When a brand-name drug goes generic, patients often face a confusing choice: stick with the expensive brand, switch to a cheaper generic, or try something in between-authorized generic. Many don’t even know this third option exists. But for patients on critical medications-like blood thinners, seizure drugs, or thyroid hormones-this choice isn’t just about cost. It’s about safety, consistency, and trust.
What Exactly Is an Authorized Generic?
An authorized generic is not a copy. It’s the exact same pill, capsule, or injection as the brand-name drug, made by the same company, in the same factory, with the same active and inactive ingredients. The only difference? It doesn’t carry the brand name on the label. You might see a different color, shape, or marking, but the medicine inside is identical. The FDA defines it clearly: authorized generics are marketed under the original brand’s New Drug Application (NDA). That means they skip the usual generic approval process. They don’t need to prove bioequivalence because they’re already proven-they’re the same product. This isn’t a loophole. It’s a legal pathway created by the Hatch-Waxman Act in 1984 to encourage competition without sacrificing quality. Unlike regular generics, which must meet FDA standards for equivalence but can differ in fillers, dyes, or binders, authorized generics have zero variation in formulation. For patients with allergies to lactose, gluten, or artificial dyes, this matters. A 2023 GoodRx study found that 12.7% of patients had adverse reactions switching to regular generics due to inactive ingredients. With authorized generics? That number drops to 2.3%.Why Switch at All?
Cost is the biggest driver. Authorized generics often cost 4-8% less at the retail level than the brand-name drug-and up to 14% cheaper for wholesalers. In some cases, they’re priced lower than regular generics because the brand company is using them to compete with other generics entering the market. But price isn’t the only reason. For drugs with a narrow therapeutic index-where even tiny differences in absorption can lead to overdose or treatment failure-authorized generics offer unmatched stability. The FDA estimates about 5.3% of all prescriptions fall into this category. These include warfarin, levothyroxine, lithium, and phenytoin. For patients on these drugs, switching to a regular generic can trigger lab abnormalities, hospital visits, or worse. A 2021 study in the Journal of Clinical Pharmacy and Therapeutics showed that 18.4% of patients switched back to the brand after trying a regular generic. Only 7.2% did the same after switching to an authorized generic. That’s a 60% drop in switchbacks. For chronic conditions like asthma, the Asthma and Allergy Foundation of America found a 42% lower discontinuation rate with authorized generics.Why Don’t More People Use Them?
