COVID-19 and Blood Thinners: What You Need to Know About Risk, Medication, and Safety
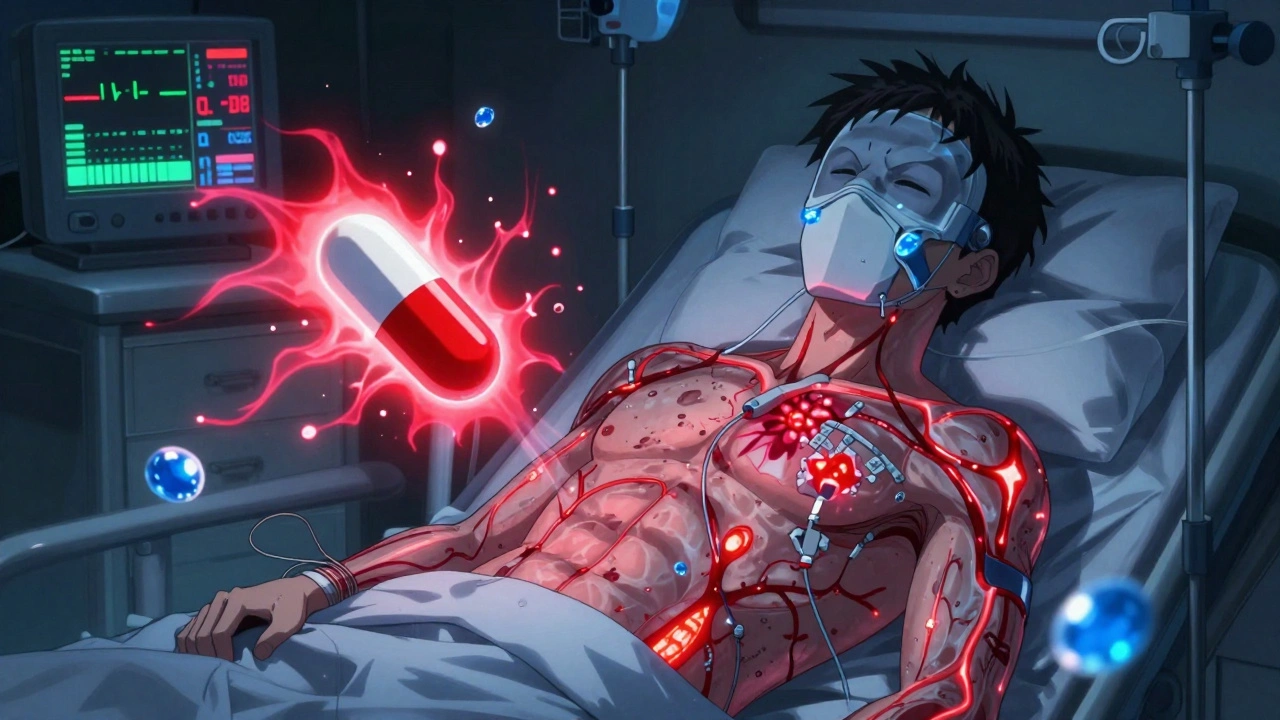
When you have COVID-19, a viral infection that can trigger dangerous blood clots. Also known as SARS-CoV-2 infection, it doesn’t just affect your lungs—it can turn your blood into a sticky, clot-prone mess. That’s why doctors often turn to blood thinners, medications that stop clots from forming or growing. Also known as anticoagulants, these drugs are lifesavers for some patients but can be risky if used incorrectly. Not everyone with COVID-19 needs them, but for those with severe illness, hospitalization, or a history of clotting problems, they’re a standard part of care.
Why does this happen? The virus triggers inflammation that makes your blood vessels sticky and your platelets overactive. In severe cases, clots can form in your lungs, heart, brain, or legs—leading to strokes, heart attacks, or pulmonary embolisms. Studies show that hospitalized COVID-19 patients have a much higher chance of clots than people with other types of pneumonia. That’s why hospitals started giving low-dose blood thinners to most admitted patients, even if they didn’t have a clot yet. It’s not about treating clots—it’s about stopping them before they start.
Not all blood thinners are the same. Heparin, a fast-acting injectable anticoagulant. Also known as low molecular weight heparin, it’s commonly used in hospitals because it works quickly and can be monitored easily. For people recovering at home, warfarin, a long-term oral anticoagulant. Also known as Coumadin, it’s older but still used when clots are a recurring threat. Newer options like rivaroxaban, a direct oral anticoagulant. Also known as Xarelto, it’s easier to take and doesn’t need regular blood tests. But they’re not for everyone. If you’re at low risk, taking blood thinners can cause bleeding problems without any benefit. If you’re at high risk, skipping them could be deadly.
What should you do if you’re on a blood thinner and get COVID-19? Don’t stop or change your dose without talking to your doctor. Some medications interact badly with COVID-19 treatments. Others might need dose adjustments if you’re sick, dehydrated, or not eating well. If you notice unusual bruising, swelling in one leg, chest pain, or trouble breathing, get help right away. These aren’t normal side effects—they could be signs of a clot or a bleed.
The good news? Most people who get mild COVID-19 don’t need blood thinners. The key is knowing your risk. If you’re older, have heart disease, diabetes, or a history of clots, talk to your doctor before you get sick. Ask: "If I end up in the hospital, will I get a blood thinner?" That conversation could save your life.
Below, you’ll find real-world advice from patients and clinicians on how to manage blood thinners safely during and after COVID-19—from spotting warning signs to avoiding dangerous drug combos and knowing when to push back on treatment.
Respiratory Infections and COVID-19: How Anticoagulants Interact with COVID Treatments and What It Means for Your Safety
COVID-19 and its treatments like Paxlovid can dangerously alter how blood thinners work, increasing risks of bleeding or clots. Learn how to safely manage anticoagulants during respiratory infections with up-to-date guidelines and real-world strategies.