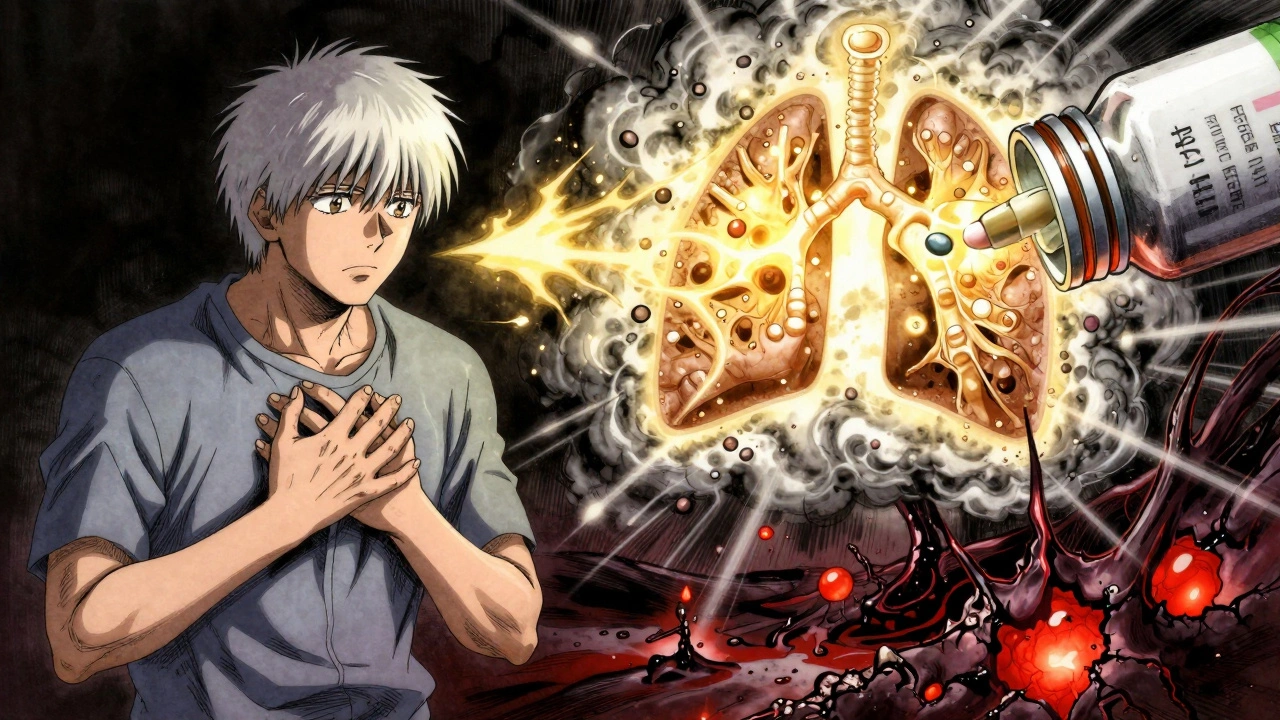
When you're in pain - joints swollen, lungs tight, skin burning - corticosteroids can feel like a miracle. Within days, sometimes hours, the inflammation drops, the fever breaks, the breathing clears. But that relief doesn't come without a price. And the longer you take them, the heavier that price becomes.
How Corticosteroids Work - Fast and Hard
Corticosteroids, like prednisone and hydrocortisone, are synthetic versions of cortisol, the hormone your body naturally makes to handle stress and inflammation. They don't cure anything. Instead, they silence your immune system's alarm bells. For conditions like rheumatoid arthritis, lupus, severe asthma, or a sudden flare of eczema, that silence is lifesaving. Unlike other anti-inflammatory drugs that take weeks to kick in, corticosteroids act fast. A single oral dose of prednisone can reduce joint swelling by 70% in under 48 hours. Injections into a painful knee or shoulder often bring relief within a week, with effects lasting weeks to months. That speed is why doctors reach for them during emergencies - like a severe asthma attack or a flare-up of inflammatory bowel disease. But here’s the catch: your body wasn’t designed to run on this kind of chemical firehose. Corticosteroids don’t just turn off inflammation - they mess with nearly every system in your body. Blood sugar spikes. Bone density crumbles. Immunity weakens. Mood swings hit. And the longer you stay on them, the more damage stacks up.The Real Side Effects - Not Just Weight Gain
Most people know about moon face and weight gain. But those are just the visible signs. The hidden dangers are worse. After just 5 to 30 days of use, even short courses of corticosteroids raise your risk of serious problems:- Sepsis: Risk jumps by 430%. Your body can’t fight off infections like it used to.
