When your liver starts to fail, it doesn’t just stop processing toxins-it starts pulling your whole body apart. One of the most dangerous, yet often missed, consequences is hepatorenal syndrome (HRS), a rapid and deadly form of kidney failure that happens not because the kidneys are damaged, but because the liver is dying. This isn’t a coincidence. It’s a cascade. And if you or someone you know has advanced cirrhosis, understanding HRS could mean the difference between life and death.
What Hepatorenal Syndrome Really Is
Hepatorenal syndrome isn’t kidney disease. It’s liver disease turning on the kidneys. In people with end-stage cirrhosis, blood flow gets messed up. The liver can’t handle pressure, so blood pools in the abdomen and gut. This triggers a chain reaction: the body thinks it’s losing blood, even though there’s too much fluid overall. In response, it tightens arteries everywhere-especially in the kidneys. Without enough blood flow, the kidneys shut down. No scarring. No infection. Just functional failure. This is why biopsies of kidneys in HRS patients look perfectly normal. The problem isn’t in the organ itself. It’s in the body’s desperate attempt to survive a failing liver. That’s why doctors call it a ‘functional’ kidney injury. It’s reversible-if you act fast.Two Types, Two Timelines
HRS isn’t one condition. It’s two. And they demand different responses. Type 1 HRS is a medical emergency. Creatinine levels spike-often doubling in under two weeks-rising above 2.5 mg/dL. Patients can go from stable to needing dialysis in days. Median survival without treatment? Just 2 weeks. This type usually shows up after a trigger: an infection like spontaneous bacterial peritonitis, heavy bleeding, or severe alcohol flare-ups. About 35% of Type 1 cases follow an infection. That’s why doctors check for it immediately when kidney function drops in someone with cirrhosis. Type 2 HRS creeps in slowly. Creatinine stays between 1.5 and 2.5 mg/dL. It’s tied to stubborn ascites-fluid in the belly that won’t go away, even with high doses of diuretics. This form doesn’t kill as fast, but it’s just as serious. It’s a sign the liver is nearing the end. Most people with Type 2 HRS end up on the transplant list.How Doctors Diagnose It (And Why So Many Get It Wrong)
There’s no single test for HRS. Diagnosis is a process of elimination. If your creatinine is up, doctors must rule out everything else first: dehydration, kidney stones, infection, drug damage, or blockages. They check your urine sodium-less than 10 mmol/L points to HRS. They look at urine osmolality-it’s higher than your blood. No blood in the urine. No protein. No signs of structural damage. Then comes the critical step: giving you albumin. One gram per kilogram of body weight, intravenously. If your kidneys don’t improve within 48 hours, and you’re not responding to stopping diuretics, HRS is likely. Missing this step leads to misdiagnosis in 25-30% of cases, according to experts at Hospital Clínic Barcelona. The problem? Most non-specialists don’t know this protocol. A 2021 study found only 58% of general physicians could correctly identify HRS from case scenarios. In community hospitals, protocols are rare. In academic centers, they’re standard. That gap kills people.
