Joint Injection: What It Is, How It Works, and What You Need to Know
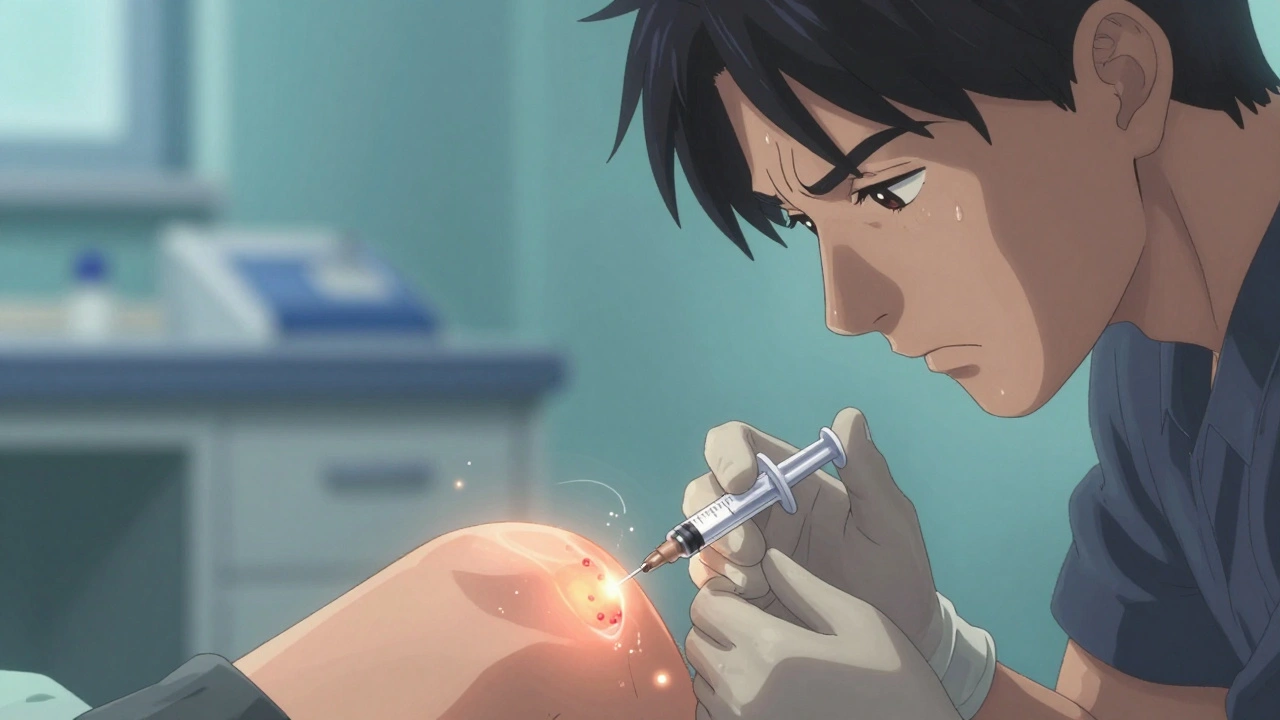
When your knees, shoulders, or hips ache from wear and tear, a joint injection, a procedure where medication is delivered directly into a painful joint to reduce inflammation and pain. Also known as intra-articular injection, it’s one of the most common ways doctors help people avoid surgery or reduce reliance on oral painkillers. It’s not a cure, but for many, it’s a game-changer—letting them walk without limping, sleep through the night, or play with their grandkids again.
Most joint injections use corticosteroid, a powerful anti-inflammatory drug that mimics the body’s natural cortisol mixed with a local anesthetic for immediate relief. The effect can last weeks to months, depending on the joint and the person. For some, it’s a one-time fix. For others with chronic conditions like osteoarthritis or rheumatoid arthritis, it becomes part of a regular management plan. But it’s not the only option. synovial fluid, the natural lubricant inside joints that thins out with age and disease can be replaced with hyaluronic acid injections, especially in knees. This doesn’t reduce inflammation like steroids, but it helps the joint move smoother—like adding oil to a rusty hinge.
Who gets these injections? Mostly adults over 50 with joint degeneration, but also younger people with sports injuries, bursitis, or gout. The procedure takes under 15 minutes and is done in a clinic, not a hospital. You’ll feel a pinch, then pressure, then usually relief within a day or two. But it’s not risk-free. Repeated injections can weaken tendons or cartilage over time. That’s why most doctors limit them to three or four a year per joint. And if you’re diabetic, steroids can spike your blood sugar—so monitoring is key.
What you won’t find in most doctor’s offices are the real stories: the woman who skipped knee replacement because one injection gave her six months of hiking; the man who tried pills for years and found his pain vanished after a shoulder shot; the athlete who used injections to stay competitive while rehabbing. These aren’t outliers—they’re common outcomes when the right person gets the right injection at the right time.
There’s also a lot of confusion around safety. Some think it’s just a placebo. Others worry about side effects from steroids. But the data is clear: when used properly, joint injections are safe and effective. They’re backed by decades of clinical use and are recommended by guidelines from the American College of Rheumatology and the FDA. Still, they’re not for everyone. If you have an infection near the joint, uncontrolled diabetes, or are on blood thinners, your doctor will weigh the risks.
Below, you’ll find real posts from people who’ve been there—whether they’re asking how to prepare, what to expect after, or how to tell if it’s working. You’ll also find advice on when to avoid injections, what alternatives exist, and how to talk to your doctor about whether this is right for you. No fluff. Just facts, experiences, and practical steps to help you decide what comes next.
Corticosteroid Injections for Joint Pain: What They Do, How They Work, and When to Avoid Them
Corticosteroid injections offer fast relief for joint inflammation but aren't a long-term fix. Learn how they work, who benefits most, the real risks of repeated use, and when to choose other treatments.