
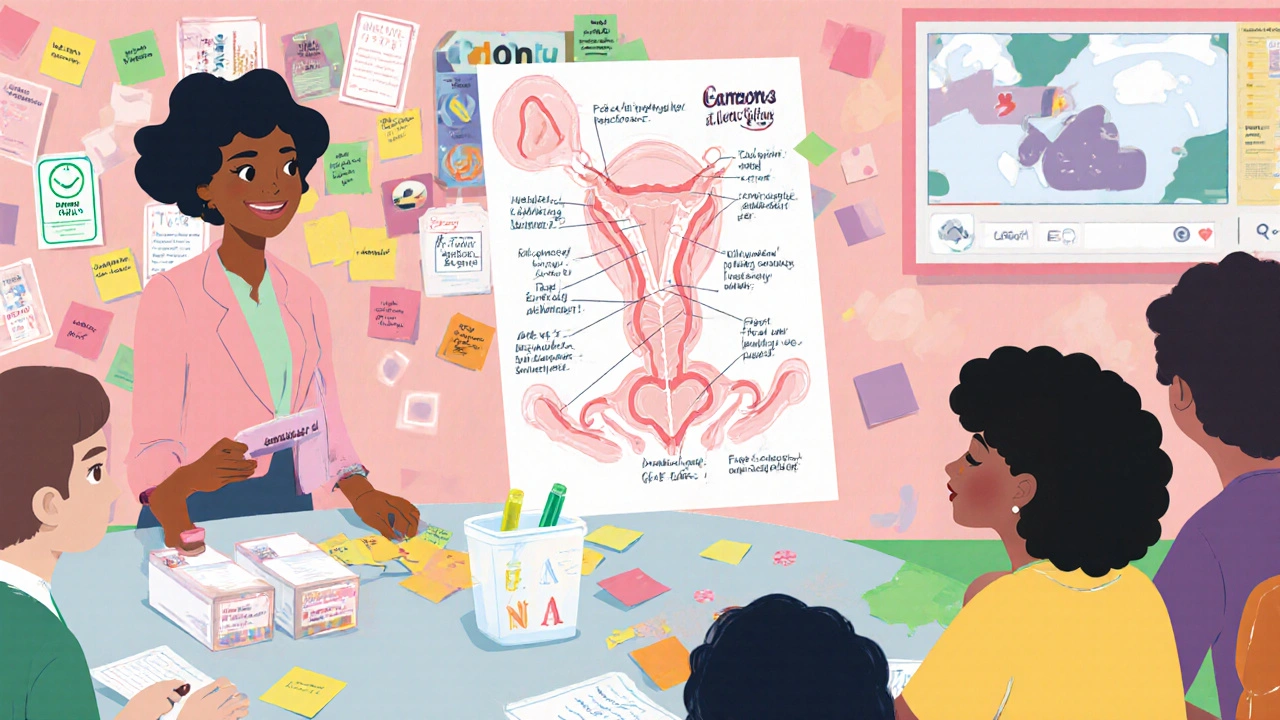
Gonorrhea Facts Quiz
Quick Facts About Gonorrhea
Test your knowledge with these essential facts about gonorrhea. Select the correct answer for each question.
Submit your answers to see the correct responses and key facts.
Key Takeaways
- Know the three most important facts about gonorrhea that every teen should hear.
- Use a 5‑step lesson framework that fits into any school period.
- Combine factual info with interactive activities to boost recall.
- Address stigma head‑on with language that normalizes testing and treatment.
- Leverage free resources from CDC, WHO and local health departments for up‑to‑date data.
What Is Gonorrhea?
When building a sex‑education unit, Gonorrhea is a bacterial sexually transmitted infection (STI) caused by Neisseria gonorrhoeae. It spreads through vaginal, anal or oral contact and can affect anyone who is sexually active. In the United States, the CDC recorded over 600,000 cases in 2023, a 30% rise from five years earlier, signalling that the infection is far from a relic of the past. Untreated, it can lead to pelvic inflammatory disease, infertility, and increased HIV transmission risk.
Why Focus on Teens?
Adolescents (ages 13‑19) are at a unique crossroads. Hormonal changes, peer pressure and the rise of dating apps create a perfect storm for STI exposure. According to WHO, 1 in 4 sexually active teens will contract an STI before age 25. Their bodies are still developing, making them more vulnerable to complications. Moreover, many teens lack accurate information, rely on myths, or feel too embarrassed to ask questions.
Core Components of an Effective Lesson
A well‑structured session should cover five pillars: knowledge, risk perception, skills, attitudes, and resources. Below is a step‑by‑step outline that can be squeezed into a typical 45‑minute class.
- Hook (5min) - Show a short, age‑appropriate video clip that illustrates a real‑life scenario where a teen discovers they have an STI.
