
Buying prescription drugs in the U.S. can feel like walking into a store where the price tag changes every time you turn around. One pharmacy charges $450 for a 30-day supply of your medication. Another down the street wants $89. Same drug. Same dose. Same insurance. What’s going on?
The answer isn’t magic. It’s data-and now, you have tools to see it.
Since 2024, federal rules have forced insurers and pharmacies to show you exactly what you’ll pay before you fill a prescription. No more guessing. No more surprise bills. But knowing these tools exist isn’t enough. You need to know how to use them right-or you’ll still overpay.
Why Drug Prices Vary So Much
It’s not just about where you shop. Your insurance plan, pharmacy network, and even the time of year can change your out-of-pocket cost by hundreds of dollars. A 90-day supply of apixaban, for example, might cost $1,200 at one pharmacy but just $213 at another-even with the same insurance. That’s not a typo. That’s the reality of how drug pricing works in the U.S.
Pharmacies negotiate prices with your insurer. Some get better deals. Some don’t. Manufacturers set list prices, but those rarely matter to you. What matters is your out-of-pocket cost-the amount you pay after insurance kicks in. Most people don’t know the difference, and that’s why they pay too much.
Price transparency tools fix that. They pull real-time data from your plan and show you what you’ll actually pay at nearby pharmacies. Not the list price. Not the wholesale cost. The number on your receipt.
What You Need Before You Start
Before you open any tool, gather three things:
- Your exact medication name and dosage (e.g., “metformin 500 mg”)
- How many pills or days you need (30-day, 90-day, etc.)
- Your insurance plan name and member ID (you’ll need to log in)
If you’re on Medicare, you’ll use the same tools-but your plan might be called Medicare Part D. If you’re insured through your employer, check your benefits portal. Most large employers (78%, according to Kaiser Family Foundation) now offer built-in price tools.
Don’t have insurance? You can still use tools like FAIR Health or GoodRx. They show cash prices, which are sometimes cheaper than your insurance copay.
Top Tools to Compare Drug Prices
Not all tools are made the same. Here are the most reliable ones, based on user reports and industry analysis:
- Rx Savings Solutions: Integrated with 18 of the top 25 pharmacy benefit managers. It doesn’t just show prices-it suggests cheaper alternatives. One 2023 study found it saved users money on 83% of prescriptions.
- Optum Rx: Used by major insurers like UnitedHealthcare and Aetna. Access it through your myCompass account. It’s accurate because it pulls your plan’s exact negotiated rates.
- FAIR Health Consumer: Free, no login needed. Great for people without employer insurance or those on Medicare. Shows prices by zip code.
- Turquoise Health: Used by hospitals and large employers. Less consumer-friendly but very detailed. Good if you’re comparing multiple drugs or need to see historical pricing trends.
- GoodRx: Not a plan-based tool, but it shows cash prices and coupons. Often cheaper than insurance copays for generic drugs.
For most people, start with Optum Rx or FAIR Health. If you’re on a large employer plan, your insurer’s tool is usually the most accurate.

How to Use a Price Tool Step by Step
Follow this process every time you refill a prescription:
- Log in to your insurer’s portal or open FAIR Health/GoodRx.
- Enter your medication name, dose, and quantity.
- Set your location (within 10 miles for best results).
- Compare prices across 3-5 pharmacies. Look for the lowest out-of-pocket cost-not the list price.
- Check if the tool suggests a generic or alternative drug. For example, switching from brand-name lisinopril to generic can cut costs by 80%.
- Call the pharmacy to confirm the price. Sometimes systems lag. Don’t trust the app blindly.
- Fill your prescription at the cheapest location.
It takes 15-20 minutes the first time. After three uses, it takes under 7 minutes. That’s less time than waiting on hold with your pharmacy.
Real Savings: What People Are Actually Saving
People aren’t just saving a few bucks. They’re saving hundreds-or even thousands.
One Reddit user saved $287 on a 90-day supply of apixaban by switching from CVS to Walmart using Rx Savings Solutions. Another slashed their annual medication bill from $1,850 to $620 using Optum Rx’s comparison tool.