- Blood clots: Venous thromboembolism risk rises by 230%. A clot in your leg can travel to your lungs.
- Bone fractures: Your bones lose density fast - up to 3-5% per month in the first year. A simple fall can break a hip.
- High blood sugar: Even people without diabetes can develop steroid-induced diabetes. Blood sugar levels can spike so high they need insulin.
- Cataracts and glaucoma: Eye pressure builds. Vision blurs. Some damage is permanent.
When Are They Actually Needed?
Corticosteroids aren’t meant for every ache or sniffle. Yet, they’re overused - badly. In the U.S., 21% of adults got at least one prescription for systemic corticosteroids between 2012 and 2015. Nearly half of those were for conditions where they offer little to no benefit: common colds, sinus infections, back pain, and bronchitis. Doctors know this. The American College of Rheumatology and the European League Against Rheumatism both say: don’t use steroids for viral infections. But pressure from patients who want quick relief, combined with time constraints in clinics, leads to overprescribing. The real, evidence-based uses are clear:- Acute flare-ups of rheumatoid arthritis, lupus, or vasculitis
- Severe asthma or COPD exacerbations
- Relapsing multiple sclerosis
- Severe allergic reactions or anaphylaxis
- Organ transplant rejection
How Long Is Too Long?
There’s no safe long-term dose. But guidelines give us boundaries. The American College of Rheumatology says: no more than 12 weeks of systemic steroids for inflammatory arthritis - and even then, at the lowest possible dose. For most, that’s 5 to 10 mg of prednisone daily. Anything beyond that needs specialist review. The European League Against Rheumatism is even stricter: no patient with rheumatoid arthritis should stay on more than 5 mg of prednisone daily beyond six months - unless all other treatments have failed. And here’s something most patients don’t know: even after you stop, your body doesn’t bounce back right away. Corticosteroids suppress your adrenal glands. They stop making cortisol. If you stop suddenly, your body can go into adrenal crisis - low blood pressure, vomiting, collapse. That’s why tapering isn’t optional. It’s life-saving.How to Protect Yourself If You Must Take Them
If your doctor says you need steroids, ask these questions:- What’s the exact dose and duration? (No more than 14 days unless absolutely necessary.)
- Will I need a taper? (If yes, make sure you get the schedule in writing.)
- What monitoring will happen? (Blood sugar, bone scans, eye exams.)
- Are there alternatives? (DMARDs, biologics, NSAIDs - even physical therapy?)
- A baseline DEXA scan to check bone density
- Monthly blood sugar tests
- Quarterly eye checkups
- Calcium (1,200 mg/day) and vitamin D (800 IU/day) supplements
- Annual bone-strengthening shots like zoledronic acid

New Hope - Safer Alternatives Are Coming
The good news? Science is catching up. In December 2023, the FDA approved fosdagrocorat, the first selective glucocorticoid receptor modulator (SGRM). Unlike traditional steroids, it reduces inflammation without triggering as many side effects. In trials, it cut hyperglycemia risk by 63% compared to prednisone at the same dose. Hospitals are also changing. Since January 2024, Medicare Advantage plans require pre-authorization for any steroid course longer than 10 days. Electronic health records now flag inappropriate prescriptions - and in hospitals using these alerts, inappropriate prescribing dropped by 31%. But these tools are only as good as the people using them. Until every doctor treats steroids like a controlled substance - with strict limits and full monitoring - patients still bear the risk.The Bottom Line
Corticosteroids are not evil. They’re powerful. And like a chainsaw, they’re brilliant for cutting through an emergency - but terrible for everyday trimming. If you’ve taken them for a flare-up and felt better, that’s real. But if you’re still on them months later, you’re not being treated - you’re being managed with a blunt instrument. Talk to your doctor. Ask if you can switch to a DMARD or biologic. Ask if your dose can drop. Ask if you’ve had your bone scan this year. And if you’re being prescribed steroids for a cold or back pain - say no. There’s a better way. The goal isn’t to avoid steroids forever. It’s to use them wisely - briefly, at the lowest dose, with full protection - and never let them become your default solution.Can corticosteroids cause permanent damage?
