Polypharmacy Risk Checker
Your Medication List
Risk Assessment
Risk Assessment Results
Medication Safety Tips
Next Steps
- Bring your medication list to your next doctor appointment
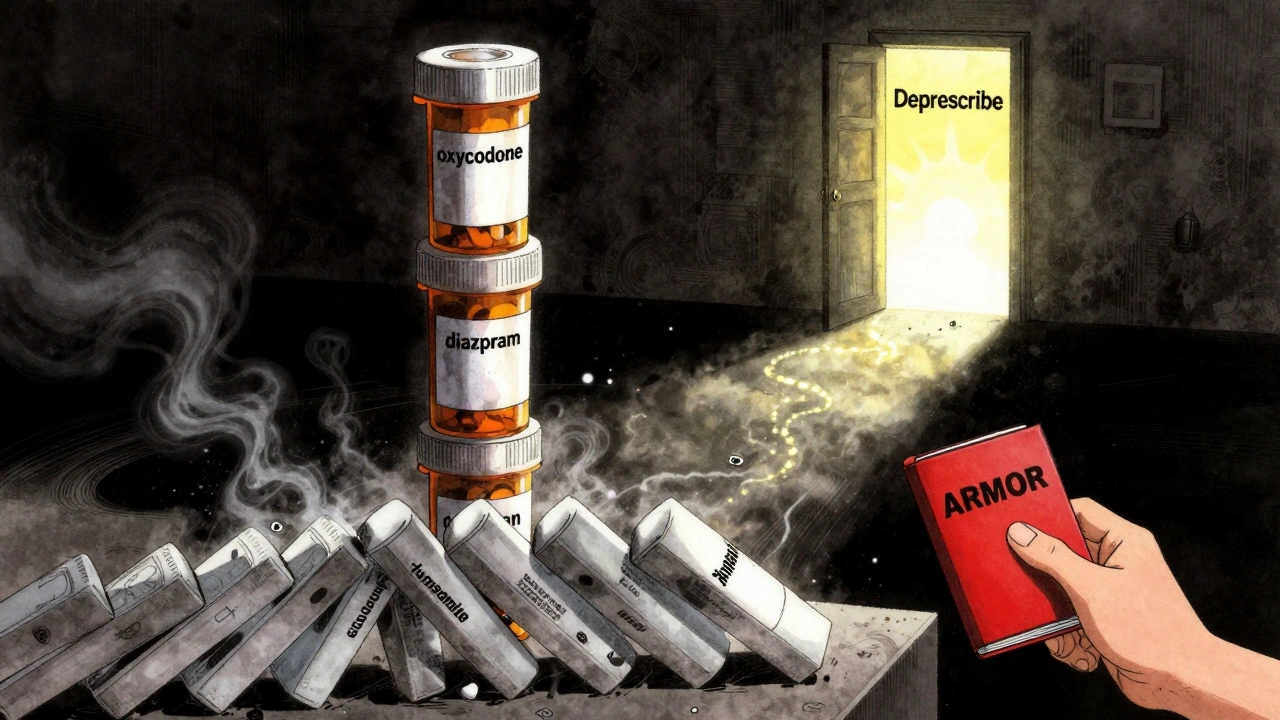
- Ask about the ARMOR tool: Assess, Review, Minimize, Optimize, Reassess
- Request a Medicines Use Review at your local pharmacy
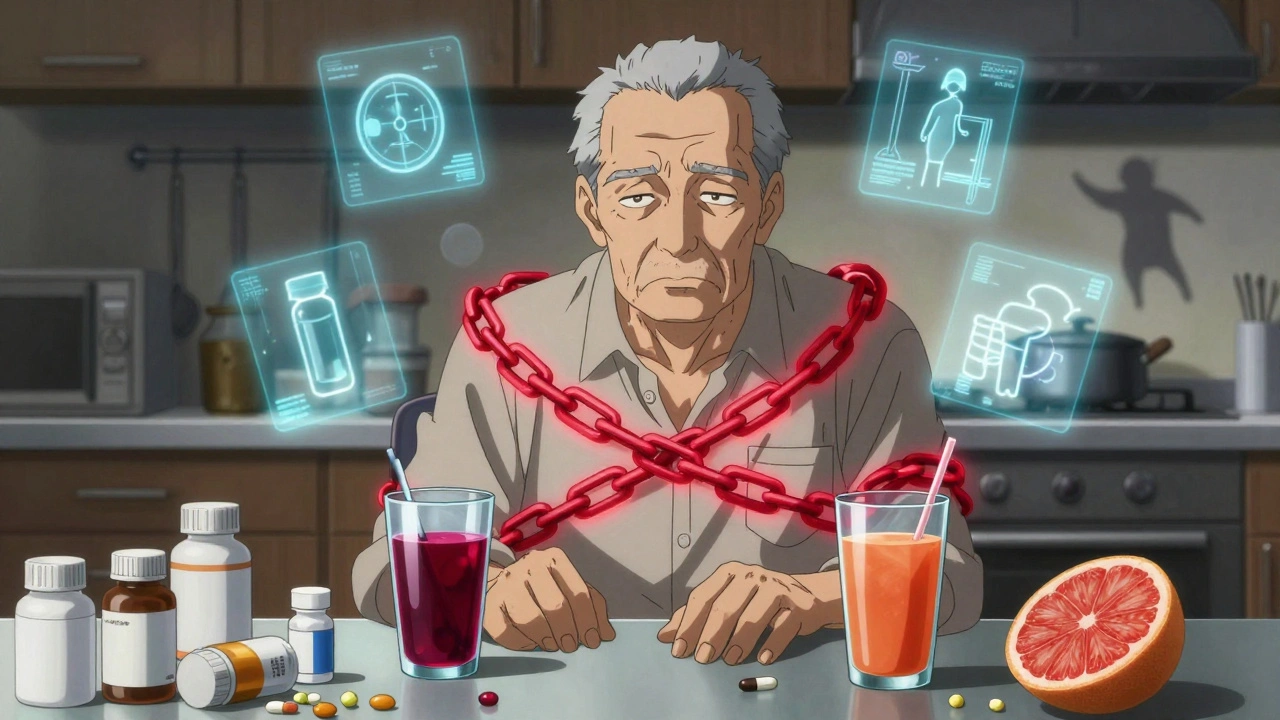
- Check for dangerous combinations like warfarin + cranberry juice
What Is Polypharmacy-and Why Should You Care?
When someone takes five or more medications at the same time, that’s called polypharmacy. It’s not always bad-many older adults need multiple drugs to manage conditions like high blood pressure, diabetes, or arthritis. But the more pills you take, the higher the chance something will go wrong. In the UK and US, about one in three adults in their 60s and 70s are on five or more prescriptions. And that’s not just a number-it’s a ticking time bomb for side effects, falls, confusion, and hospital visits.
Here’s the real problem: most people don’t realize how dangerous some combinations can be. You might take lisinopril for your blood pressure, furosemide to drain extra fluid, and calcium for your bones. Each one is fine on its own. But together? They can throw off your electrolytes, make you dizzy, or even cause your kidneys to struggle. Or worse-you take warfarin to thin your blood, then drink cranberry juice because you think it’s healthy. That combo can turn your blood into a slow leak. No warning. No symptoms until it’s too late.
