Getting the quantity and directions right on a controlled substance prescription isn’t just good practice-it’s the law. One wrong number, one unclear sig, and you could be looking at a DEA enforcement action, a license suspension, or worse, a patient harmed by a dosing error. In 2023, over 6,200 pharmacy and prescriber enforcement actions were tied to verification failures. Most of them? Simple mistakes in quantity or directions that could’ve been caught with a checklist and a second look.
What You Must Verify on Every Controlled Prescription
The DEA requires seven mandatory elements on every controlled substance prescription. Skip one, and you’re non-compliant. These aren’t suggestions-they’re legal requirements under 21 CFR § 1306.05. Here’s what you need to check every single time:- Prescriber’s full name and address - No abbreviations. If it says "Dr. J. Smith, 123 Main St," that’s fine. If it says "Dr. Smith, 123 Main," you need to call and confirm.
- Date of issue - Schedule II prescriptions must be dated the day they’re presented. For Schedules III-V, the date can’t be more than six months old.
- Patient’s full name and address - Middle initials count. "J. Doe" and "John Doe" are different if the PDMP shows one but not the other.
- Drug name and strength - "Hydrocodone 5mg" isn’t the same as "Hydrocodone 7.5mg." Spell it out. Don’t assume.
- Dosage form - Tablet, capsule, liquid, patch? Each has different dosing implications, especially with opioids.
- Quantity prescribed - This is where most errors happen. The number must match the written word. "30 tablets" must equal "thirty (30)." If it doesn’t, pause. Call the prescriber.
- Directions for use (sig) - "Take one by mouth every 6 hours as needed for pain" is clear. "1 q6h PRN pain" is acceptable. "Take 1 tid"? That’s vague. Clarify it.
Don’t rely on memory. Print a checklist. Tape it to your monitor. Use it until it’s automatic.
Quantity Verification: The #1 Error Point
In 2022, 2% of all Medicaid prescription rejections were because the written quantity didn’t match the numerical quantity. That’s not a small number-it’s 1 in 50 prescriptions. And it’s preventable.Here’s how to catch it:
- Read the number out loud. "Thirty tablets."
- Look at the number next to it. "30."
- Do they match? If yes, move on. If no, stop. Don’t fill it.
- If the prescription says "30" but the handwriting looks like "80," call the prescriber. Don’t guess.
