
More people in the UK and across the world are turning to CBD for sleep, pain, or anxiety-but many don’t realize how risky it can be when taken with their regular prescription meds. If you’re on blood thinners, heart medication, thyroid pills, or seizure drugs, mixing them with CBD isn’t just a bad idea-it could land you in the hospital.
Why CBD and Prescription Drugs Don’t Mix
CBD doesn’t just float through your body. It gets processed by the same liver enzymes that handle about 60% of all prescription medications. These enzymes, called CYP3A4 and CYP2C19, are like traffic controllers for drugs. They break down medications so your body can use them safely and get rid of the leftovers. But when CBD shows up, it jams the system. It blocks these enzymes, slowing down how fast your body clears other drugs. That means if you’re taking a medication that normally gets broken down quickly, CBD can cause it to build up in your blood. Too much of a good thing becomes dangerous. For example, warfarin-a common blood thinner-can become toxic if CBD slows its breakdown. That raises your risk of internal bleeding. One study found six out of seven people on warfarin who added CBD needed their dose lowered. Two had serious bleeding episodes.Medications That Could Turn Dangerous With CBD
Not all drugs react the same. Some are fine. Others? Not even close. The real danger comes with medications that have a narrow therapeutic index. That’s medical jargon for: the difference between the right dose and a toxic dose is tiny. A little extra in your bloodstream, and things go wrong fast. Here are the most common and risky ones:- Warfarin (blood thinner): CBD can spike levels, increasing bleeding risk.
- Amiodarone (heart rhythm): Can cause dangerous heart rhythm changes.
- Levothyroxine (thyroid): CBD may lower effectiveness, leaving you with fatigue, weight gain, or depression.
- Clobazam, Lamotrigine, Valproate (seizure meds): CBD can raise levels so high you get dizziness, confusion, or liver damage.
- Tacrolimus, Sirolimus (immunosuppressants): Used after organ transplants. CBD can cause toxic buildup, leading to kidney failure or infection.
The Grapefruit Test: A Simple Way to Spot Trouble
If your doctor or pharmacist told you to avoid grapefruit with your medication, that’s your first red flag. Why? Because grapefruit and CBD both block the same liver enzyme: CYP3A4. If your pill bottle says "avoid grapefruit," it’s basically saying: "Don’t mix this with CBD." About 85 prescription drugs carry this warning. That includes statins for cholesterol, certain blood pressure pills, anti-anxiety meds like triazolam, and even some cancer treatments. If your medication has that warning, skip CBD. No exceptions.What About Low Doses? Is a Little CBD Safe?
