When your knee swells up after a long walk, or your shoulder locks up from lifting groceries, corticosteroid injections - often called cortisone shots - are one of the most common treatments doctors reach for. They work fast. For many people, the relief is real. But they’re not a cure. And if you use them too often, they can make things worse.
How Corticosteroid Injections Actually Work
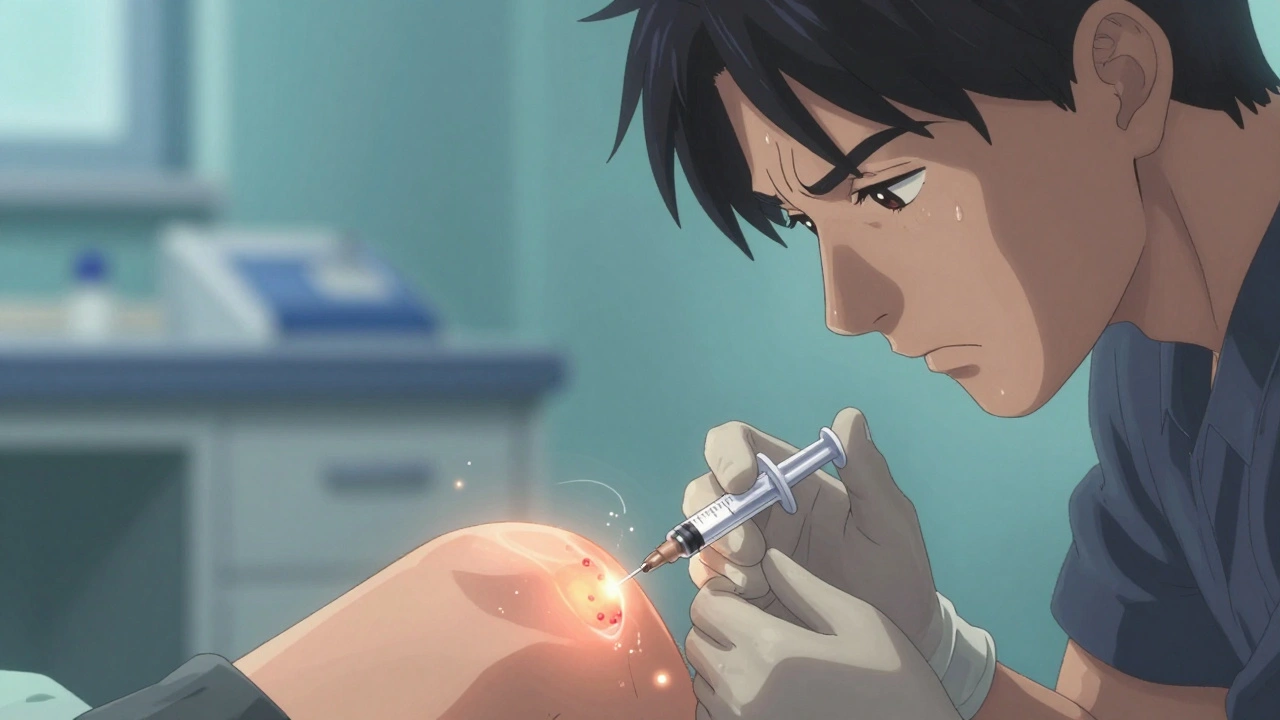
Corticosteroid injections don’t fix damaged cartilage or worn-out tendons. What they do is silence the inflammation that makes your joint hurt. Inside your joint, immune cells release chemicals like interleukin-1 and tumor necrosis factor-alpha. These trigger swelling, heat, and pain. Corticosteroids stop those signals. They bind to receptors in your cells, turn down the genes that cause inflammation, and reduce the number of white blood cells flooding the area.
Most injections mix a corticosteroid - like triamcinolone acetonide or methylprednisolone acetate - with a local anesthetic like lidocaine. The anesthetic gives you immediate relief, while the steroid takes 24 to 72 hours to kick in. The dose depends on the joint. A knee might get 40 to 80 mg. A finger joint? Maybe 10 mg. Too much in a small space can cause tissue damage.
Studies show these injections reduce synovial fluid volume, stabilize cell membranes, and lower prostaglandin levels - all of which calm the inflammation. But they don’t rebuild cartilage. They don’t repair a torn meniscus. They just quiet the noise.
Who Benefits Most From These Injections?