- Check the refill field. Is it marked "0"? If the quantity is 120 tablets and the refill says "3," that’s 480 tablets total. Is that clinically appropriate? If not, question it.
Handwritten prescriptions are the biggest risk. A 2023 Pharmacy Times survey found 68% of pharmacists struggle with illegible handwriting. Forty-one percent say they have to call a prescriber at least once a day just to clarify a quantity or direction. Don’t be embarrassed to call. It’s your job.
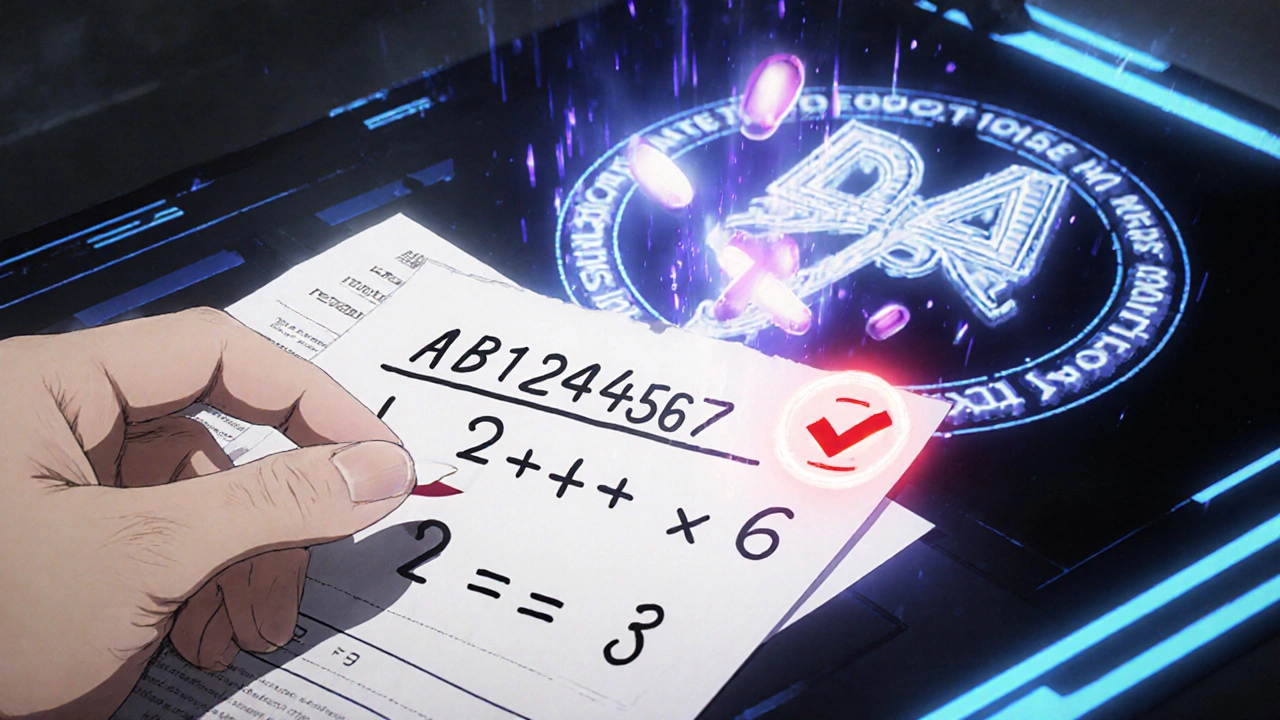
DEA Number Validation: The 3-Step Math Check
A DEA number isn’t just a random string. It’s a coded identifier with a built-in checksum. You don’t need software to verify it-you need a calculator.Here’s the official DEA method:
- Take the first letter. It should be A, B, F, G, M, or X (for prescribers). If it’s not, the number is invalid.
- The second letter must match the prescriber’s last name initial. If the prescriber is Dr. Patel, the second letter must be P. If it’s R, stop.
- Now, the math:
Take the DEA number: AB1234567
- Add the 1st, 3rd, and 5th digits: 1 + 3 + 5 = 9
- Add the 2nd, 4th, and 6th digits: 2 + 4 + 6 = 12 → Multiply by 2 → 24
- Add both results: 9 + 24 = 33
- The last digit of that sum (3) must match the 7th digit of the DEA number.
33 → last digit is 3. DEA number’s 7th digit is 3. ✅ Valid.
The DEA says this catches 98.7% of fake DEA numbers. You don’t need an app. You need to know this. Practice it. Do it on every prescription.
PDMP Review: Your Real-Time Safety Net
In 49 states, you’re required to check the Prescription Drug Monitoring Program (PDMP) before dispensing controlled substances. But not all PDMPs are equal.Only 27 states require real-time data submission (under 5 minutes). The rest? Some take 24 hours. Some take a week. That gap? That’s where diversion happens.
Here’s how to use PDMP effectively:
- Check before you fill. Not after.
- Look for red flags: multiple prescribers, multiple pharmacies, overlapping prescriptions.
- Check the quantity and frequency. Is a patient getting 120 hydrocodone tablets every 10 days? That’s 360 per month. CDC guidelines say that’s excessive.
- Use PMP InterConnect. It’s the most reliable cross-state system. Pharmacists using it report a 37% reduction in verification time.
California pharmacists spend an average of 22 minutes per PDMP check. Tennessee? Nine minutes. Why? California’s system pulls in more data points. Don’t get frustrated-get efficient. Learn your state’s system. Bookmark it. Make it part of your workflow.