What Happens If You Don’t Treat It
Without treatment, Type 1 HRS is almost always fatal. Even with treatment, survival is grim. A 2020 UNOS analysis of nearly 5,000 patients showed that with just supportive care, only 18% were alive after one year. With vasoconstrictor therapy-like terlipressin plus albumin-that number jumps to 39%. But the only real cure? A liver transplant. Transplant patients with HRS have a 71% one-year survival rate. That’s higher than many other liver disease patients. Why? Because HRS is a clear signal: the liver is done. Transplant centers prioritize these patients. Since 2022, the MELD-Na score-used to rank transplant urgency-has been adjusted to give higher priority to those with HRS. That’s saved lives.The Treatment: Terlipressin and the Cost of Survival
The gold standard for Type 1 HRS is terlipressin, a drug that tightens blood vessels and restores flow to the kidneys. It’s given every 4 to 6 hours, along with daily albumin infusions. In the CONFIRM trial, 44% of patients saw their creatinine drop below 1.5 mg/dL within two weeks. But there’s a catch. Terlipressin isn’t FDA-approved in the U.S. until December 2022, when Mallinckrodt’s version, Terlivaz™, finally got the green light. It costs $1,100 per vial. A full 14-day course? Around $13,200. Many insurers still fight coverage. Patients report delays, denials, and having to switch to cheaper but less effective combos like midodrine and octreotide. Side effects are real. One Reddit user, ‘LiverWarrior42’, shared that terlipressin gave him severe abdominal pain-so bad they had to cut the dose in half. Others develop heart rhythm issues, low blood pressure, or even tissue death in fingers or toes from reduced blood flow. Still, for Type 1 HRS, the risk of not treating is far worse.What About Type 2? TIPS and Transplant Lists
For Type 2 HRS, the goal isn’t to reverse kidney failure-it’s to manage the ascites and get to transplant. Diuretics often don’t work. That’s where TIPS (transjugular intrahepatic portosystemic shunt) comes in. This procedure creates a new channel between liver veins to reduce pressure. Studies show it improves kidney function in 60-70% of Type 2 cases. But there’s a trade-off. About 30% of patients develop hepatic encephalopathy-brain fog, confusion, even coma-after TIPS. So it’s not for everyone. Many patients, like one Reddit poster whose husband’s HRS didn’t respond to meds, simply get listed for transplant. Their MELD-Na score climbs, pushing them higher on the list.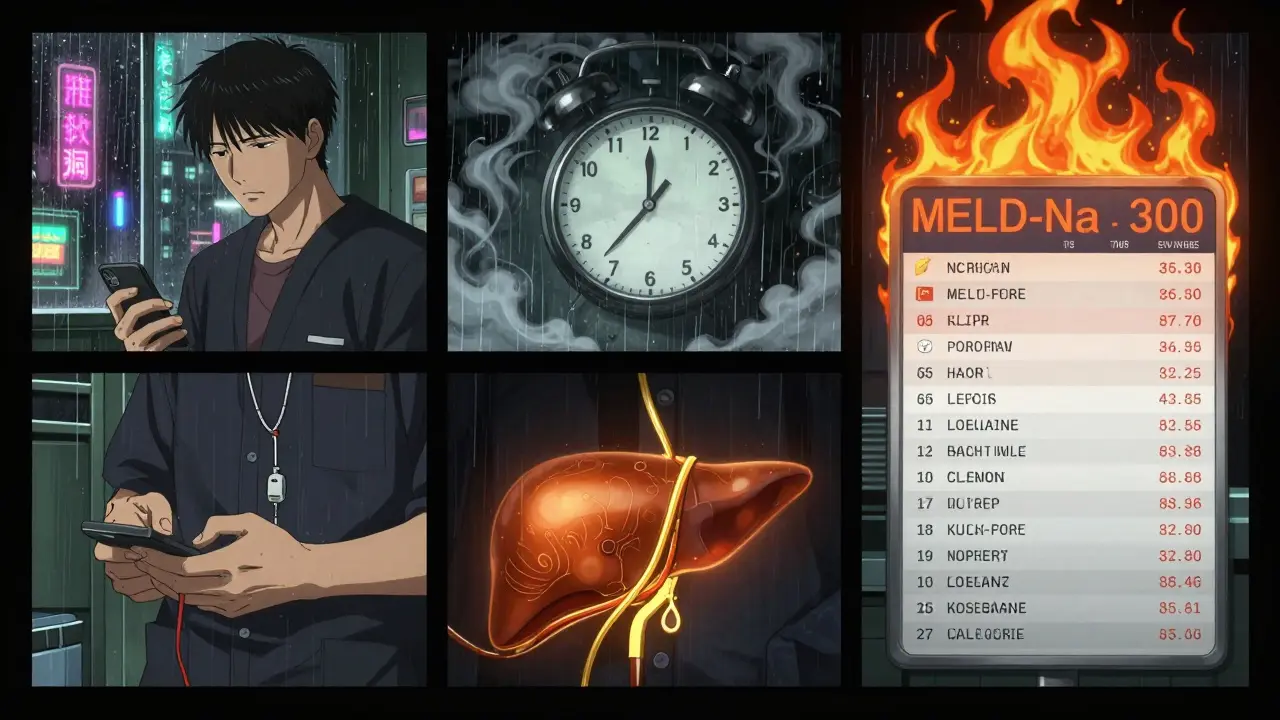
Why Early Detection Saves Lives
A 2022 Mayo Clinic study showed that when hospitals implemented a clear HRS protocol, diagnosis time dropped from over five days to less than two. Appropriate treatment use jumped from 54% to 89%. And 30-day survival improved by 22%. The takeaway? Speed matters. If you have cirrhosis and your creatinine rises-even slightly-push for a specialist. Ask about albumin challenge. Ask about urine sodium. Don’t wait for symptoms to get worse.The Future: New Drugs, Better Predictions
The future of HRS isn’t just about better drugs-it’s about catching it before it happens. Researchers are testing new biomarkers like NGAL (neutrophil gelatinase-associated lipocalin) in urine. Early data suggests levels above 0.8 ng/mL can predict HRS development in high-risk cirrhotics before creatinine even rises. Three new drugs are in Phase 3 trials: one uses a pump to drain ascites automatically, another targets ammonia buildup, and a third mimics the action of vasopressin. If any of these succeed, they could cut HRS deaths by 30-40% by 2027. But access remains unequal. In North America, 63% of HRS patients get vasoconstrictors. In sub-Saharan Africa, that number is 11%. Most get only fluids and diuretics. That’s not medical care. That’s waiting.What You Need to Do Now