Some people say, "I only take 5mg of CBD oil. That’s tiny. It can’t hurt." But here’s the problem: it doesn’t matter how little you take. Even small doses of CBD can inhibit liver enzymes. That’s not a myth-it’s been proven in clinical trials. A 2023 review in Frontiers in Pharmacology showed that CBD’s effect on enzymes can last for days after you stop using it. So even if you take CBD in the morning and your pill at night, the enzyme blockage is still active. That’s why spacing doses doesn’t always help. There’s also no safe threshold. What’s low for one person could be high for another. Your age, weight, liver health, and other meds all change how your body reacts. There’s no official "safe" dose of CBD when you’re on prescription drugs.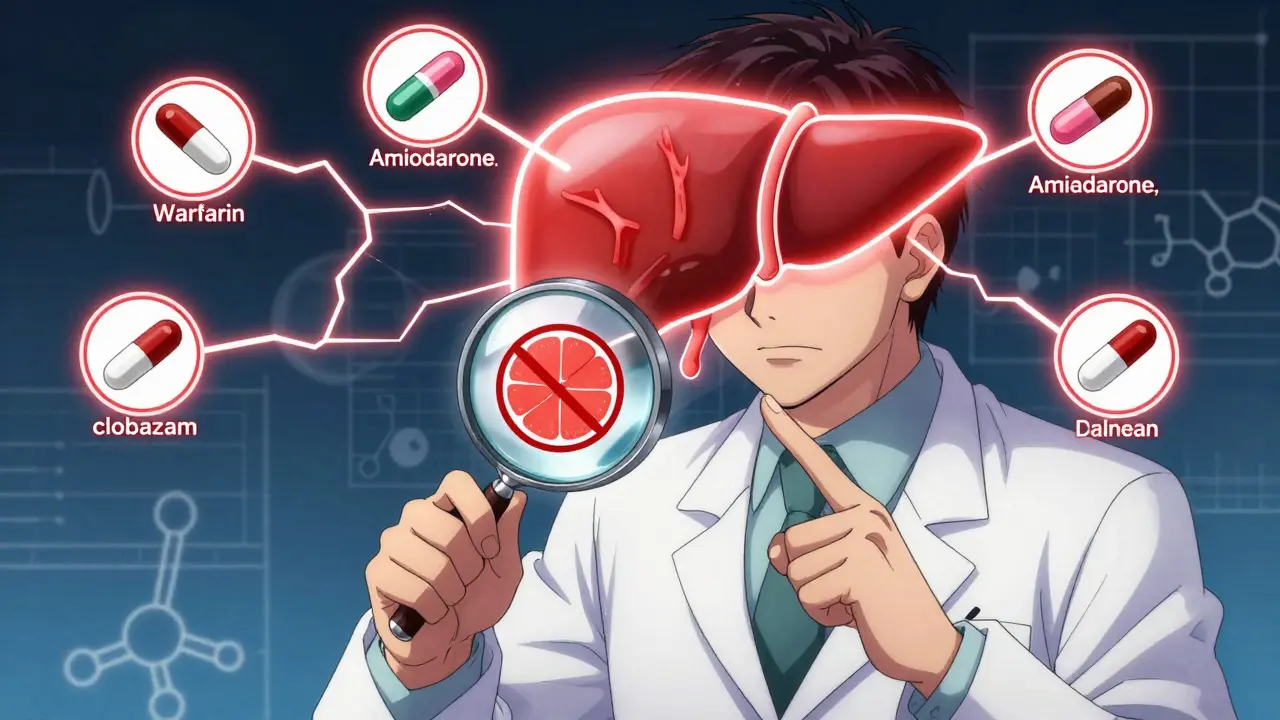
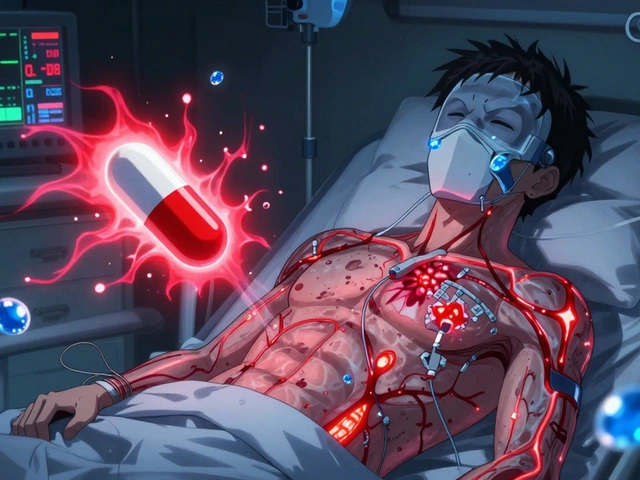
Liver Damage Is Real-And Often Silent
CBD isn’t harmless to your liver. In clinical trials of Epidiolex (the FDA-approved CBD drug for seizures), about 20% of patients had elevated liver enzymes-a sign of liver stress. That number jumped even higher in people taking other seizure meds at the same time. If your liver is already damaged from alcohol, fatty liver disease, or hepatitis, CBD can make things worse. The FDA says CBD is contraindicated in people with moderate to severe liver impairment. That means if you’ve been told your liver isn’t working right, you shouldn’t use CBD at all. And here’s the scary part: liver damage from CBD often has no symptoms until it’s advanced. No pain. No nausea. Just a blood test that shows your liver enzymes are climbing.Sedation Is a Hidden Risk
CBD makes you sleepy. That’s why people use it for insomnia. But if you’re already taking something that causes drowsiness-like Xanax, Benadryl, opioids, or alcohol-CBD can turn mild tiredness into dangerous sedation. One study found people who combined CBD with benzodiazepines had a 40% higher chance of falling, stumbling, or being involved in a car crash. That’s not just inconvenient. It’s life-threatening. If you’ve ever felt foggy after taking a painkiller or antihistamine, imagine that feeling doubled. That’s what happens when CBD teams up with CNS depressants.What Should You Do If You’re on Medication?