Yes. Long-term use - especially beyond 3 months - can lead to permanent changes. These include cataracts (12% of long-term users), osteoporosis (8%), and steroid-induced diabetes (7%), even after stopping. Bone loss begins within weeks and doesn’t always reverse. Eye damage and muscle weakness can also become permanent if not caught early.
Is it safe to stop prednisone cold turkey?
No. Stopping suddenly can trigger adrenal insufficiency - a life-threatening condition where your body can’t produce enough cortisol. Symptoms include extreme fatigue, dizziness, nausea, and low blood pressure. Always taper under medical supervision. For courses longer than 14 days, a minimum 7-day taper is required. In some cases, especially after long-term use, tapering can take weeks or months.
Why do doctors prescribe steroids for colds if they don’t work?
They shouldn’t. Viral infections like colds, bronchitis, and sinusitis don’t respond to steroids. But patient pressure, time constraints, and the desire to “do something” lead to overprescribing. Studies show 47% of steroid prescriptions in the U.S. are for conditions with no proven benefit. This is a known quality-of-care failure. If you’re given steroids for a cold, ask for evidence - and consider getting a second opinion.
How do I know if I’m on too high a dose?
If you’re taking more than 7.5 mg of prednisone daily for over 3 months, you’re in the high-risk zone. Signs you’re on too much include rapid weight gain, facial puffiness, easy bruising, mood swings, or blood sugar spikes. Your doctor should be monitoring your bone density, eye health, and glucose levels. If they’re not, ask why. The goal is always the lowest effective dose for the shortest time.
Are steroid injections safer than pills?
Injections are safer for localized issues - like a swollen knee or shoulder - because they deliver the drug directly to the problem area, reducing overall exposure. But they’re not risk-free. Repeated injections can damage nearby tissue, weaken tendons, and raise blood sugar. Systemic absorption still happens. For chronic conditions, injections shouldn’t be used more than 3-4 times per year in the same joint. They’re a tool for flare-ups, not maintenance.
What are the best alternatives to corticosteroids?
For autoimmune and inflammatory conditions, disease-modifying drugs (DMARDs) like methotrexate or biologics like adalimumab are safer long-term options. They take weeks to work but don’t cause bone loss, diabetes, or immune suppression. For pain and inflammation, NSAIDs (like ibuprofen) or physical therapy can help - though they’re less potent than steroids. Newer drugs like fosdagrocorat, approved in late 2023, offer steroid-like benefits with fewer side effects and may replace traditional steroids in the coming years.
Write a comment
Your email address will not be published.






14 Comments
So I got prescribed prednisone for a bad flare last year. Thought I was getting magic fairy dust. Turns out I got moon face, insomnia, and a diabetes diagnosis. My doctor said it was "just for a couple weeks." Two months later I was on insulin. Don't let them trick you into thinking it's harmless.
Also, why do we still treat steroids like they're Advil? This post is a wake-up call.
Respectfully it is imperative to acknowledge that corticosteroids remain indispensable in acute inflammatory emergencies despite their significant adverse effects. The medical community must prioritize patient education and strict adherence to evidence based guidelines to mitigate long term harm. Prevention through early intervention with DMARDs is the optimal strategy.
It's interesting how the article frames corticosteroids as a chainsaw when in reality they're more like a sledgehammer - blunt force trauma with immediate results. The real issue isn't the drug itself but the systemic failure of primary care to have the time or resources to implement alternatives. I've seen patients prescribed steroids for bronchitis because the doctor had 7 minutes to see them and the patient was demanding something. The system is broken not the medication.
And yet the data on sepsis and thrombosis risk is terrifying. Even a 10-day course increases VTE risk by over 200%. That's not a side effect - that's a public health crisis disguised as a quick fix.
Why aren't we mandating electronic alerts for every steroid prescription? Why aren't we requiring mandatory counseling on tapering? Why are we still letting GPs prescribe these like they're cough syrup?
The FDA's approval of fosdagrocorat is promising but it's not a panacea. It's still early stage. And the real problem is inertia. Doctors are trained to prescribe steroids because they work. The alternatives require follow-up, monitoring, referrals - things our current healthcare model disincentivizes.
