Warfarin and COVID meds: What you need to know about interactions and risks
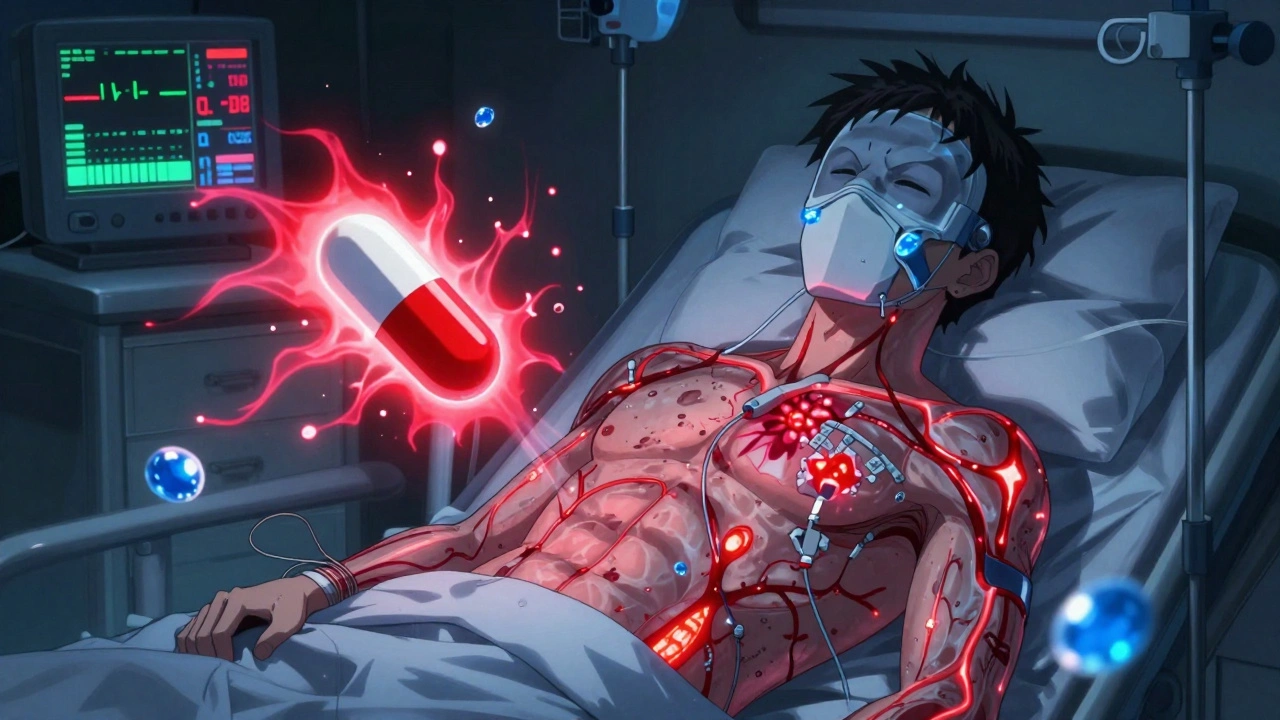
When you're taking warfarin, a blood thinner used to prevent clots in people with atrial fibrillation, deep vein thrombosis, or artificial heart valves. Also known as Coumadin, it's one of the most common medications that can go wrong when mixed with other drugs. During the pandemic, many people started taking new treatments for COVID-19, a viral infection that can cause severe respiratory illness and trigger inflammation throughout the body—like antivirals, steroids, or even over-the-counter pain relievers. But here’s the problem: some of those drugs can make warfarin too strong—or too weak—and either raise your risk of bleeding or let dangerous clots form.
For example, corticosteroids, like prednisone, often used to reduce lung inflammation in severe COVID cases can increase your INR, meaning your blood takes longer to clot. That’s not always bad if you’re being monitored—but if your doctor doesn’t know you’re on warfarin, a simple steroid course could land you in the ER. Then there’s antiviral drugs, such as Paxlovid (nirmatrelvir/ritonavir), which are designed to block viral replication. Ritonavir, one of its components, is a strong inhibitor of liver enzymes that break down warfarin. That means warfarin builds up in your system, and even a normal dose can become toxic. One study showed INR levels jumped by over 50% in patients taking both within days.
It’s not just prescription drugs. Even something as simple as ibuprofen, a common painkiller many take for fever or body aches with COVID, can irritate your stomach lining and raise bleeding risk when combined with warfarin. And don’t forget St. John’s Wort, a herbal supplement some use for low mood—it’s been linked to treatment failure in HIV meds, but it also speeds up warfarin breakdown, making it useless. These aren’t hypothetical risks. Real people have had strokes, internal bleeds, and hospitalizations because these interactions weren’t caught in time.
What should you do? First, never start or stop any new medication—prescription, OTC, or supplement—without telling your pharmacist or doctor you’re on warfarin. Second, keep your INR checked regularly, especially when you’re sick or starting a new treatment. Third, use a medication tracker. Write down everything you take, including doses and times. When you go to the ER or see a new provider, bring that list. Most people don’t realize how many drugs can interfere with warfarin. Even antibiotics like ciprofloxacin or metronidazole can change how your body handles it.
The good news? These risks are well-documented and avoidable. You don’t have to choose between treating your COVID symptoms and staying safe on warfarin. But you do need to be proactive. The posts below give you real, practical advice on spotting dangerous drug combos, understanding how your body processes medications, and talking to your care team so you’re never caught off guard. Whether you’re managing warfarin long-term or just started it during a recent illness, this collection will help you make smarter, safer choices.
Respiratory Infections and COVID-19: How Anticoagulants Interact with COVID Treatments and What It Means for Your Safety
COVID-19 and its treatments like Paxlovid can dangerously alter how blood thinners work, increasing risks of bleeding or clots. Learn how to safely manage anticoagulants during respiratory infections with up-to-date guidelines and real-world strategies.