Opioid Conversion Factors: Don’t Guess, Calculate
Methadone, fentanyl, hydromorphone-these aren’t like regular painkillers. Their potency varies wildly. A 10mg tablet of morphine is not the same as 10mg of hydromorphone. That’s why the CDC’s 2022 opioid conversion factors are non-negotiable.Here are the key ones you need to know:
| Opioid | Conversion Factor |
|---|---|
| Codeine | 0.15 |
| Hydrocodone | 1 |
| Hydromorphone | 4 |
| Methadone (0-20mg/day) | 4 |
| Methadone (21-40mg/day) | 8 |
| Methadone (41-60mg/day) | 10 |
| Methadone (≥61mg/day) | 12 |
| Fentanyl patch (25mcg/hr) | 2.4 |
Example: A patient is prescribed 60mg of hydrocodone per day. That’s 60 morphine equivalents. Now they get a script for 20mg of hydromorphone per day. That’s 80 morphine equivalents. You just doubled their dose. That’s dangerous. You need to call the prescriber.
Keep a laminated copy of this table in your dispensing area. Or save it as a screenshot on your phone. Don’t rely on memory.
What the Experts Say: The 5-Point Verification Protocol
Dr. John R. Overstreet, former DEA Diversion Control Director, says: "Single-point verification is insufficient in the current opioid crisis." He’s right.The American Society of Health-System Pharmacists (ASHP) recommends this 5-point protocol:
- DEA number validation - Use the 3-step math check.
- PDMP review - Check for red flags, overlapping scripts, high volumes.
- Prescription integrity check - Look for tampering: microprinting, security paper, void indicators.
- Prescriber verification - Call if anything looks off. Even if it’s after hours.
- Clinical appropriateness - Use CDC conversion factors. Is this dose safe? Is this quantity reasonable?
Pharmacies using all five points have 4% diversion incidents. Those using one or none? 31%. The numbers don’t lie.
What’s Changing in 2025 and Beyond
The DEA announced in May 2024 that all controlled substance prescriptions must include a QR code by 2026. This will link to a digital record of the prescription, including prescriber, patient, and product details-tracing it from the pharmacy back to the manufacturer.That’s not science fiction. It’s coming. And it’s built on the DSCSA standards that became mandatory in November 2023. Pharmacies that haven’t upgraded their systems are already at risk of enforcement.
Meanwhile, AI tools are being piloted in 12 states to flag suspicious patterns-like a patient getting high-dose opioids from three different prescribers in three weeks. These aren’t replacing pharmacists. They’re giving you better data to make faster, safer decisions.
Final Checklist: Before You Hand Over the Bottle
Before you seal that prescription, ask yourself:- Did I verify the DEA number using the 3-step math?
- Did the written quantity match the numerical quantity?
- Did I check the PDMP today?
- Did I confirm the sig is clear and safe?
- Did I cross-reference opioid doses using CDC factors?
- Did I call the prescriber if anything felt off?
If you answered yes to all six, you’ve done your job. Not just legally. Ethically. Safely.
There’s no software that replaces your judgment. No app that catches a poorly written sig. No system that stops you from filling a 90-day supply of methadone when the patient has no history of chronic pain. That’s on you. And you’re the only one who can do it right.
What happens if I don’t verify a controlled substance prescription correctly?
You could face civil penalties up to $758,574 per violation, license suspension, or criminal charges. The DEA reports that 37% of all controlled substance enforcement actions from 2018-2023 were due to verification failures. Even one mistake can cost you your career.
Do I need to check the PDMP for every controlled substance?
Yes-in 49 states, it’s mandatory for Schedule II-V prescriptions. Even in the one state without a mandate, it’s considered best practice. Skipping it increases your risk of dispensing to someone with a history of misuse or doctor shopping.
How do I verify a handwritten prescription I can’t read?
Call the prescriber. Don’t guess. Don’t assume. Use the DEA’s 2023 guidance: if you can’t read the quantity, sig, or prescriber’s name, you must contact them directly. Pharmacies that avoid this step are 3x more likely to be cited in inspections.
Is it okay to fill a prescription with a mismatched quantity?
