Anticoagulant-COVID Treatment Interaction Checker
Check Your Treatment Safety
This tool helps you determine the safest approach when taking blood thinners with COVID treatments based on current clinical guidelines.
Please select your anticoagulant and treatment
Start by choosing your medications to see safety recommendations
When you're on a blood thinner like rivaroxaban, apixaban, or warfarin, and you get sick with COVID-19, your treatment doesn't just get more complicated-it becomes a high-stakes balancing act. The virus doesn't just attack your lungs; it triggers your blood to clot abnormally. At the same time, the very drugs used to treat COVID-like Paxlovid or dexamethasone-can dangerously alter how your blood thinner works. This isn't theoretical. Real patients have bled internally. Others have suffered strokes or pulmonary embolisms because their anticoagulant levels dropped too low. Between 2020 and 2023, emergency visits linked to these interactions jumped by 37% at major U.S. hospitals. If you're taking a blood thinner and catch a respiratory infection, here’s what you need to know-right now.
Why COVID-19 Makes Your Blood Thicker
COVID-19 doesn’t just cause coughing and fever. In severe cases, it turns your bloodstream into a breeding ground for clots. Studies show that about 70% of critically ill patients develop tiny clots in their lung blood vessels, which is why so many end up on ventilators. This isn’t random. The virus triggers massive inflammation, which activates clotting proteins and shuts down natural anticoagulant pathways. The result? A hypercoagulable state. That’s why doctors started giving therapeutic doses of anticoagulants to hospitalized patients-higher than the usual preventive dose. The American Society of Hematology confirmed in 2021 that this approach saves lives. But here’s the catch: once you leave the hospital, your blood doesn’t instantly return to normal. D-dimer levels, a marker for clotting, stay elevated for up to three weeks in two out of three patients. That’s why guidelines now recommend continuing therapeutic anticoagulation for at least seven days after discharge.Paxlovid: The Game-Changer With Hidden Risks
Paxlovid, the antiviral combo of nirmatrelvir and ritonavir, became a lifeline for high-risk patients. It cuts hospitalization risk by nearly 90% if taken early. But ritonavir? It’s a powerful inhibitor of CYP3A4 and P-glycoprotein-two key systems your body uses to break down blood thinners. When you take Paxlovid with a DOAC like rivaroxaban or apixaban, your anticoagulant levels can spike by 3 to 5 times. That’s not a small change. It’s the difference between a safe dose and a dangerous one. A 2022 study in PMC9284020 showed all 12 patients on DOACs who took Paxlovid had dangerously high drug levels. The FDA issued a safety alert in July 2023 after 147 cases of major bleeding were reported between January 2022 and June 2023. One Reddit user shared a case where a man on full-dose rivaroxaban bled into his stomach during Paxlovid treatment and needed two units of blood. It happened because he didn’t know to pause his blood thinner.Warfarin vs. DOACs: Different Rules, Different Risks