The biggest problem? Most patients-and even many doctors-don’t know they exist. A 2022 National Consumers League survey found that 41% of patients had never heard of authorized generics. Pharmacists often don’t mention them unless asked. Insurance systems rarely distinguish them from regular generics in their databases. And when they do, they sometimes charge more. Here’s the catch: even though authorized generics are cheaper, some insurance plans put them on a higher tier than regular generics. A 2022 Health Affairs report found that 28% of commercial plans treat authorized generics as specialty-tier drugs, meaning higher copays. One patient on Reddit shared: “My insurance covered the brand but not the authorized generic version, costing me $45 more monthly despite identical medication.” Another barrier is availability. As of Q3 2023, only 37.5% of brand-name drugs with generic alternatives had an authorized generic version. If your drug isn’t one of them, you can’t switch. The FDA’s Orange Book lists which drugs have authorized generics, but it’s not user-friendly. That’s why the FDA launched the Authorized Generic Finder tool in 2023-finally making it easier to check.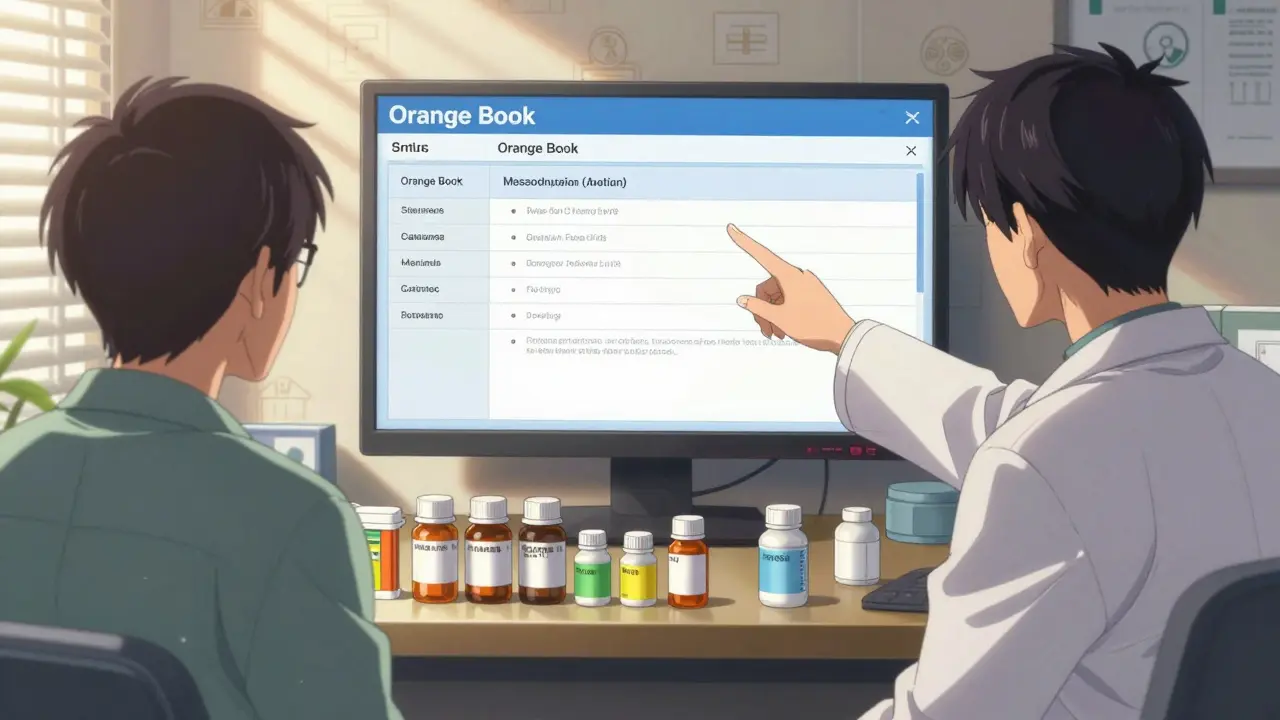
How to Manage the Transition
Switching to an authorized generic shouldn’t be a surprise. It needs planning. Here’s how to do it right:- Check availability. Use the FDA’s Authorized Generic Finder or ask your pharmacist to look up the drug in the Orange Book. If an authorized generic exists, it’ll be listed alongside the brand name.
- Verify insurance coverage. Call your insurer. Ask: “Is the authorized generic covered at the same tier as the regular generic?” Don’t assume. Some plans charge more for the authorized version.
- Educate the patient. Use simple language: “This is the exact same medicine you’ve been taking, just without the brand name on the bottle.” Show them the FDA-approved fact sheet. Visual aids help-compare the old and new pill side by side.
- Coordinate between prescriber and pharmacist. The prescriber should write “dispense as written” or “no substitution” if the patient prefers the authorized generic. Pharmacists should flag it in the system to avoid accidental substitution later.
- Follow up. For high-risk drugs, check in at 14 and 30 days. Ask: “Has your condition changed? Any new side effects?” Most patients won’t volunteer concerns unless asked.
What the Experts Say
Dr. Jane Axelrad, FDA Associate Director for Generic Drugs, says: “Authorized generics offer the therapeutic consistency of brand-name products with generic pricing.” The American Pharmacists Association recommends them specifically for narrow therapeutic index drugs, citing a 34% reduction in adverse events. But not everyone sees them as a win. Dr. Aaron Kesselheim of Harvard warns that labeling authorized generics as “superior” might make patients distrust regular generics-even though both are FDA-approved and safe. That’s a real risk. The FDA’s job isn’t to pick favorites. It’s to ensure all approved drugs work as intended. The FTC’s long-term analysis adds another layer: while authorized generics drive down prices, they might discourage other generic manufacturers from challenging patents. If fewer companies enter the market, long-term competition could suffer. That’s why the FTC still supports them-because the immediate savings outweigh the risk.