Sleeve Gastrectomy: What It Is, Who It Helps, and What You Need to Know
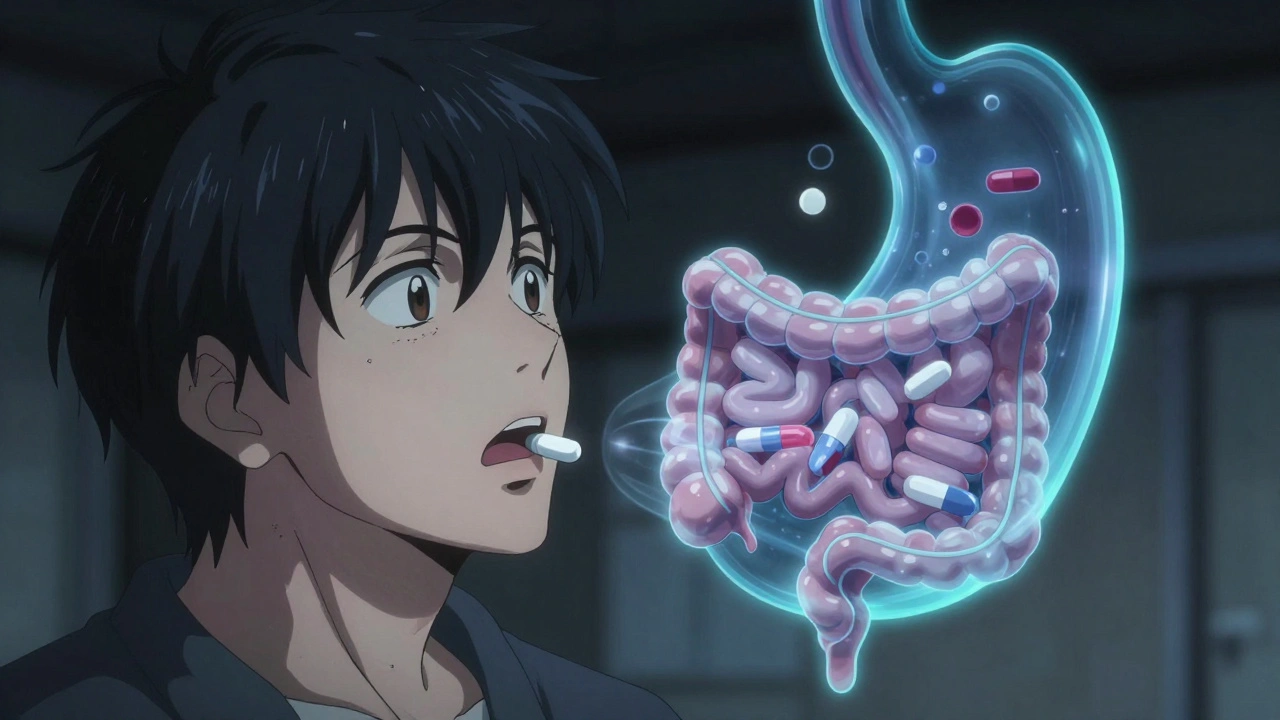
When you hear sleeve gastrectomy, a surgical procedure that removes about 80% of the stomach to help with long-term weight loss. Also known as gastric sleeve, it's one of the most common bariatric surgery options today—especially for people with obesity-related health issues like type 2 diabetes, high blood pressure, or sleep apnea. Unlike older procedures that reroute the intestines, this one is simpler: it doesn’t touch your digestive tract, just makes your stomach smaller. That means fewer complications, faster recovery, and less risk of nutrient malabsorption.
But it’s not just about shrinking your stomach. The surgery also cuts out the part of the stomach that makes ghrelin—the hormone that tells you you’re hungry. That’s why many people notice a real drop in appetite after surgery. It’s not willpower. It’s biology. And that’s why it works better for so many than dieting alone. Still, it’s not a magic fix. Success depends on changing how you eat, moving more, and sticking with follow-up care. People who skip doctor visits or go back to old habits often regain weight. This isn’t a quick fix—it’s a lifelong shift.
Who qualifies? Usually, adults with a BMI over 40, or over 35 with serious health problems tied to weight. Some insurance plans require proof you’ve tried other methods first. And while it’s generally safe, it’s still surgery. Risks include leaks, infections, blood clots, and vitamin deficiencies. That’s why post-op care matters so much. You’ll need regular blood tests, supplements like B12 and iron, and often help from dietitians or counselors.
You’ll also find that obesity treatment doesn’t stop at the operating table. Many people combine surgery with medication, therapy, or lifestyle coaching. And while some of the posts below talk about medications like canagliflozin or corticosteroid injections, they’re not replacements for this kind of surgery—they’re part of the bigger picture. If you’re managing diabetes, joint pain, or anxiety after weight loss surgery, you’re not alone. The right support system makes all the difference.
What you’ll find here isn’t a list of success stories. It’s real talk: how to avoid dangerous drug combos after surgery, how to track your health through blood tests, how to handle medication changes when your body’s healing, and how to spot fake advice online. Some posts cover pregnancy and medications, others talk about polypharmacy risks or how to talk to your doctor without feeling judged. All of it ties back to one thing: staying safe and healthy after sleeve gastrectomy isn’t just about what you eat—it’s about how you manage your whole health.
Bariatric Surgery and Medication Absorption: How Dose and Formulation Changes Save Lives
Bariatric surgery changes how your body absorbs medications. Learn which drugs are affected, why, and how to adjust doses safely after gastric bypass or sleeve gastrectomy.