You don’t have to quit CBD cold turkey if you’re on meds. But you need a plan.- Make a full list of everything you take. That includes prescriptions, over-the-counter pills, herbal supplements, and even vitamins. Many people forget about melatonin or St. John’s Wort-they can interact too.
- Take it to your pharmacist. Pharmacists are trained to spot drug interactions. They have access to databases that check every combination. Ask them: "Can I take CBD with these?" Don’t rely on Google.
- Ask for blood tests. If you’re on warfarin, thyroid meds, or immunosuppressants, your doctor should check your blood levels before and after starting CBD. A simple test can catch trouble before it’s too late.
- Start ultra-low. If your doctor says it’s okay, begin with 2-5mg of CBD per day. Wait at least a week. Watch for dizziness, unusual bruising, or extreme fatigue.
- Stop immediately if something feels off. Unexplained bruising, confusion, nausea, or feeling "too sleepy" are warning signs. Don’t wait. Call your doctor.

What About CBD Products? Are They Reliable?
Not all CBD is created equal. A 2023 study found that nearly 1 in 3 CBD products sold online contained more CBD than labeled-or even traces of THC, which can also interact with meds. Some had no CBD at all. Look for products with a Certificate of Analysis (CoA) from a third-party lab. That’s a report showing exactly what’s in the bottle. Reputable brands now provide this on their website. If they don’t, walk away. Also, avoid gummies, vapes, and edibles if you’re on meds. They’re harder to dose accurately. Oils or capsules with clear milligram amounts are safer.When to Avoid CBD Completely
There are times when CBD isn’t worth the risk:- You take immunosuppressants (tacrolimus, sirolimus).
- You’re on blood thinners like warfarin or apixaban.
- You have liver disease or elevated liver enzymes.
- You’re taking seizure meds like valproate or clobazam.
- You’re scheduled for surgery-CBD can interfere with anesthesia.
The Bottom Line
CBD isn’t magic. It’s a powerful compound that interacts with your body in ways we’re still learning. For most people on prescription meds, the risks far outweigh the benefits. The FDA, Harvard Medical School, and leading pharmacists all agree: don’t mix CBD with your prescriptions unless you’re under direct medical supervision. If you’re thinking about trying CBD, talk to your doctor or pharmacist first. Bring your meds. Ask the hard questions. It’s not about being paranoid. It’s about being smart.Your health isn’t a gamble. Don’t risk it for a trend.
Can I take CBD with my blood pressure medication?
It depends. Some blood pressure meds, like amlodipine or lisinopril, aren’t strongly affected by CBD. But others-like verapamil or diltiazem-are processed by the same liver enzyme (CYP3A4) that CBD blocks. That can cause your blood pressure to drop too low, leading to dizziness or fainting. Always check with your pharmacist. If your med has a grapefruit warning, avoid CBD.
How long does CBD stay in my system if I’m on medication?
CBD’s half-life is 18 to 32 hours, meaning it takes about a day to half out of your system. But its effect on liver enzymes can last much longer-up to several days after your last dose. That’s why even spacing your CBD and meds apart won’t always prevent interactions. Chronic use makes this worse. If you’ve been taking CBD for weeks, your body is still affected even if you skip a day.
Is full-spectrum CBD riskier than isolate?
Yes. Full-spectrum CBD contains other cannabinoids like CBN and trace THC, which can also affect liver enzymes. Isolate is just CBD, so it’s slightly less complex. But even pure CBD isolate blocks CYP3A4 strongly enough to cause dangerous interactions. The difference isn’t enough to make full-spectrum safe. Stick to isolate only if you’re under medical supervision.
Can CBD replace my prescription medication?
No. CBD is not a substitute for prescribed drugs like warfarin, levothyroxine, or seizure medications. Stopping your prescription without medical guidance can be life-threatening. Some people use CBD alongside meds to reduce side effects-but only under a doctor’s watch. Never stop or change your meds based on CBD use.
What should I do if I accidentally took CBD with my medication?
Stop taking CBD immediately. Watch for signs like unusual bruising, extreme drowsiness, confusion, nausea, or irregular heartbeat. If you’re on warfarin or a heart medication, call your doctor or go to urgent care. A simple blood test can check if your drug levels are too high. Don’t wait for symptoms to get worse.