If you have cirrhosis:- Know your creatinine. Ask for it at every visit.
- If it rises, demand a specialist consult-don’t wait for your primary doctor to refer you.
- Ask if you’ve been checked for spontaneous bacterial peritonitis.
- Ask about albumin infusion and terlipressin if you’re in Type 1 territory.
- Get on the transplant list early-even if you feel okay.
- Keep a log of urine output, weight, and creatinine.
- Know the signs of terlipressin side effects: chest pain, cold limbs, confusion.
- Advocate for insurance approval. Many denials are overturned on appeal.
Write a comment
Your email address will not be published.




11 Comments
this hit hard. my uncle just got diagnosed with type 2 hrs last month. they told him it's not the kidneys failing, it's the liver giving up. i didn't even know that was a thing. now i get why he's so tired all the time
i read this in the hospital waiting room while my mom was getting her albumin drip. they dont tell you how fast it can go south. one day shes fine next day creatinine up. scary stuff
so wait u mean all this expensive drug nonsense is just because doctors are too lazy to say liver = bad kidneys? lol. why not just transplant faster instead of wasting money on terlipressin? this whole system is broken
i mean... its poetic in a way. the liver, the body's detox queen, collapses and the kidneys just... surrender. no drama. no inflammation. just silent betrayal. we treat organs like machines but they're more like emotional partners. one breaks and the other just stops believing in love
terlipressin costs 13k?? 😳 i live in india and we dont even have that drug. we get furosemide and hope. i feel like if u dont have money u just wait to die. 🤷♂️
my cousin had this. they did the albumin test and it worked. she was scared but the doc was calm. we just kept track of her pee and weight. it helped. dont ignore the little things
this is why i became a nurse. i saw a patient go from 'i'm fine' to dialysis in 72 hours. no one saw it coming. education saves lives. share this. someone's mom, dad, sibling, friend needs to read this today
in nigeria we call this 'the silent killer that walks with a limp'. you see the swelling, the yellow eyes, the quietness... then one day they just stop answering calls. no scream. no warning. just gone. we need more awareness here. this post? it's a lifeline
i... i just cried reading this. my sister had type 1 hrs. we got lucky. terlipressin worked. but the cost... the insurance battles... the sleepless nights... i wish everyone knew how fragile this is. please, if you're reading this, check your numbers. please.
the real tragedy isn't the disease. it's that the system waits for someone to nearly die before it acts. why aren't we screening cirrhosis patients monthly for early biomarkers? why wait for creatinine to spike? we have the tools. we just don't prioritize life until it's almost gone
i'm the author. thank you all for sharing. this isn't just medical info. it's survival stories. keep talking. keep asking. keep pushing. we're not alone in this.