The Top 5 Dangerous Medication Combos You Need to Know
Not all drug interactions are obvious. Some are hidden in plain sight. Here are five of the most common-and deadly-combinations that show up again and again in emergency rooms and hospital admissions.
- Warfarin + cranberry juice: Warfarin keeps clots from forming. Cranberry juice blocks how your body breaks it down. Result? Your blood can’t clot at all. One glass a day can send you to the ER with internal bleeding.
- Statins + grapefruit juice: Statins like atorvastatin lower cholesterol. Grapefruit juice shuts down the enzyme (CYP3A4) that clears them from your system. That means too much drug builds up. Muscle breakdown (rhabdomyolysis) can follow-sometimes leading to kidney failure.
- Blood pressure meds + decongestants (like pseudoephedrine): If you’re on lisinopril, amlodipine, or metoprolol, and you grab a cold tablet with pseudoephedrine, your blood pressure can spike dangerously. This combo is behind many strokes in older adults during cold season.
- Acetaminophen + oxycodone + prochlorperazine: This trio is often prescribed together for pain and nausea. But together, they cause extreme drowsiness, low breathing, and confusion. Studies show this combo pops up in 30% of ER visits by seniors in the 30 days before admission.
- Benzodiazepines (like diazepam) + opioids (like oxycodone): Both depress the central nervous system. Together, they slow breathing to dangerous levels. The CDC lists this as one of the top causes of accidental overdose in older adults.
These aren’t rare. They’re routine. And they’re preventable.
