Renal Dosing Calculator for Elderly Patients
Patient Input
Dosing Guidance
Cockcroft-Gault CrCl
--
MDRD eGFR
--
Renal Function Category:
--Dosing Strategy:
--Recommended Dose:
Important: For narrow therapeutic index drugs (digoxin, lithium, phenytoin), serum level monitoring is essential.
High-Risk Medications
- Digoxin: 0.25 mg daily (>60 mL/min), 0.125 mg daily (30-60 mL/min)
- Lithium: 300 mg daily (30-60 mL/min)
- Cefepime: 1 g IV q8h (30-50 mL/min), 1 g IV q12h (10-29 mL/min)
- Allopurinol: 100-200 mg daily (30-60 mL/min)
- Metformin: 500 mg BID (30-45 mL/min)
- Gabapentin: 100-300 mg daily (30-60 mL/min)
Elderly Renal Impairment is a condition where an older adult’s kidneys can no longer filter blood efficiently, usually defined as a glomerular filtration rate (GFR) below 60 mL/min/1.73 m². When this happens, the way the body handles medicines changes dramatically, and a dose that’s safe for a younger adult can become poisonous for a senior.
In the UK, roughly one‑third of people over 65 have chronic kidney disease at stage 3 or worse, according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). That means clinicians are constantly juggling two goals: keep the drug effective while stopping toxicity dead in its tracks.
Understanding Kidney Function in Older Adults
The first step is to know exactly how well the kidneys are working. Two numbers are most useful:
- Creatinine Clearance (CrCl) - calculated from serum creatinine, age, weight, and sex.
- Estimated GFR (eGFR) - derived from equations that also factor in race and body surface area.
Why do we need both? Creatinine‑based formulas tend to underestimate true kidney function in seniors by 15‑20 % (BMC Nephrology, 2013). That under‑estimation can lead to unnecessary dose cuts, leaving the patient under‑treated.
How to Estimate Renal Function - The Equations That Matter
Three equations dominate clinical practice:
- Cockcroft‑Gault (CG) equation - [(140 - age) × weight kg] ÷ (72 × serum creatinine) with a 0.85 factor for women. It’s the go‑to for most drug‑dosing tables because it gives a direct CrCl.
- Modification of Diet in Renal Disease (MDRD) equation - estimates GFR using serum creatinine, age, sex, and race. Good for confirming borderline CG results.
- CKD‑EPI / cystatin C‑based formulas - preferred when GFR is above 60 mL/min/1.73 m² or when muscle mass is low, as often seen in frail elders.
Practical tip: for patients with a CrCl between 25‑59 mL/min, KDIGO recommends using CG as a conservative estimate, then double‑check with MDRD if the result sits right on a dosing cut‑off.
Renal Dosing Guidelines - What the Major Bodies Say
The Kidney Disease: Improving Global Outcomes (KDIGO) 2011 Drug Dosing Report remains the backbone of most hospital protocols. It splits dose adjustments into three strategies:
| Strategy | When to Use | Typical Change |
|---|---|---|
| Dose Reduction | Linear‑clearance drugs (e.g., gabapentin) | Reduce total daily dose proportionally to CrCl drop |
| Interval Extension | Time‑dependent drugs (e.g., vancomycin) | Keep same dose but give it less often |
| Combination | Drugs with both concentration‑ and time‑dependent components (e.g., piperacillin/tazobactam) | Both dose and interval are altered |
For a quick mental shortcut, many clinicians use the “50 % rule”: cut the dose in half or double the interval when CrCl < 50 mL/min. KDIGO warns this oversimplifies about 22 % of high‑risk meds, especially those with nonlinear kinetics.
