When you start a new medication, it’s normal to feel unsure about what’s happening in your body. Maybe you feel a little dizzy after taking your blood pressure pill. Or your stomach feels upset after your antibiotic. You might wonder: is this a side effect, or could it be a dangerous allergy? The difference matters - not just for how you feel today, but for what medications you can safely take for years to come.
Side Effects and Allergies Are Not the Same
Side effects are predictable reactions to a drug. They happen because the medication affects more than just the target area in your body. For example, statins can cause muscle aches in 5-10% of people. Antibiotics like amoxicillin often lead to diarrhea because they disrupt gut bacteria. These aren’t emergencies. They’re common, and often get better after a few days or weeks as your body adjusts. About 60-70% of initial side effects fade within 2-4 weeks, according to WebMD’s 2023 update. Allergic reactions are different. They’re your immune system overreacting to the drug as if it’s a threat. This can happen even with a tiny dose. Symptoms include hives, swelling of the lips or throat, trouble breathing, or a sudden drop in blood pressure. These are red flags. If you have any of these, stop the medication and get help right away. Penicillin is the most commonly reported drug allergy - about 10% of Americans say they have it. But studies show 90% of those people aren’t truly allergic after proper testing. The problem? People mix them up. A 2022 study at UCSF found that 70% of patients call any unpleasant reaction an “allergy.” That leads to doctors avoiding safe, effective drugs and prescribing broader antibiotics instead - which fuels antibiotic resistance. In fact, people labeled with a penicillin allergy get 63% more of these stronger antibiotics, according to JAMA in 2021.What to Say When You Notice Something New
Don’t wait until your next appointment to speak up. But don’t panic either. The key is to describe what happened clearly. Here’s how:- Timing: When did the symptom start? Within minutes? Hours? Days? Allergies usually show up fast - within 1 to 6 hours after taking the pill. Side effects often creep in over a day or two.
- Symptoms: What exactly did you feel? A rash? Nausea? Headache? Dizziness? Be specific. “I got a red, itchy rash” is better than “I felt weird.”
- Severity: On a scale of 1 to 10, how bad was it? Did it go away when you skipped a dose? Did it come back when you took the next one?
- History: Have you had this before with other meds? Or is this the first time?
Try this script: “I started taking [medication name] on [date]. About [timeframe] later, I got [symptom]. It lasted [duration]. It got worse when I took the next dose. I didn’t have trouble breathing or swelling, but the [symptom] was really uncomfortable.”
Patients who use this kind of detailed description are 89% more likely to get the right diagnosis, according to Mayo Clinic’s 2022 communication analysis. Those who just say “I’m allergic” get misclassified 70% of the time.
Bring Your Meds - Literally
Don’t rely on memory. Bring the actual bottles to your appointment. Your doctor might not know the exact dose or brand you’re taking. Even small differences - like extended-release vs. immediate-release - can change how your body reacts. UCLA Health tracked this and found that when patients brought their physical medication bottles, communication errors dropped by 28%. That’s huge. It means fewer wrong assumptions, fewer missed connections, and better decisions. Also, write down everything you’ve taken - even over-the-counter stuff, supplements, and herbal teas. Some interactions aren’t obvious. For example, grapefruit juice can make statins more potent and increase muscle pain risk. Your pharmacist can help you spot these.
Use a Symptom Log
You don’t need a fancy app. Just a notebook or a notes app on your phone. For three days before your appointment, track:- Date and time you took each medication
- What symptom you felt
- When it started
- How long it lasted
- How bad it was (1-10)
- Whether it improved after skipping a dose
Patients who do this are 3.2 times more likely to get their meds adjusted correctly, according to APG Health’s 2023 study. One patient, a 58-year-old woman on lisinopril, thought her daily headaches were from stress. She logged them and noticed they started exactly 2 hours after her morning pill. Her doctor switched her to a different blood pressure med - and the headaches vanished.
Ask the Right Questions
Don’t just wait for your doctor to explain. Ask these five questions:- Is this a known side effect of this medication? How common is it?
- Could this be a true allergic reaction? What are the warning signs I should never ignore?
- Will this go away on its own, or do I need to stop the drug?
- Are there other medications in a different class that might work without this issue?