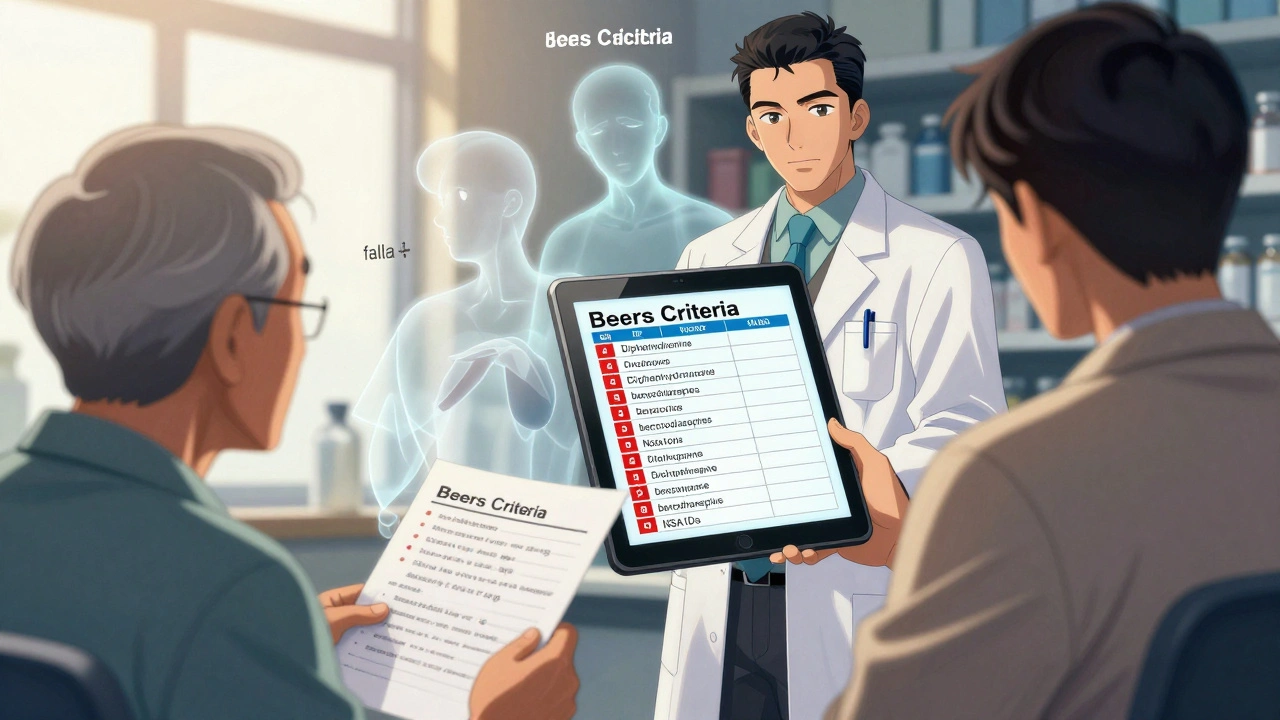
The Beers Criteria: Your Secret Weapon Against Bad Prescriptions
Doctors don’t always know which drugs are risky for older patients. That’s where the Beers Criteria comes in. Updated in 2019 by the American Geriatrics Society, it’s a list of medications that should be avoided-or used with extreme caution-in people over 65.
Here’s what the Beers list flags as high-risk:
- Anticholinergic drugs (like diphenhydramine/Benadryl, oxybutynin): These cause confusion, dry mouth, constipation, and memory loss. They’re often in sleep aids, allergy meds, and bladder pills.
- Benzodiazepines (like lorazepam, alprazolam): Even short-term use increases fall risk by 50%. Long-term use can cause dementia-like symptoms.
- Nonsteroidal anti-inflammatories (NSAIDs like ibuprofen, naproxen): These raise blood pressure, hurt kidneys, and increase stomach bleeding risk-especially when mixed with blood thinners.
- α1-blockers (like doxazosin, terazosin): Used for prostate issues, but they cause sudden drops in blood pressure when standing. That’s a recipe for falls.
If you’re on any of these, ask: Is this still necessary? Many people take them because they were prescribed years ago and never reviewed.
Prescribing Cascades: How One Pill Leads to Five More
Have you ever been prescribed a new drug because of a side effect from another? That’s called a prescribing cascade-and it’s one of the biggest reasons people end up on 10, 12, even 15 medications.
Example: You take oxycodone for back pain. It causes constipation. So your doctor prescribes a laxative. The laxative causes electrolyte imbalance. Now you need potassium supplements. Then you get dizzy from the potassium, so you’re given a diuretic. And on it goes.