Write a comment
Your email address will not be published.



10 Comments
CBD’s inhibition of CYP3A4 and CYP2C19 is well-documented; however, the clinical significance of this interaction remains underappreciated by the general public. The pharmacokinetic data from Epidiolex trials, coupled with case reports involving warfarin and amiodarone, demonstrate a clear, dose-independent risk profile. The notion that ‘low doses are safe’ is not only misleading-it is dangerously inaccurate. Even sub-10mg daily doses have been shown to reduce enzyme activity by 30–50% in human hepatocyte models. This is not speculation-it is biochemistry.
Hey everyone-I get it, CBD helps with anxiety and sleep, and I’ve seen people thrive with it. But Laura’s right: this isn’t about fear-mongering, it’s about science. I’ve had clients on blood thinners who thought ‘natural’ meant ‘safe.’ Spoiler: it doesn’t. Talk to your pharmacist. Get bloodwork. Don’t guess. Your liver doesn’t care if it’s ‘just a little.’ It just knows: more toxin, more work. Be smart. You’ve got this.
It is empirically indefensible to assert that CBD is benign in polypharmacy contexts. The CYP450 enzyme system is not a suggestion-it is a biochemical gatekeeper. The cited studies (Frontiers in Pharmacology, 2023) are not outliers; they are consistent with the pharmacological canon. Furthermore, the assertion that ‘spacing doses mitigates risk’ is pharmacologically fallacious. Enzyme inhibition is non-linear and cumulative. To suggest otherwise is to misunderstand hepatic metabolism at a fundamental level. This is not opinion-it is pharmacokinetics.
People keep saying ‘talk to your doctor’ like they’re not already overwhelmed with 12 medications and a 10-minute appointment. Good luck explaining CBD to someone who’s never heard of CYP3A4. Meanwhile, the FDA approves a CBD drug for seizures but won’t regulate the $20 billion market. That’s not safety-that’s negligence.
I’ve been on levothyroxine for 8 years. Started CBD for sleep last winter. My TSH went from 2.1 to 5.8 in 6 weeks. I didn’t feel different-just tired. Got my levels checked because I read this article. Stopped CBD. Back to normal in 3 weeks. Just sharing. Don’t assume it’s fine.
It’s not just CBD-it’s the entire wellness-industrial complex that’s turned self-experimentation into a cult. People think because something is ‘plant-based’ or ‘organic’ it’s automatically benign. They ignore decades of pharmacology because a YouTube influencer said it ‘balances their chi.’ The fact that someone would casually mix CBD with tacrolimus after a kidney transplant isn’t ignorance-it’s arrogance. And now we have to clean up the mess. Your ‘natural remedy’ is someone else’s ER visit. Stop pretending you’re a pioneer. You’re just a walking hazard.
Why are we even having this conversation? CBD is a scam. It’s overpriced hemp water. If you’re on real medicine, you don’t need some hippie oil. The government should ban this junk. I don’t care if it’s ‘legal’-if it messes with my heart pills, it’s dangerous. And don’t give me that ‘third-party lab’ BS. Half those CoAs are fake. I’ve seen the receipts.
CBD is fine. You're overthinking. Just don't take it with warfarin. Everyone else is chill.
I’m a nurse in rural Ohio. I’ve seen patients on warfarin start CBD for pain after their knee surgery. They don’t tell their doctors. They think it’s ‘just herbal.’ One guy had a GI bleed. Another passed out driving. No one’s evil here-just uninformed. The answer isn’t to shame them. It’s to make clear, simple info available. Handouts at pharmacies. Signs on the CBD shelf. ‘If it says no grapefruit, skip this.’ That’s all it takes.
Oh, so now CBD is the new nicotine? Let me guess-next we’ll be banning kombucha because it ‘interferes with statins.’ You know what’s really dangerous? Not talking to your doctor. Not reading the label. Not checking interactions. But sure, let’s vilify a plant extract while Big Pharma keeps selling you pills that cost $500 a month and come with a 12-page warning leaflet. I’ll take my 5mg CBD oil over another SSRI any day. Just don’t tell me I’m a menace for choosing it.