If you have sudden, sharp pain from gout, bursitis, or tendonitis, corticosteroid injections are often the best first step. A 2023 meta-analysis found patients with acute inflammatory conditions saw noticeable pain relief within 48 hours - and many stayed pain-free for 4 to 6 weeks.
People with rheumatoid arthritis flares, tennis elbow, or hip bursitis often report dramatic improvements. One patient from the Arthritis Foundation forum returned to competitive golf just 10 days after a hip injection, with 70% less pain for 12 weeks. That kind of result isn’t rare.
Doctors also use these shots as a diagnostic tool. If your shoulder pain disappears after an injection, it’s likely coming from the joint itself. If it doesn’t, the problem might be your neck or rotator cuff. That’s valuable info for planning next steps.
What the Evidence Says About Long-Term Use
Here’s the catch: the benefits don’t last. After 6 weeks, most studies show no difference between people who got corticosteroid injections and those who got saline. At 24 weeks? No benefit at all.
A 2023 study tracking patients with osteoarthritis found those who got repeated knee injections had over 3 times the risk of cartilage loss compared to those who didn’t. Continuous users? Nearly 5 times higher risk. That’s why the American College of Rheumatology now advises against these injections for advanced osteoarthritis.
And it’s not just cartilage. Repeated shots can weaken tendons. There are documented cases of Achilles tendon ruptures after multiple ankle injections. Rotator cuff tears have worsened after shoulder cortisone shots. The FDA added warnings about this in 2021.
Experts agree: limit injections to 3 or 4 per joint per year. Some say every 3 months is safe. But if you’re needing them more often, it’s a sign you need a different plan - not another shot.

Cost, Alternatives, and What’s New
A single corticosteroid injection costs between $100 and $300 without insurance. Compare that to PRP ($500-$1,500) or hyaluronic acid (viscosupplementation) at $500-$1,000. Corticosteroids win on price and speed.
But alternatives are catching up. Platelet-rich plasma (PRP) and stem cell therapies are growing fast - up 37% annually from 2019 to 2022. They don’t work as fast, but some studies suggest they might slow degeneration. Still, no strong evidence yet that they beat corticosteroids for short-term relief.
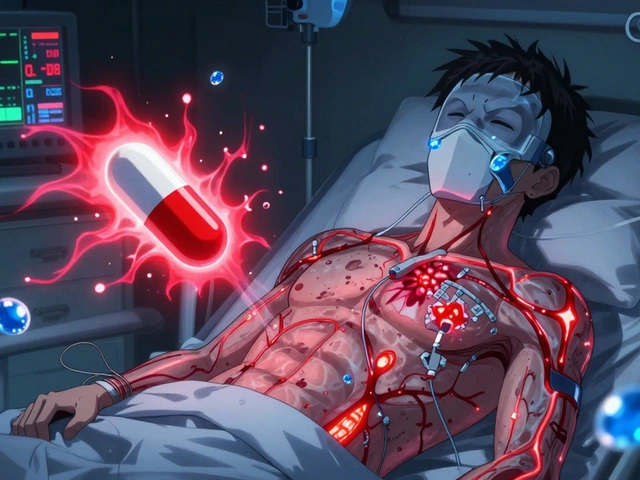
One big development: Zilretta, an extended-release form of triamcinolone acetonide approved by the FDA in 2023. In trials, 45% of patients with knee osteoarthritis had pain relief for 12 weeks - double the rate of standard injections. It’s promising, but it’s not a magic bullet. It still carries the same risks.
The Real Risks Nobody Talks About
Most people hear about temporary pain flares or skin thinning. But there are quieter dangers.
Diabetics can see blood sugar spike for up to 72 hours after an injection. If you’re on insulin or metformin, check your levels daily for 3 days. One patient in Manchester reported needing extra insulin for a week after a knee shot - something her doctor never warned her about.
Then there’s infection risk. A 2023 study found patients who got corticosteroid injections within 3 months before knee or hip replacement had more than double the chance of post-surgery joint infection. Surgeons now avoid giving these shots within 6 months of planned surgery.
And let’s not forget the psychological trap. When a shot works, it’s tempting to keep going back. But each one chips away at the joint’s natural defenses. You’re not treating the problem - you’re just masking it.

What to Do Before and After the Shot
Don’t walk into a clinic expecting a quick fix. Ask these questions:
- What’s the exact diagnosis? Is it inflammation, or is it structural damage?
