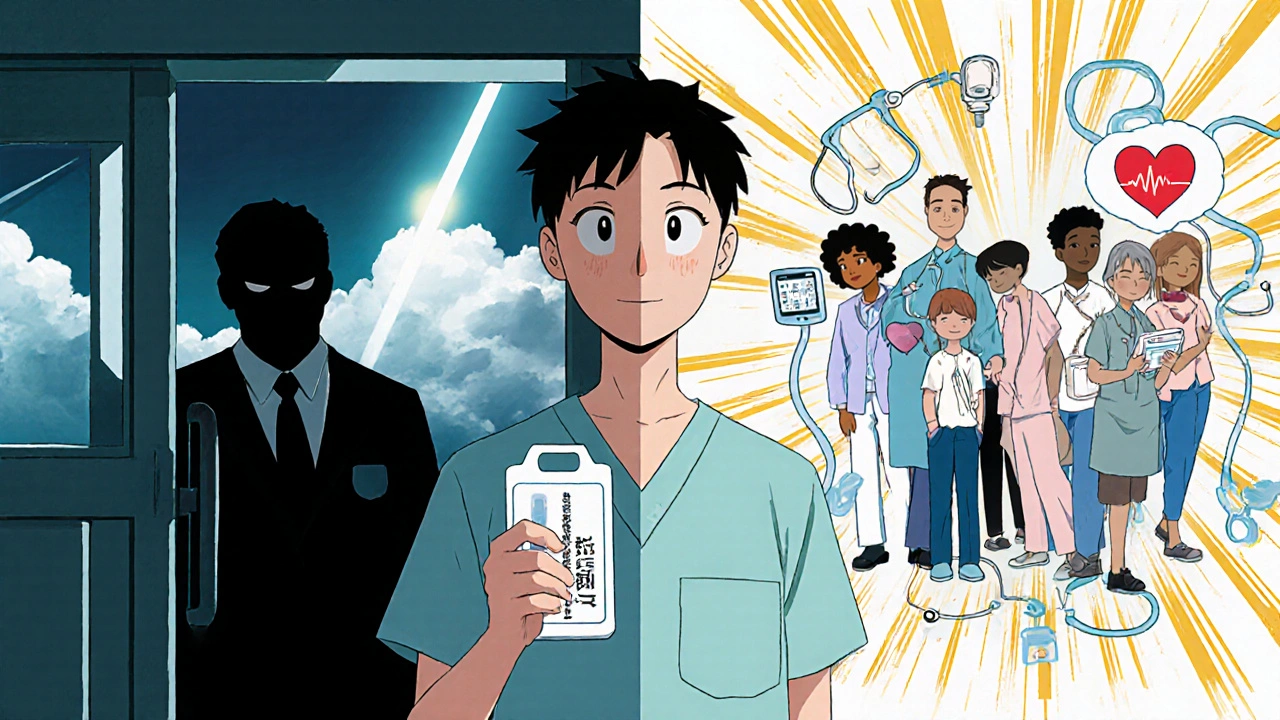
Use trusted resources to back you up
Bring printed material. Not to prove you’re "right," but to show you’ve done your homework. The CDC’s Stigma Reduction Toolkit, the AMA’s patient-friendly guide to talking about substance use, and SAMHSA’s Talking Points for Patients are all free and available in 12 languages. Print one page. Hand it to your doctor. Many patients report better outcomes when they do this. One Reddit user wrote: "I brought the CDC’s talking points to my appointment and said, ‘I want to discuss overdose prevention as part of my comprehensive care plan.’ My doctor immediately prescribed naloxone without judgment." You’re not being difficult. You’re being informed.Know your rights and resources
You have the right to non-stigmatizing care. Since 2017, federal law requires providers who take Medicare or Medicaid to complete stigma training. By 2022, 89% had done so. Still, access isn’t equal. In rural areas, only 28% of providers are trained to prescribe buprenorphine. In cities, it’s 56%. That gap matters. If your doctor refuses to help:- Ask for a referral to a provider trained in addiction medicine
- Contact SAMHSA’s National Helpline: 1-800-662-4357. It’s free, confidential, and available 24/7. In 2022, they handled nearly 300,000 calls.
