Short-Term Steroids: What They Do, Risks, and Real-World Uses
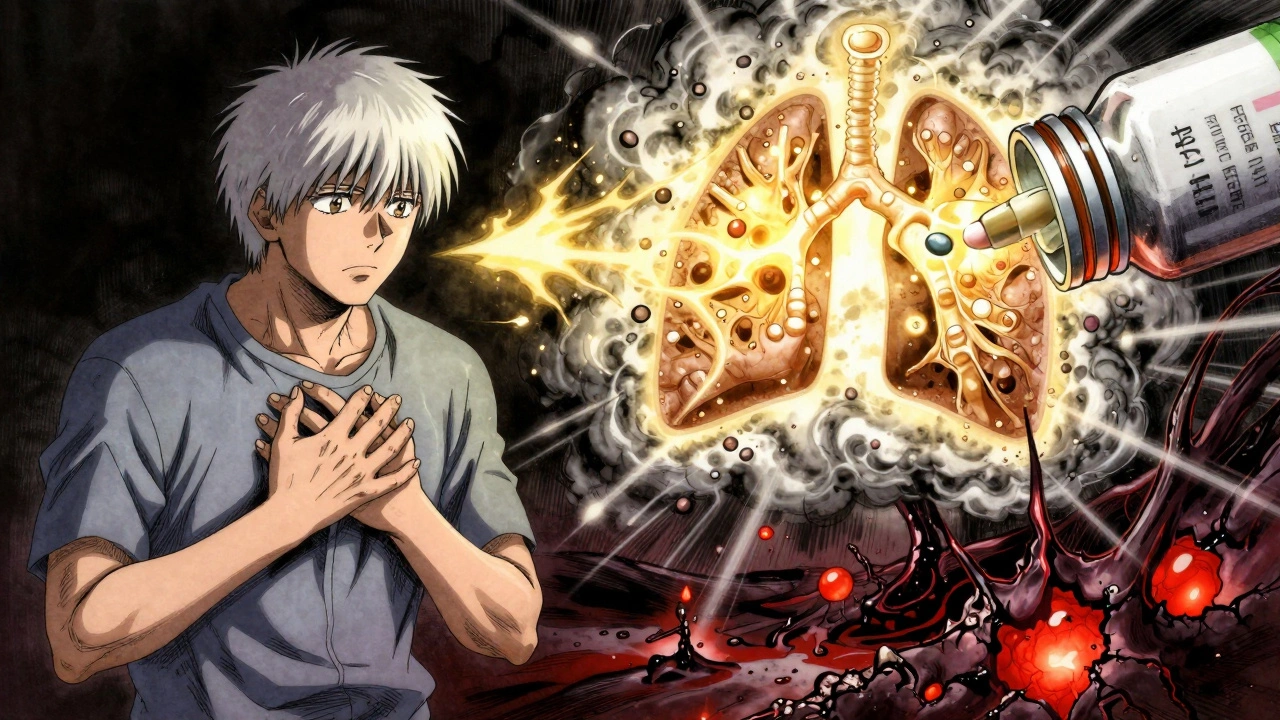
When doctors prescribe short-term steroids, a class of anti-inflammatory drugs used for brief periods to manage acute conditions. Also known as corticosteroids, they’re not the same as the anabolic steroids misused in sports. These medications mimic cortisol, your body’s natural stress hormone, and can turn down inflammation fast—often within hours. Many people use them for flare-ups of arthritis, asthma attacks, allergic reactions, or severe skin conditions. They’re not meant for daily, long-term use, but even a few days or weeks can make a big difference when used right.
Corticosteroids, the medical term for the type of steroids used to reduce inflammation, come in many forms: pills, injections, creams, and inhalers. For joint pain, a single corticosteroid injection, a targeted shot delivered directly into an inflamed joint can give weeks of relief without affecting the whole body. But even localized shots carry risks if used too often—tissue weakening, infection, or spikes in blood sugar. And while short-term oral steroids like prednisone are common, they can still cause trouble: trouble sleeping, mood swings, increased appetite, or a sudden rise in blood pressure. These side effects aren’t guaranteed, but they’re real enough that you need to know what you’re signing up for.
What makes short-term steroids tricky is that they don’t treat the root cause. They silence the symptom—like turning off an alarm without fixing the fire. That’s why they’re powerful tools in the right hands, but dangerous if used carelessly. People with diabetes, high blood pressure, or a history of mental health issues need extra caution. Even healthy adults can develop temporary issues like fluid retention or blurred vision. The key is timing: a 5- to 10-day course is very different from taking the same dose for months. And you never just stop them cold—your body needs time to restart its own cortisol production.
The posts below cover real situations where short-term steroids are used—and where they shouldn’t be. You’ll find clear guidance on when injections help with joint pain, how they interact with other drugs like blood thinners, and what signs mean it’s time to call your doctor. There’s also info on how these drugs affect pregnancy, how they’re monitored in clinical settings, and why some people avoid them entirely after seeing side effects. This isn’t about fear. It’s about knowing when to say yes, when to say no, and how to use them safely when they’re truly needed.
Corticosteroids: When Short-Term Relief Outweighs Long-Term Risks
Corticosteroids offer fast relief for inflammation but carry serious long-term risks like bone loss, diabetes, and infections. Learn when they’re necessary, how to minimize harm, and what safer alternatives exist.