Not all blood thinners behave the same. Warfarin is older, requires frequent INR checks, and interacts with many foods and drugs-but ritonavir doesn’t affect it as dramatically. The American College of Cardiology says warfarin can be safely taken with Paxlovid if INR is monitored daily. But DOACs? They’re trickier. Apixaban, rivaroxaban, edoxaban, and dabigatran all rely on the same liver and gut pathways that Paxlovid blocks. That’s why guidelines diverge. In the U.S., the FDA recommends stopping DOACs during Paxlovid treatment. In Europe, some recommend reducing the dose instead. For dabigatran, the European Medicines Agency allows a 75 mg twice-daily dose if creatinine clearance is above 30 mL/min, but only if timed carefully. The U.S. guidelines say avoid it entirely. This confusion isn’t academic. It’s life-or-death. A 2022 study found that 25% of elderly anticoagulated patients fall into the gray zone of kidney function (CrCl 30-50 mL/min), where no clear guidance exists.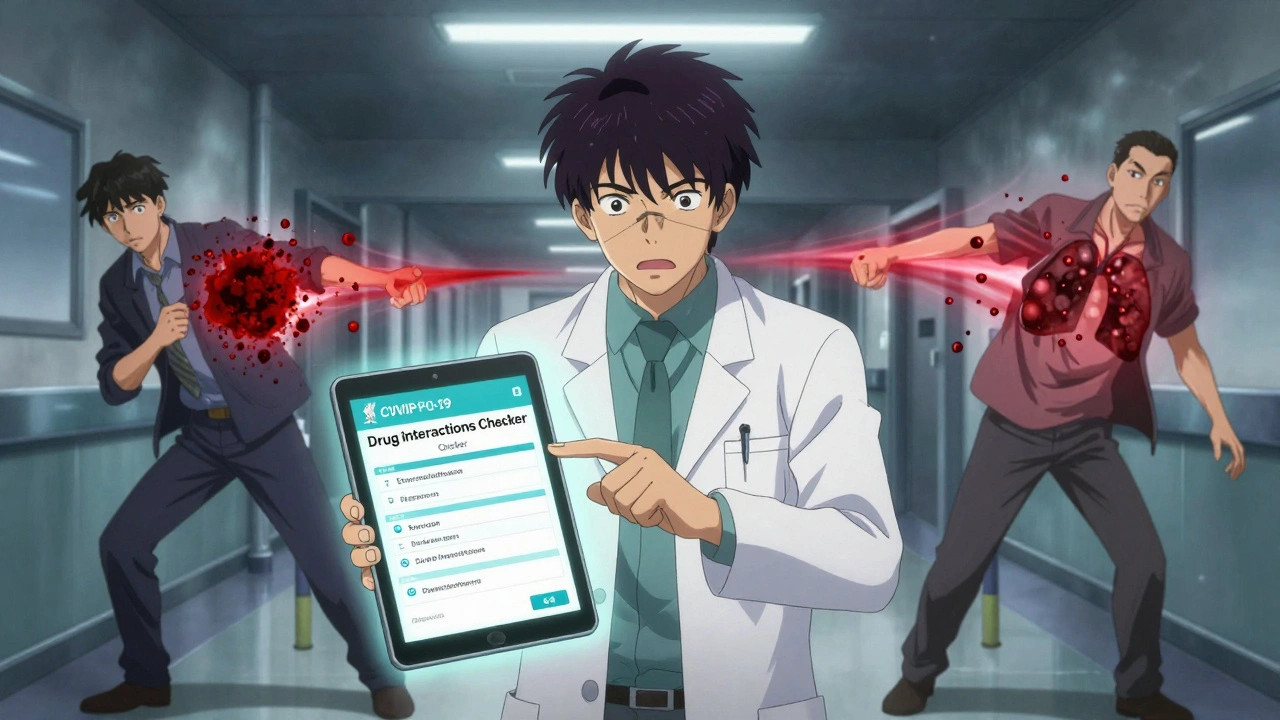
What to Do When You Need Paxlovid
If you’re on a DOAC and test positive for COVID-19, don’t guess. Here’s what works based on current evidence:- For apixaban or rivaroxaban: Stop the DOAC for the full 5 days of Paxlovid treatment. Resume 2 days after the last dose. If your thrombotic risk is high (CHA₂DS₂-VASc score ≥3), ask your doctor about bridging with daily enoxaparin injections during those 5 days.
- For dabigatran: If your kidney function is normal (CrCl ≥50 mL/min), you may take 75 mg twice daily during Paxlovid, but only if you space it at least 12 hours apart from Paxlovid. Otherwise, pause it entirely.
- For warfarin: Continue as usual, but check your INR every day during Paxlovid treatment. Don’t wait a week.
And don’t rely on memory. Use the Liverpool COVID-19 Drug Interactions Checker, updated daily, which has handled over 1.2 million queries since 2020. Pharmacists at Mayo Clinic say this tool alone reduced interaction-related ER visits by 40% in their clinics.
Dexamethasone: The Silent Killer of Anticoagulant Levels
While Paxlovid makes blood thinners too strong, dexamethasone-the steroid used in severe COVID cases-does the opposite. It’s a strong inducer of CYP3A4 and P-gp. That means it speeds up how fast your body clears DOACs. A 2021 study by Testa et al. found dexamethasone can reduce rivaroxaban levels by up to 50%. That’s not a minor drop. It’s enough to leave you unprotected. One patient on apixaban for atrial fibrillation developed a pulmonary embolism after starting dexamethasone, even though he didn’t stop his anticoagulant. His levels had dropped below the therapeutic range. This is why monitoring isn’t optional. Anti-Xa levels for DOACs should be checked every 24-48 hours during steroid treatment. INR for warfarin should be checked daily. If you’re on both Paxlovid and dexamethasone? You’re caught between two extremes-one drug making your blood too thin, the other making it too thick. This is why hospital teams use protocols, not guesswork.