Also, the fact that only 42% of doctors do basic monitoring like bone scans or eye exams is criminal. This isn't negligence - it's negligence on a national scale.
And yet I still get why patients beg for it. When you can't breathe or walk, you don't care about osteoporosis in 5 years. You care about breathing right now.
It's a tragic trade-off. We need better tools. We need more time. We need to stop treating inflammation like a bug to be sprayed away.
bro i was on 20mg of prednisone for 6 weeks for my eczema and i swear i gained 18lbs and started having panic attacks. my doc just said "it'll go away" but it didn't. i still have trouble sleeping and my bones feel weak. why do they not tell you this stuff before you start?
also i got a steroid shot in my knee last year and now my tendon feels like it's gonna snap. so much for "localized".
Y'all need to stop treating steroids like they're a quick fix and start treating them like they're a nuclear reactor. One wrong move and everything goes sideways.
My mom was on them for RA for 18 months. She’s fine now, but she’s got cataracts, osteoporosis, and a permanent sweet tooth from all the sugar spikes. She’s on 5 supplements just to keep her from crumbling.
But here’s the thing - she’s alive. She can walk. She can hug her grandkids. And if we’d said no to steroids when she was in agony, she’d be in a wheelchair today.
It’s not about avoiding them. It’s about using them like a scalpel, not a hammer. And if your doctor isn’t monitoring you like you’re a ticking bomb - find a new one.
Wow. Another anti-medical establishment diatribe. You know what’s worse than steroids? The fact that people think they know better than doctors because they read a blog post.
My uncle had lupus. He didn’t die because of steroids. He died because he stopped taking them after reading Reddit. Don’t be that guy.
One must contemplate the ontological paradox of medical intervention: the very mechanism that preserves life also accelerates its decay. Corticosteroids are the Sisyphus of pharmacology - pushing the boulder uphill only to watch it roll back down as the body crumbles.
Yet, we cling to them because we fear the silence of suffering more than the noise of decay.
Is this not the human condition? We trade eternity for a moment of ease.
Also 🤷♂️
I’m crying. I’m crying because I was one of those people who got prescribed prednisone for a "bad allergy" and ended up in the ER with blood sugar so high they thought I was diabetic.
I’m crying because I’m 28 and I already have osteoporosis.
I’m crying because my doctor didn’t warn me.
I’m crying because I had to tell my mom I might never have kids because of the damage.
But I’m also crying because this post got it right. We need to stop normalizing this. This isn’t medicine. This is damage control with a side of denial.
As a rheumatology nurse with over a decade of experience, I can confirm: this is the most accurate summary of steroid use I’ve ever seen in a public forum.
Patients are terrified of biologics because of the cost and injections. So they take prednisone - because it’s cheap, fast, and their doctor says "it’s just for a little while."
Then they come back six months later with a broken hip and a new diabetes diagnosis.
We need to stop letting primary care be the gatekeeper for steroids. This should be a specialist-only decision - period.
And yes, fosdagrocorat is coming. But we can’t wait for it. We need to change the culture now.
My sister’s doctor gave her steroids for a sinus infection. She got a blood clot. Now she’s on blood thinners for life. The doctor didn’t even mention the risk. She’s 32. She has a toddler. This isn’t just negligence - it’s a crime.
USA bad. Canada gives you a 3-day course and a pamphlet. Here? You get a 30-day script and a shrug.
Also 🤡
my doc gave me 5mg for 2 weeks. i took it for 8 months. i didn’t think it mattered. i was wrong.
now i’m on calcium, vitamin d, and a bone shot every year. and i still get dizzy if i stand up too fast.
don’t be me.
So let me get this straight - you’re blaming doctors for prescribing the only thing that works? How about blaming the patients who demand quick fixes? How about blaming the insurance companies that won’t cover biologics? How about blaming the pharmaceutical companies that market steroids like candy?
Everyone’s a victim except the people who actually make the decisions.
Also, your "evidence" is a 2023 survey? That’s not science. That’s a blog post with stats.
OMG I JUST GOT PRESCRIBED PREDNISONE FOR A COLD 😭😭😭 I’M SO SCARED I’M GONNA TURN INTO A MOON PERSON AND DIE FROM A BLOOD CLOT 😭😭😭
PLS HELP I DON’T WANT TO BECOME A STATISTIC 😭😭😭
…
jk i’m fine. i’m not even taking it. but this post made me feel things.