Studies show nearly 40% of medications in older adults are prescribed to fix side effects of other meds. It’s a loop with no exit-until someone steps back and asks: What’s the original problem? And do we still need all these pills?
That’s why medication reviews matter. Not once a year. Not when you’re in the hospital. But regularly. And with someone who sees the full picture.
Your Polypharmacy Risk Checklist: 7 Steps to Safer Medications
Here’s a simple, practical checklist you can use today-whether you’re a patient, caregiver, or family member.
- Make a complete list: Write down every pill, patch, liquid, vitamin, herb, and over-the-counter drug you take-including what dose and how often. Don’t forget the aspirin you take daily or the melatonin you use for sleep.
- Bring it to every appointment: Don’t rely on memory. Don’t assume your doctor knows what’s in your cabinet. Hand them the list. Ask: Do I still need all of these?
- Check for Beers Criteria drugs: Look up your meds on the American Geriatrics Society’s Beers Criteria list. If you see one flagged, ask your pharmacist or GP why it’s still being prescribed.
- Ask about food interactions: Grapefruit? Cranberry? Dairy? Alcohol? Ask your pharmacist: What should I avoid eating or drinking with these pills?
- Review every 3-6 months: Medication needs change. A drug that helped last year might be unnecessary now. Schedule a medication review like you would a dental checkup.
- Use the ARMOR tool: Assess your meds. Review why each is prescribed. Minimize what’s not needed. Optimize the rest. Reassess after changes. This simple framework works in clinics and at home.
- Know your red flags: Dizziness, confusion, falls, fatigue, memory slips, constipation, or sudden weight loss? These aren’t just “getting older.” They could be drug reactions.
Who Should You Talk To? Pharmacists Are Your Best Allies
Most people think pharmacists just hand out pills. They’re wrong. Pharmacists are the only healthcare professionals trained to spot drug interactions across all categories-prescription, OTC, supplements, even herbal teas.
In the UK, you can walk into any community pharmacy and ask for a Medicines Use Review (MUR). It’s free. It takes 20-30 minutes. They’ll go through your list, flag risks, and even call your GP to suggest deprescribing.
One 72-year-old cancer patient in Manchester cut her meds from 12 to 7 after a pharmacist used the ARMOR tool. She didn’t lose any treatment effectiveness. She just stopped taking things that were hurting her.
Don’t wait for a crisis. Book a review. Bring your list. Ask the hard questions.
What Happens When You Don’t Act?
Every year in the UK, over 200,000 hospital admissions are linked to adverse drug reactions. Half of them involve people over 65. Polypharmacy is the leading cause.
The cost? Not just financial-though seniors spend £37 billion a year on medications. It’s in lost independence. Falls that break hips. Confusion that leads to nursing home admission. Emergency trips that could have been avoided.
And here’s the worst part: most of these aren’t accidents. They’re systemic failures. Fragmented care. Prescriptions handed out without review. Alerts ignored because doctors are overwhelmed.
You can’t fix the system alone. But you can fix your own list.
Final Thought: Less Is Often More
Medications aren’t magic. They’re tools. And like any tool, too many can make things worse. The goal isn’t to stop all drugs-it’s to stop the ones that don’t belong.
Ask yourself: If I took just three pills tomorrow, which ones would I keep? That’s the question that saves lives.
What counts as polypharmacy?
Polypharmacy is defined as taking five or more medications regularly, including prescription drugs, over-the-counter medicines, vitamins, and supplements. It’s not just about quantity-it’s about whether each drug is still necessary and safe to take with the others.
Can I stop my meds if I think they’re causing side effects?
Never stop a medication suddenly without talking to your doctor or pharmacist. Some drugs, like blood pressure or antidepressant meds, can cause dangerous withdrawal effects. But you can and should ask: Is this still helping me? Your provider can help you taper safely if needed.
Are over-the-counter drugs really risky?
Yes. Many people don’t realize OTC drugs like diphenhydramine (Benadryl), ibuprofen, or even antacids can cause serious interactions. Diphenhydramine is anticholinergic and linked to confusion and falls. Ibuprofen can increase bleeding risk with warfarin or damage kidneys when taken with blood pressure meds. Always include them on your list.
How often should I get a medication review?
At least once every 6 months-or anytime you start or stop a medication, change doctors, or notice new symptoms like dizziness, confusion, or fatigue. If you’re on more than five drugs, quarterly reviews are ideal.
Can pharmacists really help reduce my meds?