- Should I see an allergist to get tested? Especially if it’s penicillin or another antibiotic.
Harvard Health recommends asking: “What are the most common side effects of this drug? And what symptoms mean I need to stop it right away?” That simple shift turns vague worry into clear action.
Why This Matters Beyond Today
Mislabeling a side effect as an allergy doesn’t just affect your next prescription. It can follow you for life. If your chart says “Penicillin Allergy,” every future doctor will avoid it - even if you never had a real reaction. That means you might get a more expensive, more toxic antibiotic instead. And that increases your risk of C. diff infections, kidney damage, or antibiotic-resistant bacteria. A 2023 study in the Journal of General Internal Medicine showed that clinics using structured conversations about side effects vs. allergies reduced unnecessary antibiotic use by 27%. That’s not just better for you - it helps everyone by slowing down antibiotic resistance. The CDC’s 2023 National Action Plan aims to cut medication communication errors by 30% by 2026. You’re part of that solution. When you speak up clearly, you help your care team make smarter choices - for you and for the system.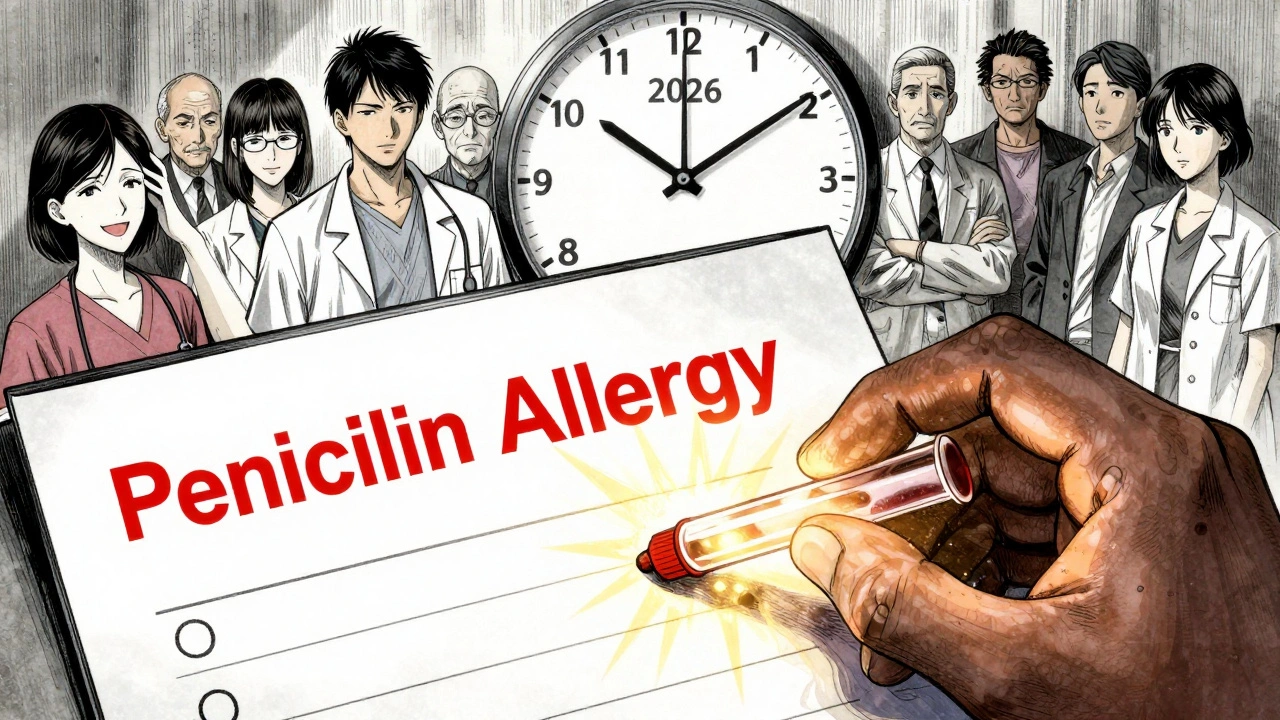
What to Do If You’re Still Unsure
If you’re worried but not sure what’s happening, call your pharmacist. They’re medication experts and often have more time than doctors to walk you through it. Most pharmacies offer free 10-minute consultations. If you had a reaction that felt serious - swelling, trouble breathing, or a widespread rash - don’t wait. Go to urgent care or call 911. Then follow up with your primary doctor to get it properly documented. And if you’ve been told you have a drug allergy but never had testing, ask about an allergy evaluation. Skin tests or graded challenges can confirm whether you’re truly allergic - especially for penicillin, sulfa drugs, or certain painkillers.Bottom Line
You don’t need to be a medical expert to communicate well about your meds. You just need to be specific, honest, and prepared. Track your symptoms. Bring your bottles. Ask the right questions. And don’t let fear silence you.The goal isn’t to avoid every uncomfortable feeling. It’s to know which ones are normal, which ones are dangerous, and which ones can be fixed - without risking your long-term health.