Real-World Mistakes and How to Avoid Them
A 2022 survey by the American Pharmacists Association found that 63% of community pharmacists saw at least one dangerous interaction per month. The most common? Dabigatran and Paxlovid. Patients often don’t realize their blood thinner needs to be paused. Some think, “I’m just taking it for a few days-I’ll be fine.” But the risk isn’t just theoretical. In one case, a 78-year-old woman on rivaroxaban took Paxlovid and developed a GI bleed. She was hospitalized for three days. Her pharmacist hadn’t flagged the interaction because the prescription didn’t include her anticoagulant list. That’s why communication is key. Always tell every doctor, pharmacist, and ER staff you’re on a blood thinner. Bring your pill bottles. Use apps like Medisafe or MyTherapy to track your meds. And if you’re unsure, call your pharmacist before taking anything new. They’re trained for this.What’s Next? Better Tools, Safer Drugs
The industry is responding. Pfizer’s next antiviral, PF-07817883, is in Phase 2 trials and shows almost no CYP3A4 inhibition. That means it might not interfere with blood thinners at all. Meanwhile, machine learning models are being trained to predict interaction risks. A 2023 study in Nature Medicine built a model that predicted severity with 89.4% accuracy using 12,783 patient records. Point-of-care tests for anti-Xa levels are becoming faster and cheaper, making monitoring possible even in outpatient settings. But until those tools are widespread, the rules are simple: When in doubt, pause the DOAC and consult your care team. Don’t wait for symptoms. Bleeding doesn’t always come with warning signs. Clots don’t always cause pain. The safest move isn’t always the easiest one.How to Stay Safe Going Forward
- Keep a current list of all your medications, including doses and reasons you take them. Share it with every provider.Respiratory infections like COVID-19 aren’t going away. Anticoagulants are essential for millions. The challenge isn’t to avoid one or the other-it’s to manage them together. With the right knowledge and a proactive team, you can stay protected without putting yourself at risk.
Write a comment
Your email address will not be published.




11 Comments
This hit me right in the gut. My mom’s on apixaban for AFib, and when she got COVID last winter, her pharmacist had to call the cardiologist at 2 a.m. because the pharmacy system didn’t flag the interaction. She ended up in the ER with a scary drop in INR after dexamethasone. I wish everyone knew how sneaky these drugs are-like silent landmines in your medicine cabinet.
Don’t just trust the script. Bring your bottles. Say it out loud: 'I’m on a blood thinner.' I swear, it saves lives.
Thank you for writing this. My mom’s still here because someone finally told us what to do.
Now I’m making a laminated card for her wallet.
God bless pharmacists.
Wait… so you’re telling me Big Pharma and the CDC are hiding this? Why does every single anticoagulant interaction get buried under ‘clinical guidelines’? I’ve been saying for years that Paxlovid is just a Trojan horse to get people hooked on hospitalizations. Look at the numbers-37% more ER visits? That’s not an accident. That’s a profit margin.
And why are we letting the FDA and EMA contradict each other? Because they’re owned by the same lobby. Wake up. Your blood thinner isn’t the problem. The system is.
I’ve been off all pharmaceuticals for 8 years now. Turmeric and garlic saved me. You think a pill can fix what the virus does? Think again.
And don’t even get me started on dexamethasone. That’s a steroid weaponized by the WHO to suppress immunity. It’s not medicine. It’s control.
It is, without question, a matter of profound concern that individuals entrusted with the management of anticoagulation therapy are not universally equipped with the requisite knowledge to navigate the pharmacokinetic complexities introduced by antiviral agents such as nirmatrelvir/ritonavir. The data presented, while statistically significant, lacks a longitudinal component, and the anecdotal case reports-though compelling-do not constitute a robust evidence base. Furthermore, the recommendation to pause DOACs without clear biomarker-guided resumption protocols introduces a new category of risk: thrombotic events due to therapeutic gaps.
One must ask: who is responsible for ensuring compliance? The patient? The pharmacist? The physician? The algorithm? The answer, I fear, is none of the above.
Regulatory inconsistency across jurisdictions is not confusion-it is negligence.
ok but like… why does paxlovid even exist? i swear every time i hear about someone bleeding out because they took it with their blood thinner i just think… why not just let people get sick and rest? why force a pill on everyone? i had covid and i just drank tea and slept for a week. i’m fine. why do we need these fancy drugs that make you bleed? it’s all just fear selling.
and dexamethasone? that’s just steroid abuse. they give it to everyone like it’s candy. my cousin got it and her face swelled up like a balloon. then they told her to keep taking her blood thinner? nope. nope nope nope.
also why does the liver even matter? i think the government made all these interactions up to sell more tests. i mean… look at the numbers. they jump by 37%? that’s just because they started counting better. not because it’s worse.