Absolutely. Pharmacists are trained to spot unnecessary or risky prescriptions. In the UK, you can get a free Medicines Use Review (MUR) at any community pharmacy. They’ll review your list, flag risks, and even contact your GP to suggest deprescribing-without you needing a new appointment.
What’s the ARMOR tool, and how do I use it?
ARMOR stands for Assess, Review, Minimize, Optimize, and Reassess. It’s a simple framework for managing multiple medications. First, assess all your drugs. Review why each was prescribed. Minimize anything that’s not clearly needed. Optimize the rest by checking for interactions. Reassess every few months. Many clinics use it, and you can use it at home with your list and a pharmacist.
Is polypharmacy just an older person’s problem?
No. While it’s most common in older adults, younger people with chronic conditions-like diabetes, autoimmune diseases, or mental health disorders-are also at risk. Anyone on five or more meds should review them regularly. It’s not about age-it’s about complexity.
Write a comment
Your email address will not be published.






14 Comments
This is the kind of post that should be mandatory reading for every doctor who writes prescriptions without a full med review. I've seen too many elderly patients on 12 pills just because no one ever asked if they still needed them. It's not medicine-it's medical laziness.
I work with seniors every day and this checklist is exactly what we need to hand out at every clinic visit. People don't realize that the dizziness they chalk up to aging is often just a reaction to mixing their blood pressure med with a sleep aid they got from the corner store. The Beers Criteria isn't some obscure guideline-it's a lifesaver if you actually use it. I printed this out and put it on the fridge next to my mom's pill organizer. She still takes diphenhydramine for sleep and I'm going to bring it up at her next appointment. No more Benadryl for Grandma.
Just had my MUR last week. Went in with 11 meds. Came out with 6. The pharmacist didn't judge. Just asked why I was still taking that old anxiety med from 2012. Turns out my doctor forgot to take me off it after I stopped therapy. Free, easy, and way more helpful than my last three doctor visits combined. Everyone should do this. Seriously.
Polypharmacy? More like pharmaceutical capitalism in action. 🧪💊
Of course the system is broken. Big Pharma funds every medical school. Your doctor doesn't know what's in your cabinet because they're paid to push scripts, not to think. This isn't healthcare-it's a subscription service for pills.
So we're supposed to believe that the same doctors who prescribed us all these pills are now going to magically stop doing it because some Reddit post told us to? Please. The system doesn't care if you live or die. It only cares if you keep buying.
Wait-so you're telling me the government, the FDA, and every doctor in America are all secretly in cahoots to poison old people? That’s the only explanation. I’ve been saying this for years. They’re putting fluoride in the water AND the pills. It’s all connected.
The notion that pharmacists are somehow better equipped to manage polypharmacy than physicians is not only empirically unsound, it reflects a dangerous erosion of clinical hierarchy. The physician is the steward of the therapeutic plan-not the dispenser of pills who happens to have a PharmD.
The ARMOR framework? How quaint. In the era of pharmacogenomics and AI-driven polypharmacy risk stratification, this is like using a slide rule to calculate orbital mechanics. The real issue is systemic fragmentation of care, not some checklist that ignores dynamic biomarkers and real-time EHR integration.
I showed this to my dad and he finally agreed to drop his old pain med. He’s been walking better and not napping all day. Honestly? This post saved his life. Thanks for writing it. We need more of this stuff.
My mother died because of this. She was on 14 meds. No one ever reviewed them. She fell. Broke her hip. Went to the hospital. Got sedated. Never woke up. I didn't know any of this was preventable. If I'd known, I would've fought harder. Don't wait until it's too late.
this is all a lie the pharmas are mind controllin us with the pills u think u need em but u dont they put stuff in the water and the pills to make u dependant its all a scam and the docs are paid by big pharma to keep u on it dont trust anyone
The real tragedy isn't polypharmacy-it's the epistemic collapse of clinical judgment. We've outsourced decision-making to algorithms, checklists, and pharmacy interns while abandoning the art of patient-centered therapeutics. The Beers Criteria is a band-aid on a hemorrhage. What we need is a return to phenomenological prescribing: understanding the patient's lived experience, not just their pill count.
I'm a pharmacist and I see this every day. The best thing you can do? Bring your list to your pharmacist and say, 'I want to live better, not just survive.' We can help you cut the clutter without losing the care. No judgment. Just facts. And yes, grapefruit juice really does mess with statins. I've seen it turn people into ICU patients. Don't be that person.