Steroid Injections: What They Are, How They Work, and When to Use Them
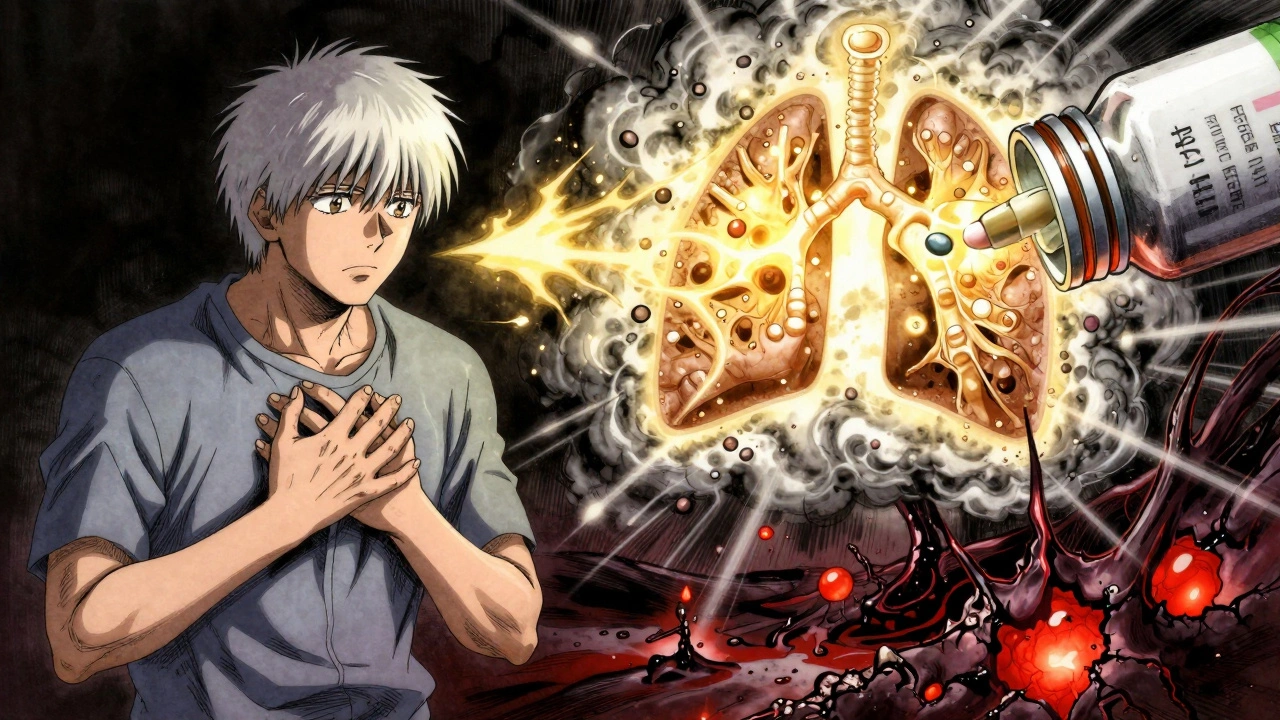
When you hear steroid injections, a medical treatment that delivers synthetic hormones to reduce inflammation in joints, tendons, or soft tissues. Also known as corticosteroid injections, they’re one of the most common ways doctors quickly calm down severe pain from arthritis, bursitis, or tendonitis. These aren’t the same as the muscle-building steroids athletes misuse. These are anti-inflammatory drugs—like prednisone or methylprednisolone—that mimic your body’s natural cortisol to shut down swelling and pain at the source.
They work by stopping immune cells from releasing chemicals that cause swelling, heat, and pain. That’s why you often feel relief within a few days, sometimes even hours. But they’re not a cure. They’re a pause button. A cortisone shot, a common type of steroid injection used for joint and soft tissue inflammation might let you walk without pain for months, but if the root problem—like worn-out cartilage or overused tendons—is still there, the pain comes back. That’s why doctors limit how often you can get them. Too many injections can weaken tendons, damage cartilage, or raise blood sugar, especially if you have diabetes.
Not everyone is a good candidate. If you’re pregnant, have an active infection, or have had a recent joint replacement, steroid injections might not be safe. And if you’ve already tried physical therapy, weight loss, or over-the-counter pain relievers without success, that’s often when your doctor suggests one. They’re most effective in larger joints like knees, shoulders, and hips, or in areas like the spine for nerve-related pain. But they’re rarely used in small joints like fingers unless the inflammation is extreme.
There’s also a big difference between a single injection and repeated ones. One shot might give you months of relief. Three or four in a year? That’s where risks start piling up. Some studies show cartilage breakdown speeds up after multiple injections in the same joint. That’s why smart doctors pair them with lifestyle changes—like movement, weight control, or braces—not as a replacement, but as a bridge.
What you won’t find in this collection are flashy claims about steroid injections being miracle cures. You’ll find real talk: how they actually work, who they help most, the quiet dangers of overuse, and what alternatives exist when the shot stops working. You’ll see how they fit into bigger health pictures—like managing arthritis without relying on pills, or why some people avoid them entirely because of diabetes or infection risk. These posts don’t sell you hope. They give you facts, so you can decide if a steroid injection is the right tool for your pain—or if there’s a better path ahead.
Corticosteroids: When Short-Term Relief Outweighs Long-Term Risks
Corticosteroids offer fast relief for inflammation but carry serious long-term risks like bone loss, diabetes, and infections. Learn when they’re necessary, how to minimize harm, and what safer alternatives exist.