How do I know if my rash is a side effect or an allergic reaction?
A side effect rash is usually mild, flat, and may appear days after starting the medication. It often doesn’t spread quickly and may fade if you skip a dose. An allergic rash is typically raised, itchy, red, and spreads fast. It often shows up within hours of taking the drug and may come with swelling or trouble breathing. If you’re unsure, take a photo and show it to your doctor.
Can I outgrow a drug allergy?
Yes, especially with penicillin. Many people lose their allergy over time - even if they had a reaction decades ago. Studies show that 80% of people who were once allergic to penicillin can tolerate it after 10 years. The only way to know for sure is through a supervised allergy test. Don’t assume you’re still allergic just because you had a reaction in the past.
Should I stop the medication if I think I’m having a side effect?
Don’t stop without talking to your provider first. Some side effects are temporary and go away as your body adjusts. Stopping abruptly can be dangerous - especially with blood pressure meds, antidepressants, or seizure drugs. Instead, log your symptoms and call your doctor or pharmacist. They’ll tell you whether it’s safe to continue, reduce the dose, or switch.
What if my doctor dismisses my concerns?
If you feel unheard, bring your symptom log and medication bottles to your next visit. Ask to speak with a pharmacist or request a referral to an allergist. You have the right to be heard. If your provider still ignores you, consider switching to a provider who takes medication safety seriously. Your health is worth it.
Are there apps that help track side effects vs. allergies?
Yes. The American Pharmacists Association launched the ‘Medication Reaction Tracker’ app in January 2023. It guides you through logging symptoms using clinical criteria to help you distinguish between side effects and true allergies. It’s free, available on iOS and Android, and has been downloaded over 87,000 times. It’s not a substitute for medical advice, but it’s a powerful tool to prepare for your appointments.
Next Steps
If you’re starting a new medication this week:- Write down the name, dose, and reason for the drug.
- Set a reminder to start a symptom log on day one.
- Bring all your meds to your next appointment - even the empty bottles.
- Ask your pharmacist: “What side effects should I watch for? And what’s an emergency?”
- If you’ve ever been told you’re allergic to penicillin or another antibiotic, ask if you can get tested.
Small steps like these can prevent big mistakes. And in medicine, clarity saves lives.
Write a comment
Your email address will not be published.




15 Comments
OMG this is so needed!! I thought I was allergic to ibuprofen because I got a rash once, turns out it was just dehydration and stress lol. So glad someone finally broke this down simply.
It’s fascinating-how the medical system, in its infinite wisdom, has normalized the conflation of ‘unpleasant’ with ‘dangerous’… and yet, we’re not taught to differentiate, because differentiation requires cognitive labor, and cognitive labor is expensive… and capitalism prefers overprescribing over education.
So we get 70% misclassification-not because patients are dumb, but because the system is designed to avoid accountability.
Penicillin? 90% false positives? And yet, every ER still treats you like you’re holding a biological grenade.
It’s not ignorance. It’s institutional inertia.
And now, we’re all just… collateral damage.
Meanwhile, the antibiotics industry keeps raking in billions.
Who benefits?
Not you.
Not me.
Definitely not the microbiome.
It’s a slow, quiet catastrophe.
And we’re all just supposed to… keep taking the pills.
This is excellent guidance. Many patients do not understand the difference between side effect and allergy. Simple, clear communication saves lives. I recommend everyone follow the steps outlined here.