- Will you use ultrasound guidance? Blind injections miss the target up to 30% of the time.
- What’s the planned dose? Too high for small joints can cause harm.
- What’s the plan if this doesn’t work?
After the shot:
- Avoid heavy lifting or strenuous activity for 48 hours. Movement can spread the steroid unevenly.
- Use ice for 15 minutes every few hours if you feel a flare-up - it happens in 2-8% of cases.
- Track your pain. If it gets worse after 3 days, call your doctor.
- Start physical therapy. Injections give you a window. Use it to strengthen the joint.
When to Say No
There are times when corticosteroid injections are a bad idea:
- You have uncontrolled diabetes - the blood sugar spike can be dangerous.
- Your joint is already severely worn out - injections won’t help and may accelerate damage.
- You’re planning joint surgery in the next 6 months.
- You’ve had 3 or more injections in the same joint in the past year.
- Your pain is constant, not flare-based - this suggests structural, not inflammatory, damage.
If you’ve tried 2-3 injections with diminishing returns, it’s time to switch strategies. Focus on weight management, low-impact exercise, bracing, or physical therapy. These don’t give instant relief - but they fix the root cause.
Final Thoughts
Corticosteroid injections are powerful tools - but they’re not for everyone. They’re best used like a fire extinguisher: quick, targeted, and only when there’s an actual fire. If your joint pain is from wear and tear, no amount of steroid will rebuild what’s broken.
They work great for acute flares. They’re not meant for chronic pain. If you’re relying on them every few months, you’re not managing your condition - you’re delaying the real work: strengthening your body, protecting your joints, and changing how you move.
There’s no shame in needing one. But there’s risk in using them too often. Listen to your body. Ask questions. And don’t let a quick fix become a long-term crutch.
How long does a cortisone shot last in a joint?
Most people feel relief for 2 to 6 weeks. Some get up to 12 weeks with extended-release versions like Zilretta. But after 6 weeks, the effect fades. Studies show no significant benefit beyond 24 weeks. If the relief lasts longer than 3 months, it’s unusual - and worth discussing with your doctor.
Can cortisone injections damage your joint?
Yes. Repeated injections - especially more than 3 or 4 per year - can weaken tendons, break down cartilage, and increase the risk of osteonecrosis. The FDA added warnings about this in 2021. One study found patients with repeated knee injections had nearly 5 times higher risk of cartilage loss over time. They’re safe when used sparingly, but harmful with overuse.
Do cortisone shots work for osteoarthritis?
They can help with pain from osteoarthritis flares, but they don’t slow the disease. For early or mild osteoarthritis, they may offer short-term relief. But for advanced cases, guidelines from the American College of Rheumatology now recommend avoiding them entirely - they don’t help and may speed up joint damage.
Is ultrasound guidance necessary for joint injections?
It’s not always required, but it’s much more accurate. Blind injections miss the target in up to 30% of cases. With ultrasound, accuracy jumps to 95%. This means better results and fewer complications. If your doctor doesn’t use imaging, ask why - especially for shoulder, hip, or wrist injections.
Can I get a cortisone shot if I have diabetes?
Yes, but with caution. Corticosteroids can raise blood sugar levels for up to 72 hours. Diabetics should monitor glucose closely after the injection and may need to adjust insulin or medication temporarily. Talk to your endocrinologist or primary care provider before the shot. Don’t skip this step - uncontrolled spikes can lead to serious complications.
What are the side effects of cortisone injections?
Common side effects include temporary pain or swelling at the injection site (a flare), skin thinning or lightening, and elevated blood sugar. Less common but serious risks include tendon rupture, joint infection, and accelerated cartilage loss. In rare cases, there’s facial flushing, insomnia, or mood changes. Most side effects are mild and short-lived - but repeated use increases risk.
How many cortisone shots can I get in a year?
Most guidelines recommend no more than 3 to 4 injections per joint per year. Some doctors allow one every 3 months. But if you’re needing them more often, it’s a red flag. It means the underlying issue isn’t being addressed. At that point, physical therapy, lifestyle changes, or other treatments should be the focus.
Are cortisone shots better than physical therapy?
They serve different purposes. Cortisone gives fast pain relief. Physical therapy builds strength, improves movement, and addresses root causes. Studies show combining both works best: get the shot to reduce pain, then start therapy to prevent it from coming back. Relying only on shots leads to more damage over time. Therapy takes longer, but it lasts.