It’s wild how something so simple-like taking a pill-can turn into a life-or-death puzzle. I’ve been on warfarin for 12 years. I check my INR like clockwork. But I never thought about how a cold could mess with it. This post made me realize I need to talk to my pharmacist, not just my doctor.
People think medicine is just pills and fixes. But it’s really about timing, balance, and listening. I’m grateful for the Liverpool tool. I saved a screenshot.
Thanks for not just scaring people. You gave us a way forward.
🙏
The entire discourse surrounding anticoagulant interactions with antiviral therapies remains fundamentally flawed by its reliance on reactive rather than predictive frameworks. The notion that one can simply ‘pause’ a DOAC and resume it two days post-Paxlovid is not a protocol-it is a gamble dressed in clinical language. There is no universal pharmacodynamic profile among patients; renal clearance varies, body mass index modulates volume of distribution, and genetic polymorphisms in CYP3A4 and P-gp are not accounted for in any algorithm currently in use. The Liverpool tool, while commendable in its ambition, is a bandage on a hemorrhage. We require real-time, point-of-care anti-Xa monitoring integrated into EHRs-not a static checklist that assumes homogeneity in a heterogeneous population. And yet, we continue to treat patients as data points. This is not medicine. This is triage by spreadsheet.
And let us not forget: the 37% increase in ER visits? That’s not an epidemic of drug interaction. That’s an epidemic of fragmented care.
Until we restructure how we coordinate between primary care, pharmacy, and emergency services, we are merely rearranging deck chairs on the Titanic.
I’m a nurse in rural Kansas. We don’t have a clinical pharmacist on staff. Last month, an 82-year-old man came in with a GI bleed after taking Paxlovid and rivaroxaban. He didn’t know they interacted. His daughter didn’t know. His primary care doc didn’t know. We had to call a specialist in Wichita at 3 a.m.
This isn’t just about guidelines. It’s about access. People in small towns don’t have time to read 12-page PDFs. They need someone to tell them, face to face: ‘Stop this pill for five days.’
Can we make a simple one-pager? A printable flyer? Something that says: ‘If you’re on a blood thinner and get COVID-call your pharmacist before taking ANY new pill.’
We need this in every pharmacy, every clinic, every doctor’s waiting room. Not just in big cities.
It is imperative that the patient population be made aware of the inherent risks associated with concomitant administration of direct oral anticoagulants and antiviral therapeutics. The current paradigm of patient self-management, while laudable in principle, is demonstrably inadequate in the context of polypharmacy and age-related pharmacokinetic alterations. The responsibility for ensuring safe medication use cannot be delegated to the layperson without robust, standardized, and universally accessible education. Furthermore, the absence of mandatory pharmacogenomic screening prior to initiation of DOAC therapy represents a systemic failure of clinical governance. I urge all healthcare institutions to implement mandatory pre-prescription counseling protocols, supported by AI-driven drug interaction alerts embedded directly into e-prescribing platforms. Until such measures are codified into law, patient safety remains an afterthought.
my grandma took paxlovid and didn’t tell anyone she was on rivaroxaban. she’s fine. maybe it’s not as bad as they say?
also i think the liver is kinda overrated.
Oh great. Another article written by someone who thinks their job is more important than your life. You want us to stop our blood thinners because a pill might make us bleed? What about the stroke we’ll get because we listened to you? You’re not a doctor. You’re a glorified pharmacy brochure.
And why are we even using Paxlovid? It’s just a placebo with side effects. The real cure? Fresh air and vitamin D. But hey, let’s keep selling pills and panic.
Next you’ll tell us to stop breathing because it might trigger a clot.
Thanks for the fear porn.
This is the kind of post that reminds me why I still believe in community. I’ve been on dabigatran for 6 years, and I’ve never once felt like I understood the full picture-until now. Thank you for breaking it down without jargon. I printed this out and gave it to my sister, who’s on apixaban and just tested positive. She cried. Not from fear-from relief.
We need more of this. Not just facts. But care. Care that says: ‘You’re not alone in this.’
And yes, I used the Liverpool tool. I’m pausing my pill. And I’m texting my pharmacist right now.
You’ve done something rare here. You’ve made people feel safe enough to listen.
Thank you.