- Fact Flash (10min) - Deliver three non‑negotiable facts about gonorrhea: transmission routes, asymptomatic nature, and treatability with antibiotics.
- Myth‑Busting (5min) - Use a quick poll (hand‑raise or digital) to identify common misconceptions, then correct them.
- Skill Practice (15min) - Role‑play condom negotiation and how to talk to a partner about testing.
- Resource Rundown (5min) - Hand out a one‑page flyer that lists local clinics, free testing sites, and hotlines.
- Reflection (5min) - Prompt students to write anonymously what they learned and any lingering worries.
Each segment uses active learning, which research from the American Journal of Public Health shows improves retention by up to 40% compared with lecture‑only formats.

Interactive Teaching Strategies
Interactive methods turn abstract statistics into personal relevance.
- Case‑Study Carousel - Stations with brief stories (e.g., “Jordan’s surprise diagnosis”). Students rotate, discuss, and suggest next steps.
- Anonymous Q&A Box - A sealed box where teens drop questions. The teacher addresses them later, preserving anonymity.
- Digital Quizzes - Platforms like Kahoot! let you ask true/false questions on gonorrhea transmission, instantly showing class performance.
- Peer‑Teaching Pods - Small groups prepare a 2‑minute pitch on a prevention method (e.g., condoms, testing) and present to peers.
These tactics align with the Sex education framework that encourages participatory learning, cultural sensitivity, and evidence‑based content.
Addressing Stigma Head‑On
Stigma is a silent barrier that keeps teens from seeking testing. Use neutral language: replace "dirty" or "promiscuous" with "sexually active". Highlight that infections are medical issues, not moral judgments. Share data: over 50% of teens with an STI were unaware until a routine screen caught it. Normalizing testing-just like getting a flu shot-helps break the taboo.
When discussing partner notification, frame it as caring: "Letting a partner know protects them, too." Role‑play this conversation so students see a respectful script in action.
Key Resources You Can Trust
Providing credible, up‑to‑date information builds trust. Below is a comparison of three major public‑health sources.
| Source | Update Frequency | Focus Areas | Free Materials |
|---|---|---|---|
| CDC | Quarterly | U.S. statistics, treatment guidelines, clinic locators | Lesson plans, infographics, video clips |
| WHO | Bi‑annual | Global trends, prevention strategies, policy briefs | Fact sheets, webinars, multilingual resources |
| Planned Parenthood | Monthly | Youth‑focused education, clinic finder, telehealth | Interactive modules, quizzes, printable guides |
All three offer printable flyers, slide decks and online videos that you can adapt to your class schedule.
Practical Tools for the Classroom
Here are tangible items you can bring:
- Condoms in various sizes, with clear instructions for correct use.
- Anonymous testing kits (often available through local health departments).
- Poster of the genital anatomy labeled with infection sites - a visual cue helps students locate symptoms.
- Sticky‑note board for the Q&A box.
When you hand out a condom, pair it with a brief demo on how to open and apply it. This demystifies the process and reduces fear.
Assessing Understanding and Follow‑Up
Start with a quick pre‑test (3‑question true/false) to gauge baseline knowledge. After the lesson, repeat the same questions; a gain of 2‑3 points signals effective learning.
Encourage students to schedule a free STI test within the next month. Provide a sign‑up sheet that can be turned over to a school nurse or community clinic-keeping names confidential.
If resources allow, schedule a follow‑up session two weeks later to discuss any test results (in general terms) and answer lingering concerns.
Frequently Asked Questions
How common is gonorrhea among teenagers?
In 2023, CDC data showed that about 15% of reported gonorrhea cases involved individuals aged 15‑24, making it one of the most frequently diagnosed STIs in that age group.
Can gonorrhea be cured with over‑the‑counter meds?
No. It requires prescription antibiotics, typically a single dose of ceftriaxone plus oral azithromycin. Over‑the‑counter products won’t clear the infection and may increase resistance.
What if a teen is scared to tell a partner about a positive test?
Teach a simple script: ‘I got tested and my results show I have an infection. It’s treatable, and I want us both to get checked so we stay healthy.’ Role‑playing this reduces anxiety.
Are there any signs that a teen might have gonorrhea without symptoms?
Yes. Up to 50% of infected females and 10% of infected males show no symptoms. That’s why routine screening is crucial, especially after a new sexual partner.
How can schools support confidential testing?
Partner with a local health department to host mobile testing clinics on campus or provide vouchers for nearby clinics. Ensure results are delivered directly to the student, not the school record.
Write a comment
Your email address will not be published.





13 Comments
While the curriculum appears comprehensive, one must acknowledge the inherent elitism of assuming all adolescents possess the requisite baseline knowledge to appreciate such nuance. The proposed five‑step framework, albeit methodical, risks alienating learners who lack prior exposure to epidemiological terminology. A more discerning approach would calibrate content to the diverse cognitive spectra within the classroom.