High‑Risk Medications & Practical Dosing Charts
Below are the drugs that regularly show up in adverse‑event reports for seniors with CKD. The numbers reflect the most recent consensus from KDIGO, ASHP, and specialty societies.
| Medication | CrCl Range (mL/min) | Adjusted Dose / Interval |
|---|---|---|
| Digoxin | > 60 | 0.25 mg daily |
| Digoxin | 30‑60 | 0.125 mg daily |
| Digoxin | <30 | 0.125 mg every 48 h |
| Lithium | > 60 | 300 mg BID |
| Lithium | 30‑60 | 300 mg daily |
| Lithium | <30 | 150 mg daily |
| Cefepime | > 50 | 1 g IV q6h |
| Cefepime | 30‑50 | 1 g IV q8h |
| Cefepime | 10‑29 | 1 g IV q12h |
| Cefepime | <10 | 1 g IV q24h |
| Allopurinol | > 60 | 300 mg daily |
| Allopurinol | 30‑60 | 100‑200 mg daily |
| Allopurinol | <30 | 100 mg every other day |
| Metformin | > 45 | 500‑850 mg BID |
| Metformin | 30‑45 | 500 mg BID |
| Metformin | <30 | Contraindicated |
| Gabapentin | > 60 | 300‑1200 mg daily |
| Gabapentin | 30‑60 | 100‑300 mg daily |
| Gabapentin | <30 | 100 mg daily |
These tables are meant to be printed and kept on the ward. Always confirm the patient’s most recent labs before finalizing the order.
Implementing Safe Dosing in Clinical Practice
Even the best guidelines fail if they never reach the bedside. Here are three proven tactics:
- Pharmacist‑Led Review: A Mayo Clinic study showed a 58 % drop in adverse drug events when a clinical pharmacist ran all renal dose checks for patients over 65.
- Electronic Alerts: The University of Nebraska Medical Center’s EHR alerts cut inappropriate dosing by 37 % in a year‑long rollout.
- Point‑of‑Care Calculators: Apps like Epocrates Renal Dosing (1.2 M downloads Q2 2023) give instant CG numbers and suggested doses, reducing errors by ~40 %.
In each case, the key is “just‑in‑time” information - the clinician should never have to pull up a PDF while the patient is waiting.

Emerging Tools & Future Directions
The market is finally catching up. In 2023 the FDA cleared DoseOptima, an AI‑driven platform that pulls the latest labs, runs a cystatin C‑based equation, and spits out a dose recommendation in seconds. A multicenter trial reported 92.4 % accuracy across 15,000 encounters.
Beyond AI, pharmacogenomics is poised to add another layer. The NIH’s Pharmacogenomics Research Network is recruiting seniors for a study on transporter gene variants that affect renal clearance of drugs like dabigatran and levetiracetam. Results could eventually let us personalize the CrCl cut‑offs for each patient.
Regulators are also tightening the net. The EMA’s 2017 guideline mandates explicit dosing tables for every CrCl bracket below 60 mL/min, and the FDA’s 2019 geriatric pharmacology guidance now requires renal‑adjustment language on all new drug labels targeting adults over 65.
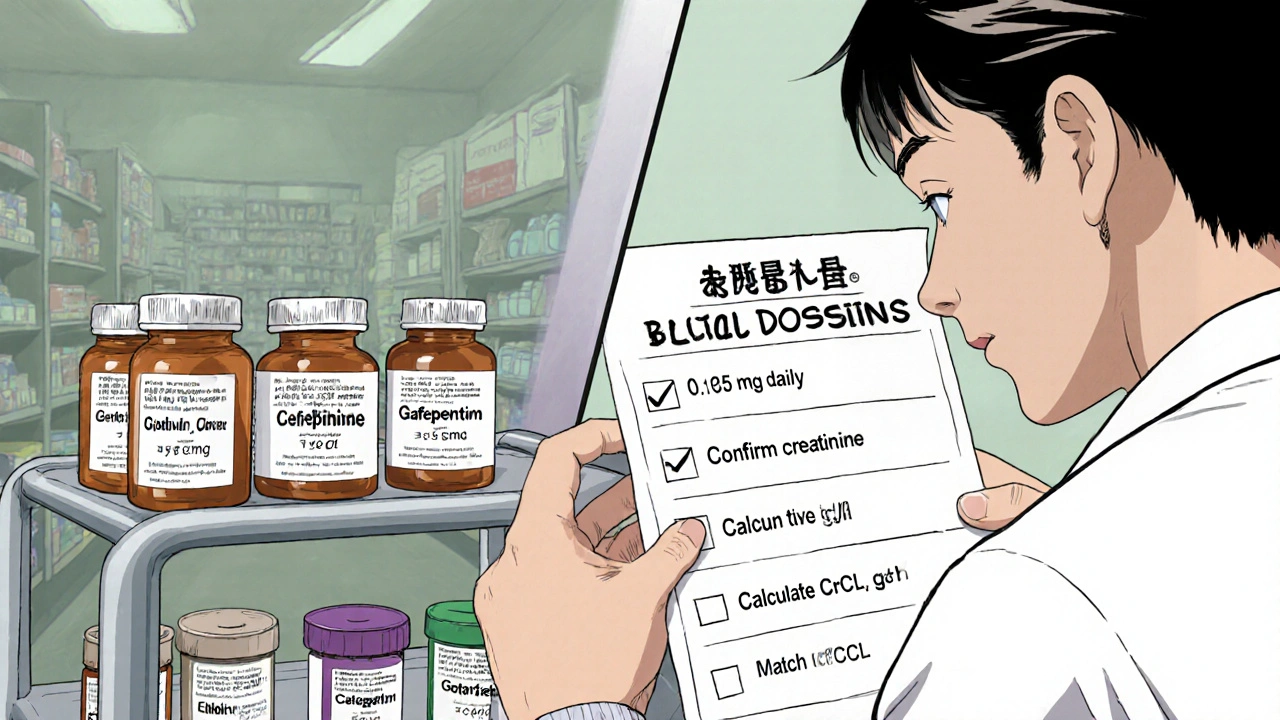