Write a comment
Your email address will not be published.


13 Comments
Been getting these for my knee since 2020. First two were magic. Third one? Barely touched the pain. Fourth? Made it worse for a week. Now I just do PT and walk like a grandpa. No judgment - just facts.
As someone who’s managed RA for 14 years, I can say this: cortisone is a bridge, not a home. I’ve had 3 shots in my right shoulder this year - and yes, I’m now doing daily resistance bands and yoga. The relief is real, but the dependency? Dangerous. Don’t let the quick fix become your only tool.
Oh, sweet merciful heavens - yet another mainstream piece that treats corticosteroids like a magic bullet while ignoring the grotesque cascade of iatrogenic devastation. We’re not just talking cartilage erosion here. We’re talking tendon necrosis, adrenal suppression, metabolic chaos, and the silent erosion of joint integrity over time. And yet, the ortho docs keep reaching for the syringe like it’s a damn placebo button. It’s not medicine - it’s temporal bandaging with a side of iatrogenic tragedy.
Let’s be brutally honest: the entire medical-industrial complex profits from repetitive corticosteroid injections. Insurance covers them. Surgeons get paid per injection. Physical therapy? Reimbursed at 1/5 the rate. The data is clear - after 3 injections, outcomes plateau or worsen. Yet clinics still push them because they’re profitable, not because they’re principled. This isn’t healthcare - it’s revenue optimization disguised as relief. And patients? They’re the collateral damage in a system that rewards short-term fixes over long-term outcomes.
They’re just trying to keep you doc-dependent so they can sell you more drugs later. 🤡
It’s fascinating how we treat inflammation like an enemy to be annihilated, rather than a signal to be understood. Corticosteroids don’t heal - they silence. But what are we missing when we mute the body’s alarm system? Chronic pain isn’t always a malfunction - sometimes it’s the last honest thing left in a joint that’s been ignored for years. Maybe the real question isn’t ‘how often can I get a shot?’ but ‘why did this happen in the first place?’
In India, we often rely on traditional remedies - turmeric paste, warm oil massages, Ayurvedic therapies - before even considering injections. I’ve seen elders with severe knee pain walk without discomfort after months of consistent practice. Not instant, but sustainable. Western medicine excels at speed, but Eastern traditions teach patience. Perhaps the answer lies not in choosing one over the other, but in integrating wisdom from both worlds.
DIABETICS BEWARE 😱 I got one last month and my sugar went to 320. My endo was PISSED. 🤬 Don’t be me.
Given the pharmacokinetics of intra-articular triamcinolone acetonide, the localized concentration gradient induces a transient suppression of NF-κB signaling pathways, thereby downregulating pro-inflammatory cytokine transcription. However, prolonged exposure leads to apoptosis of chondrocytes via mitochondrial dysfunction and oxidative stress, as evidenced by elevated caspase-3 expression in synovial fluid biopsies. The clinical implication is clear: repeated administration compromises structural integrity beyond the threshold of compensatory repair mechanisms. This necessitates a paradigm shift from palliative intervention to regenerative rehabilitation protocols.
I’ve been a physio for 22 years. I’ve seen hundreds of patients come in with ‘one last shot’ and then come back six months later with worse pain and no mobility. The truth is, injections don’t make you stronger - they just make you quiet. The real work? Movement. Stability. Loading the joint properly. If you’re not doing any rehab after the shot, you’re not healing - you’re just delaying the inevitable. I wish more doctors would say that out loud.
My buddy got a cortisone shot for his tennis elbow, did zero PT, and now he can’t lift his coffee cup. Don’t be that guy. Get the shot if you need it - then hit the gym. Strengthen the damn muscles around the joint. That’s the only thing that’ll keep you moving for the next 20 years. Shots are a reset button, not a cheat code.
It is imperative to underscore that the administration of corticosteroid injections, while clinically efficacious in the short-term modulation of inflammatory mediators, constitutes a therapeutic intervention that must be strictly contextualized within a multidisciplinary management framework. Absent concurrent implementation of biomechanical correction, neuromuscular re-education, and lifestyle modification, such interventions risk exacerbating underlying degenerative pathology. Therefore, the standard of care must evolve beyond episodic pharmacological palliation toward sustained, patient-centered rehabilitative paradigms.
^^^ This. I got my shot, then started doing squats with a chair. Three months later, I can climb stairs without wincing. No magic. Just consistency.