No. Never. CMS data shows 2% of Medicaid rejections in 2022 were due to quantity mismatches. The DEA considers this a serious violation. If the written quantity says "twenty (20)" but the number says "30," stop. Call the prescriber. Fill the correct amount. Document the correction.
What’s the easiest way to remember DEA number validation?
Remember this: First letter = prescriber type. Second letter = last name initial. Then: Add 1st, 3rd, 5th digits. Add 2nd, 4th, 6th digits and multiply by 2. Add both sums. Last digit must match the 7th digit of the DEA number. Practice it on five prescriptions today. It’ll become automatic.
Are electronic verification systems worth the cost?
Yes. Chain pharmacies using FDA-compliant DSCSA systems report 99.2% accuracy and 31% fewer diversion incidents than those using manual methods. The upfront cost is $15,000-$50,000, but the cost of a single enforcement action can be over $750,000. The ROI is clear.
Next Steps: Build Your Verification Routine
Start tomorrow. Print the DEA number validation steps. Tape them to your screen. Print the CDC opioid conversion table. Put it in your drawer. Use the PMP InterConnect app daily. Call prescribers without hesitation. Track how many times you catch an error. That’s not a burden-it’s your shield.You’re not just filling prescriptions. You’re stopping diversion. You’re preventing overdose. You’re protecting your license. And you’re the last line of defense. Don’t let it slip.
Write a comment
Your email address will not be published.



7 Comments
This is the kind of guide every pharmacy needs taped to their monitor. I printed it out and laminated it. My team and I have caught 3 bad scripts in the last month just by following the checklist. Seriously, if you're not doing this, you're playing Russian roulette with someone's life.
Call the prescriber. No shame in it. I've called at 11pm on a Sunday and still got a response. They appreciate it. We're not just pharmacists-we're the last line of defense.
Ugh. Another bureaucratic laundry list. I’ve been filling scripts for 22 years and never once got nailed. You think the DEA cares about your 3-step math check? Nah. They care about quotas and headlines. This whole thing is performative compliance wrapped in a fancy PDF.
And don’t get me started on PDMP-half the time it’s outdated and the other half it’s so slow you could brew a pot of coffee while waiting. Stop pretending this is safety. It’s liability theater.
The opioid conversion table is correct but incomplete. You omitted the 2024 update to methadone ratios for patients on chronic buprenorphine maintenance. That’s a critical omission-misapplying the 4:1 ratio in that population has led to at least three documented overdoses in the last year.
Also, the DEA number validation method described is outdated. The 7th digit check only applies to legacy formats. Since 2021, new DEA numbers use a modified Luhn algorithm with a different weighting scheme. This guide is dangerously incomplete.
I just wanted to say thank you for writing this. I’m a new pharmacist and I was terrified of making a mistake. This checklist saved me. I printed it, put it in my pocket, and now I use it every single time. I even showed it to my preceptor. She cried.
It’s not perfect, but it’s honest. And that’s what matters.
In India we dont have such strict rules but i see same problem. Pharmacist dont verify anything. Patient come with 100 pills of oxycodone and no PDMP. No call. No nothing. You think america is alone in this? No. This is global problem. You need more training not more checklists
While the intent of this guide is commendable, its reliance on anecdotal data and non-peer-reviewed sources undermines its credibility. The assertion that 68% of pharmacists struggle with illegible handwriting lacks a cited methodology. Furthermore, the claim that AI tools are being piloted in 12 states is misleading-no federal or state agency has publicly confirmed such initiatives as of Q3 2024.
For professional audiences, peer-reviewed references are non-negotiable.
You people are so obsessed with rules you forget we’re dealing with human beings. I had a patient last week with terminal cancer. His pain was unbearable. The script said 30 tablets but the handwriting looked like 80. I called the doctor. He said ‘just give him what he needs.’ I gave him 80. He cried and hugged me.
Now you’re gonna tell me I broke the law? Good. Let them suspend my license. I’d rather be a pharmacist than a robot.