Quick Checklist for Busy Clinicians
- Confirm the latest serum creatinine and weight.
- Calculate CrCl with Cockcroft‑Gault (use actual body weight unless BMI > 30, then use adjusted weight).
- Match the patient’s CrCl to the appropriate dosing strategy (reduction, interval, or combo).
- Check the drug’s therapeutic index - narrow‑window drugs (digoxin, lithium, phenytoin) need serum level monitoring.
- Document the calculation and dose decision in the chart.
- Set a reminder to repeat labs in 48‑72 hours for new starts or dose changes.
Frequently Asked Questions
How accurate is Cockcroft‑Gault for patients over 80?
It tends to underestimate true renal function by 15‑20 %. Use it as a conservative baseline, then verify with MDRD or a cystatin C‑based estimate if the dose sits near a critical cut‑off.
When should I avoid a medication altogether?
If the drug’s clearance is > 50 % renal and the patient’s CrCl is < 30 mL/min, most guidelines recommend either a drastically reduced dose or complete avoidance. Examples include glyburide, gabapentin at high doses, and certain aminoglycosides.
Do I need to adjust doses for oral versus IV meds?
Yes, but the adjustment factor can differ. IV drugs often have higher peak concentrations, so interval extension is more common. Oral agents usually follow dose reduction.
What monitoring is required after a dose change?
Re‑check serum creatinine within 48-72 hours, then repeat drug‑specific levels (e.g., digoxin, lithium) after the expected steady‑state period - typically 5-7 days for digoxin, 3-5 days for lithium.
Are there any mobile apps you recommend?
Epocrates Renal Dosing, Medscape’s Renal Dosing Calculator, and the FDA‑approved DoseOptima (AI‑driven) are all validated and widely used in hospital settings.
By treating renal function as a dynamic, patient‑specific variable and pairing that knowledge with the right tools, clinicians can keep older adults on the therapies they need without inviting toxicity.
Write a comment
Your email address will not be published.





13 Comments
When I first saw the dosing tables, I felt like I’d stumbled onto a secret weapon for our frail patients! The way the Cockcroft‑Gault equation slots right into everyday prescribing is pure gold. I love how the article reminds us to double‑check with MDRD before making any cut‑off decisions. It’s a reminder that every milligram matters when kidneys are on the fritz. Let’s keep sharpening those calculators!
Stop treating the formulas as optional accessories – they’re the backbone of safe practice. Grab a pen, run the CG, then cross‑reference with MDRD; if the numbers clash, err on the side of caution. Ignoring that step is practically inviting toxicity. The evidence isn’t vague; it’s crystal clear. Align the team around this workflow and watch adverse events plunge.