A Kaiser Health News report showed a patient reduced an MRI bill from $4,200 to $450 using Healthcare Bluebook. That’s not an outlier. That’s what happens when you stop assuming your pharmacy is the cheapest option.
Studies show people who use these tools save 15-20% on prescriptions on average. For someone taking five medications a month, that’s $300-$500 a year. For chronic conditions like diabetes or high blood pressure, the savings can be over $1,000.
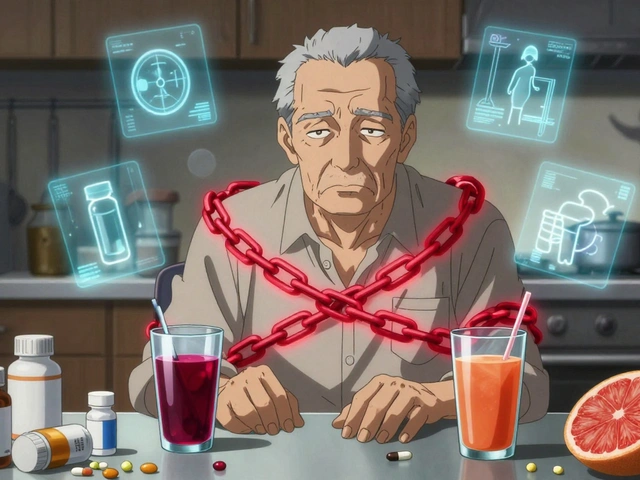
What These Tools Won’t Tell You
They’re powerful-but not perfect.
Some tools still show list prices instead of your actual cost. That’s misleading. Always look for the phrase “your cost” or “out-of-pocket.” If you see “retail price,” ignore it.
Also, not all drugs are covered. Specialty meds, like those for multiple sclerosis or rheumatoid arthritis, often require prior authorization. The tool might show a price, but your insurer might still deny it. Check your plan’s formulary before you commit.
And here’s a big one: GoodRx coupons aren’t always accepted. Some pharmacies won’t honor them if you’re using insurance. Always ask: “Can I use this coupon instead of my insurance?” Sometimes, paying cash is cheaper.

How to Avoid Common Mistakes
Most people make these three errors:
- Using the first pharmacy they see-Don’t. Compare at least three.
- Not checking for alternatives-Tools like Rx Savings Solutions suggest cheaper drugs that work just as well. Ask your doctor if switching is safe.
- Forgetting to call the pharmacy-Systems update slowly. A price shown online might be wrong by the time you get there.
Also, don’t assume your mail-order pharmacy is cheapest. Sometimes, your local CVS or Walgreens has a better deal-especially for 30-day supplies.
What’s Coming Next
By 2026, the Congressional Budget Office estimates that 90% of prescription purchases will involve price comparison tools. That’s up from 40% in 2023.
New tools are adding AI to predict future price drops. Some are integrating quality ratings-like how quickly a pharmacy fills prescriptions or how often they make errors. The federal government is also pushing for blockchain-backed pricing data to stop fraud and inaccurate listings.
And if you’re worried about rising drug costs, there’s new legislation in the works. The Fair Accountability and Innovative Research Drug Pricing Act would require manufacturers to justify price hikes over $100 per month. That could mean fewer sudden spikes.
Final Tip: Make It a Habit
Don’t wait until your prescription runs out. Check prices every time you refill-even if you’ve used the same pharmacy for years. Prices change weekly.
Set a calendar reminder: “Check med prices” every 30 or 90 days. It takes five minutes. The average user saves $400 a year just by doing this.
Drug prices aren’t going to get simpler. But you don’t need to be a pricing expert to save money. You just need to use the tools-and use them right.
Write a comment
Your email address will not be published.




13 Comments
It’s wild how we’ve normalized being robbed by pharmacies like it’s just part of being American. I used to pay $300 for my blood pressure med until I found out Walmart had it for $12. No insurance trickery. Just cash. Why does this feel like a secret only the desperate know?