Why do we even need a script for this Isn’t it obvious If you feel weird stop taking it
One thing the article doesn’t emphasize enough is that side effects aren’t always harmless. Muscle pain from statins can progress to rhabdomyolysis. Diarrhea from antibiotics can lead to C. diff. The key isn’t just labeling it-it’s tracking severity and progression. If it’s getting worse, even if it’s not swelling or breathing trouble, it’s not ‘just a side effect.’ It’s a signal. Listen to your body. Document it. Push back if dismissed.
And yes-pharmacists are your secret weapon. They know the interactions, the patterns, the red flags. Use them.
I’ve been a patient for over 30 years, and I can tell you-this is the most comprehensive, compassionate, and clinically accurate guide I’ve ever read on this topic. The emphasis on bringing physical medication bottles? Genius. So many doctors assume you know what you’re taking, but they don’t realize that the bottle says ‘10mg’ and your prescription says ‘20mg’ because the pharmacy switched brands and you didn’t notice. The symptom log? Not just helpful-it’s transformative. I started one after my last ER visit and realized my ‘migraines’ were tied to my beta-blocker, not stress. Changed everything. Also, the question about seeing an allergist? That’s the one most patients never think to ask. Thank you for writing this. It should be required reading for anyone starting any new medication.
YES! I was terrified of my new antidepressant until I started logging. Turns out the nausea went away after 5 days. So glad I didn’t quit!
hmm interesting… i never thought about how mislabeling allergies affects antibiotic resistance… kinda makes you wonder how many other medical assumptions are just… wrong… like, how many people are being denied penicillin because their grandpa had a rash in 1972?
Actually, the real issue is that patients are too lazy to read the insert. The FDA requires detailed side effect disclosures. If you don’t read them, you’re complicit in your own medical ignorance. This article is just a Band-Aid on a systemic failure of personal responsibility.
Can I just say-this is the most important public health message I’ve seen in years? The way we handle medication reactions is broken. We’re treating symptoms like diagnoses. We’re not teaching people to observe, track, and communicate. We’re just telling them to ‘call if it gets worse.’ But ‘worse’ is subjective. What’s ‘worse’ to one person is normal to another. We need standardized language. We need symptom logs in every EHR. We need pharmacists involved from day one. And we need to stop calling every rash an ‘allergy.’ This isn’t just about penicillin-it’s about trust in medicine.
Also, thank you for mentioning the APhA app. I’ve been using it for months. It’s quiet, clinical, and actually helpful. No ads. No fluff. Just data.
THIS!! 😭 I had a rash on amoxicillin and panicked-called my doctor, they said ‘probably not allergic’ and told me to keep taking it. I did. Rash faded in 3 days. Now I’m not afraid of penicillin anymore. Thank you for validating that my experience matters!! 🙏
Let’s be real-this whole ‘side effect vs allergy’ thing is just Big Pharma’s way to keep you on expensive meds while making you doubt your own body. They want you to think ‘oh it’s just a side effect’ so you don’t question why you’re getting dizzy, depressed, or constipated. The real allergy? The system. The real danger? Not taking the pill. They’ll never admit it.
And that ‘symptom log’? It’s a trap. They want you to document everything so they can use it against you later when you sue for side effects. Don’t fall for it.
Just stop taking everything. Go natural. Your body knows better.
Great advice. I use the MedTracker app daily. It syncs with my Apple Health. I’ve caught two potential interactions already-ginkgo with my blood thinner, and grapefruit with my statin. Saved me a hospital trip. Highly recommend.
As a pharmacist, I see this every day. Patients say ‘I’m allergic to everything’-but when we ask for details, it’s usually nausea, dizziness, or fatigue. Those are side effects, not allergies. We need more public education. This article is a step in the right direction.
Look, I get it. People are scared. But this country is falling apart because we treat medicine like a customer service desk. You don’t get to ‘feel weird’ and demand a new drug. You take what’s prescribed. You endure the side effects. That’s how you build character. In my day, we didn’t have apps and logs-we had grit. Now everyone’s running to the pharmacist like it’s a therapy session. Get tough. Your body isn’t a fragile flower. It’s an American machine. Fix it yourself.