Kidney dosing is a dance between chemistry and compassion we can’t afford to ignore the numbers guide us but also ask what the patient feels about their meds the balance is key
💡 Good point about the “50 % rule” – it’s handy for quick mental math but you really have to remember it misses about a fifth of high‑risk drugs. Keep an eye on those narrow‑window meds like digoxin and lithium, and the rule of thumb becomes a safety net rather than a blanket. 😊
Totally agree, the rule works for a lot of meds but once you get into the nonlinear kinetics world you need a more nuanced approach. I always flag digoxin, lithium, and certain aminoglycosides for a separate level‑checking step, and it saves us from those scary serum‑level spikes. Thanks for highlighting the nuance!
💢 If you’re still relying on a blanket “cut the dose in half” mentality, you’re doing a disservice to your patients. The guidelines exist for a reason – there’s a reason the KDIGO panel spent years polishing those charts. Ignoring them is amateur hour.
i cant stress enough how much double checking that crcl number can save u from a whole lotta trouble. dont just trust the first calc u get.
Ah, the naïve optimism of “just double‑check” when the very act of calculation is steeped in centuries of renal physiologic lore. One must contemplate the epistemic humility required to admit that no single equation reigns supreme, lest we drift into the abyss of iatrogenic harm.
Honestly, I think the whole emphasis on equations is a bit overblown – we’re turning patients into spreadsheets. Real‑world clinicians know when a drug just feels off; numbers can’t capture that intuition.
While intuition plays a role, discarding validated dosing algorithms in favor of “feelings” risks systematic bias and repeatable errors. The literature consistently shows reduced toxicity when clinicians adhere to the CKD‑EPI or CG recommendations, especially for narrow‑window agents.
Renal dosing in the elderly is a multifaceted challenge that extends beyond simply plugging numbers into an equation. First, the physiological changes of aging-decreased renal mass, altered perfusion, and reduced tubular secretion-shift the pharmacokinetic landscape in ways that are not fully captured by creatinine alone. Second, the variability in muscle mass among seniors means serum creatinine can be misleading, prompting the need for cystatin C or combined formulas when accuracy is paramount. Third, the therapeutic index of many commonly used drugs, such as digoxin, lithium, and certain antibiotics, is narrow enough that even modest miscalculations can precipitate serious toxicity. Fourth, drug‑drug interactions compound the problem; for example, concomitant NSAID use can further impair renal clearance, necessitating an additional dose reduction. Fifth, the timing of laboratory draws relative to acute illness can cause transient spikes in creatinine that, if taken at face value, may lead to unnecessary dose cuts and subtherapeutic exposure. Sixth, the practice of “dose capping” without individualized assessment can create a false sense of safety while ignoring patient‑specific GFR trends. Seventh, many institutions still rely on legacy dosing tables that were derived from younger, healthier populations and have not been updated to reflect contemporary geriatric pharmacology. Eighth, electronic health record alerts, while helpful, often suffer from alert fatigue, causing clinicians to override or ignore critical renal dosing warnings. Ninth, regular re‑assessment of renal function-ideally every 48‑72 hours after initiating or adjusting a renally cleared medication-ensures that dosing remains aligned with the patient’s dynamic status. Tenth, therapeutic drug monitoring for agents like vancomycin, digoxin, and lithium provides an additional safety net that complements equation‑based dosing. Eleventh, patient education is essential; seniors and caregivers should understand the signs of toxicity so they can seek care promptly. Twelfth, interdisciplinary collaboration, especially involving pharmacists, enhances the accuracy of dose calculations and monitoring plans. Thirteenth, when confronting a borderline CrCl value, the conservative approach of using the lowest recommended dose can prevent adverse events without significantly compromising efficacy. Fourteenth, incorporating point‑of‑care tools, such as mobile dosing calculators validated for older adults, streamlines the workflow and reduces manual errors. Finally, a culture that prioritizes renal safety, reinforces guideline adherence, and encourages continuous learning will ultimately safeguard our elderly patients from avoidable medication harm.
✍️ Ah, yes, the exhaustive dissertation that could easily be distilled into a single bullet point: “Don’t forget to check the kidneys.” One might wonder why we labor through such verbosity when a concise reminder would suffice. Nevertheless, your commitment to detail is, if not charming, certainly thorough. 🙃
Remember to document the CrCl calculation and the chosen dosing adjustment in the patient’s chart.