And don’t even get me started on how the system rewards greed over care. We’re not talking about luxury drugs here-we’re talking about people choosing between insulin and rent.
omg i just tried fair health n saved $200 on my diabetes meds!!! i thought i was stuck payin what the pharmacy said 😭 thank u for this post!!
It is a profound irony, is it not, that in a nation that prides itself on innovation and market efficiency, the most basic human need-access to life-sustaining medication-is subjected to a labyrinthine system of opaque pricing, negotiated in back rooms by corporate entities with no moral compass, and then sold to the public as if it were a commodity like a pair of sneakers?
One might argue that this is not a failure of logistics, but a deliberate design. The profit motive has been elevated above the sanctity of life, and the tools you mention, while useful, are merely bandages on a hemorrhaging wound. Until we confront the structural corruption in pharmaceutical lobbying and patent monopolies, we are merely rearranging deck chairs on the Titanic.
USA still the only country where you need a PhD to buy aspirin
Other countries: $5 for everything
US: 450 bucks if you don't know the magic website
Stop being lazy. Use the tools. It's not that hard. You're not special. You're just dumb.
This changed my life honestly. I used to just take whatever the pharmacist said and cry about it. Now I check every refill. I saved $800 last year on just three meds.
It takes 5 minutes. You can do it. You deserve to not be broke because you're sick.
Also-tell your friends. This isn't a secret. It's a right.
While the practical utility of these tools is undeniable, one must consider the broader sociopolitical context in which they emerge. The necessity of such consumer-driven price arbitrage reflects a systemic failure in public healthcare policy, not merely a gap in consumer literacy.
The fact that individuals must navigate a fragmented, profit-driven ecosystem to access essential medicine suggests that the market has been permitted to supplant the social contract. The tools are helpful, yes-but they are also symptoms of a deeper malaise.
One might reasonably ask: why should a diabetic in Ohio be forced to become a price detective simply to afford their insulin? And why does the burden of systemic failure rest on the shoulders of the vulnerable?
just used optum rx for my zoloft and saved $140 😍 i didnt even know my insurance had this built in
also-turns out my local walgreens was charging me twice what the one 2 miles away did. i felt so dumb.
but hey, better late than never. thanks for the nudge. i’m gonna check my other meds this week. 🙌
Thank you for this. I’ve been telling my mom for years to check prices before she fills anything. She’s 72 and thought it was just how things are.
She used FAIR Health last week and switched from CVS to Target. Saved $210 on her statin. She cried. Not from sadness-from relief.
Everyone deserves to feel this safe. Please share this with someone who’s older. They might not know how to Google it.
Wow. Another ‘you just need to try harder’ article. So now it’s our fault we’re getting gouged? I work two jobs. I don’t have time to compare 5 pharmacies every month.
And don’t even get me started on how these tools don’t work for people without smartphones or internet. You’re preaching to the privileged.
Fix the system. Don’t tell us to be better at surviving it.
This is a classic example of neoliberal victim-blaming disguised as empowerment. The fact that you must use third-party tools to avoid financial ruin simply because your government has failed to regulate pharmaceutical monopolies is not a win-it’s a scandal.
And the suggestion that ‘it only takes five minutes’ ignores the reality of cognitive load for low-income, elderly, or disabled populations. You’re not helping. You’re gaslighting.
It’s funny how we treat medicine like a video game where you have to unlock the right coupon code to survive
What if we just made it a human right instead of a puzzle? What if we stopped celebrating people who ‘beat the system’ and started demanding the system be fixed?
I don’t want to be a price ninja. I just want to be alive without bankruptcy.
Everyone who uses these tools is just enabling the system. You think you’re saving money? You’re just propping up a broken, immoral industry.
Stop playing along. Boycott all pharmacies. Demand national price controls. Or shut up.
Just tried Rx Savings Solutions and it suggested I switch from brand-name lisinopril to generic 💡 saved $220
Also found out my mail-order pharmacy was charging me $40 more than my local CVS 😱
Life hack: set a reminder every 30 days. 5 minutes = $400/year 🤯