- Visit SMART Recovery or other peer support groups. They offer weekly online meetings specifically to help people prepare for doctor visits.
Why this matters more than ever
In 2023, the U.S. government launched its National Overdose Prevention Strategy-with stigma reduction as a core goal. They’re training 500,000 healthcare providers by 2025. By 2025, 15% of Medicare payments will be tied to how well doctors reduce stigma. This isn’t just policy. It’s personal. Every time you speak up, you’re not just protecting yourself. You’re helping change the system. Because if more patients ask for naloxone, more doctors will carry it. If more people use person-first language, more providers will learn it. You’re not asking for permission to survive. You’re claiming your right to care.Overdose isn’t a moral failure. It’s a medical event. And like any medical event, it’s preventable-with the right tools, the right talk, and the right courage.
Write a comment
Your email address will not be published.





11 Comments
I just brought up naloxone at my last appointment and my doctor acted like I asked for a gun. But I said it like the article said-"safety measure"-and he actually handed me one. No judgment. Just a nod and a prescription.
Stop coddling people who can't control their drug use. This article is just enabling. If you're taking opioids long-term, you're asking for trouble. Naloxone isn't a magic shield-it's a Band-Aid on a bullet wound. You should be in rehab, not getting free medicine.
Frances, I hear you-but you're missing the point. This isn't about rewarding bad behavior. It's about saving lives while people are still trying to get help. I lost my brother to an overdose. He never asked for naloxone because he thought he'd be judged. What if he'd known he could walk in and say, "I'm scared I'll take too much" and get help instead of a lecture? That's what this is about. Not permission. Protection.
Just wanted to add: the CDC toolkit is available in Spanish, Arabic, and Mandarin too. I printed the one-pager for my mom who speaks limited English. She took it to her pain specialist last week. He actually read it, then said, "You're right. We should be doing this for everyone." It's not about being loud-it's about being prepared.
As a physician who has completed the required stigma training under federal guidelines, I can confirm that the language shift described here is empirically validated. Patients who use "I have a substance use disorder" instead of "I'm an addict" are significantly more likely to receive comprehensive care, including medication-assisted treatment and naloxone prescriptions. The data is not anecdotal-it's institutional. This article is not advocacy; it is clinical best practice.
Yes! Yes! YES! I brought my "medication timeline"-written in pen, on paper, with dates and doses and even the name of the pharmacy I got the script from-and my doctor actually paused, looked up, and said, "You're the first person who's done this." I cried. Not because I was scared-but because I felt seen. If you're reading this and you're scared to talk? Do it. Write it down. Bring it. You're not being difficult. You're being smart.
Wait-I just checked the JAMA study cited here. The 62% increase was for the exact phrase "overdose prevention strategies and receive naloxone as a safety measure." Not "I want naloxone." Not "Can I get this?" But the full, structured sentence. That’s wild. I tried it last week. My doctor didn’t even blink. Just wrote the script. I’m going to print this and tape it to my bathroom mirror.
It’s not about whether you "deserve" help. It’s about whether your healthcare system is designed to keep you alive. I’m a nurse. I’ve seen patients die because they were too ashamed to say they took an extra pill. Shame kills faster than any drug. This article isn’t soft-it’s surgical. It cuts through the noise and gives you the scalpel to save your own life.
There’s a deeper layer here: the idea that medical care should be a right, not a reward. If we treat overdose like a moral failing, we treat people like criminals. But if we treat it like a medical event-like asthma or diabetes-we treat them like patients. That shift in framing changes everything. Not just the conversation. The outcome.
So we’re now treating addiction like a car maintenance issue? "I’m due for my naloxone oil change." This is dehumanizing. People aren’t machines. You don’t just swap out a part and call it done. This is about soul. About redemption. About whether someone wants to live. And no checklist or CDC pamphlet replaces that. You can’t script humanity.
Oh wow, so now we’re giving free antidotes to people who can’t stop doing drugs? Next they’ll hand out parachutes to skydivers who don’t know how to pull the cord. This is just taxpayer-funded enabling. Let them face consequences. That’s how people learn.