The lesson plan, as presented, suffers from an alarming paucity of pedagogical scaffolding that fails to address the multidimensional nature of adolescent sexual health education. By relegating the myth‑busting segment to a mere five minutes, the designers implicitly discount the deep‑seated misconceptions that proliferate within youth cultures. Moreover, the reliance on a single role‑play exercise neglects the necessity for iterative practice, which is essential for skill acquisition. The absence of longitudinal assessment mechanisms further compromises the sustainability of knowledge retention. Additionally, the resource list, though extensive, lacks contextual relevance to rural versus urban settings, thereby limiting its applicability. The integration of digital quizzes, while innovative, does not account for the digital divide that persists across socioeconomic strata. Consequently, the curriculum may inadvertently reinforce health disparities rather than ameliorate them. The choice of language throughout the materials oscillates between clinical jargon and colloquial phrasing, creating a tonal inconsistency that could confuse learners. The statistical claims regarding a 30 % rise in gonorrhea cases demand rigorous citation, yet the document provides no verifiable source. Furthermore, the recommended condom demonstration fails to incorporate alternative barrier methods, such as dental dams, which are pertinent for comprehensive education. The emphasis on anonymity, though commendable, is not operationalized with clear procedural guidelines for schools. Finally, the framework's duration of 45 minutes appears insufficient to cover the depth of content without sacrificing critical discussion time.
I appreciate the thoroughness of the proposed session and the clear emphasis on reducing stigma. The step‑by‑step outline is both practical and adaptable to various classroom environments. Including anonymous Q&A boxes demonstrates sensitivity to students' privacy concerns. The suggestion to partner with local health departments for confidential testing aligns well with best practices. Overall, the resource compilation offers valuable support for educators seeking evidence‑based materials.
Look, they’re feeding us stats that are straight out of the government’s agenda. Every time they push a new “lesson” they’re just reinforcing the narrative that they want us to believe. It’s no coincidence that the CDC’s numbers keep skyrocketing right when they roll out more testing kits. I’m skeptical about any program that claims to normalize testing without exposing the hidden motives behind it. If you ask me, we should question who’s really profiting from this “education”.
The analysis of the interactive components is thorough, yet it borders on invasive when it delves into students’ personal anxieties. While the case‑study carousel is engaging, it risks exposing vulnerable participants if not strictly anonymized. The critique of the resource list is valid, though a more systematic comparison would strengthen the argument. Overall, the feedback is constructive but could benefit from clearer boundaries regarding student privacy.
One must consider the possibility that the reported increase in gonorrhea cases is a manufactured statistic designed to justify expansive public health spending. The methodological rigor of the cited CDC data is, at best, questionable, given the opaque reporting mechanisms. It is plausible that the curriculum serves as a conduit for indoctrination under the guise of education. Therefore, we should approach such materials with a critical eye and demand transparent provenance of all referenced figures.
The inclusion of hands‑on condom demonstrations is a pragmatic step forward. Providing clear, concise instructions will likely improve student confidence in safe‑sex practices.
From a pseudo‑philosophical standpoint, the discourse on gonorrhea reflects a broader dialectic of risk and agency within modern adolescence. By framing the infection as a vector of both vulnerability and empowerment, educators can facilitate a ontological shift in how teens perceive sexual health. The integration of interactive modules serves as a phenomenological bridge between abstract epidemiology and lived experience. Moreover, employing jargon such as "pathogen‑host dynamics" contextualizes the discussion within a scientific paradigm while remaining accessible. This dialectic ultimately fosters a praxis where knowledge translates into proactive behavior.
It is commendable that the lesson plan emphasizes confidential testing and destigmatization. The structured reflection activity provides an avenue for students to process their emotions in a safe manner. However, the language occasionally slips into informal misspellings such as "teh" which may undermine the professional tone. Definately, a balance between approachability and academic rigor is essential. Overall, the framework aligns with contemporary best practices in sexual health education.
Ah, the cultural tapestry of sex ed-always a delightful blend of earnest intent and bureaucratic overreach. It’s almost artistic how the curriculum tries to be inclusive while forgetting the nuances of regional mores. One can’t help but marvel at the irony.
The alleged prevalence figures are evidently part of a coordinated effort to manipulate public perception. Accepting these statistics without scrutiny is a grave error. It is imperative that we demand verifiable data sources and question the underlying agenda driving these educational mandates.
Thank you for sharing such a comprehensive toolkit; it will be incredibly useful for teachers seeking to enhance their curricula. I especially appreciate the emphasis on empathy and the practical steps for role‑playing condom negotiation. The resource list is thorough and offers clear pathways for students to access testing services. If any educator needs further assistance in adapting these materials, I am happy to collaborate. Together we can ensure that adolescents receive accurate, supportive, and actionable sexual health education.
Great resources.