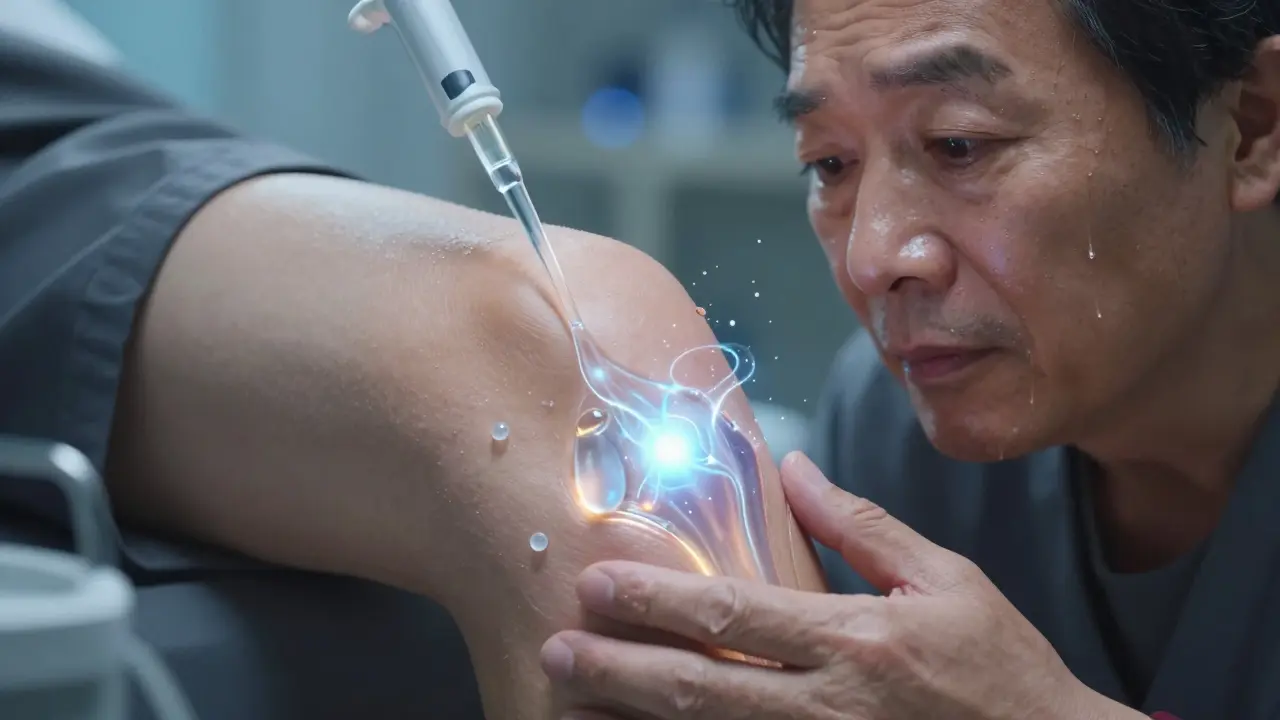
What Are Hyaluronic Acid Injections?
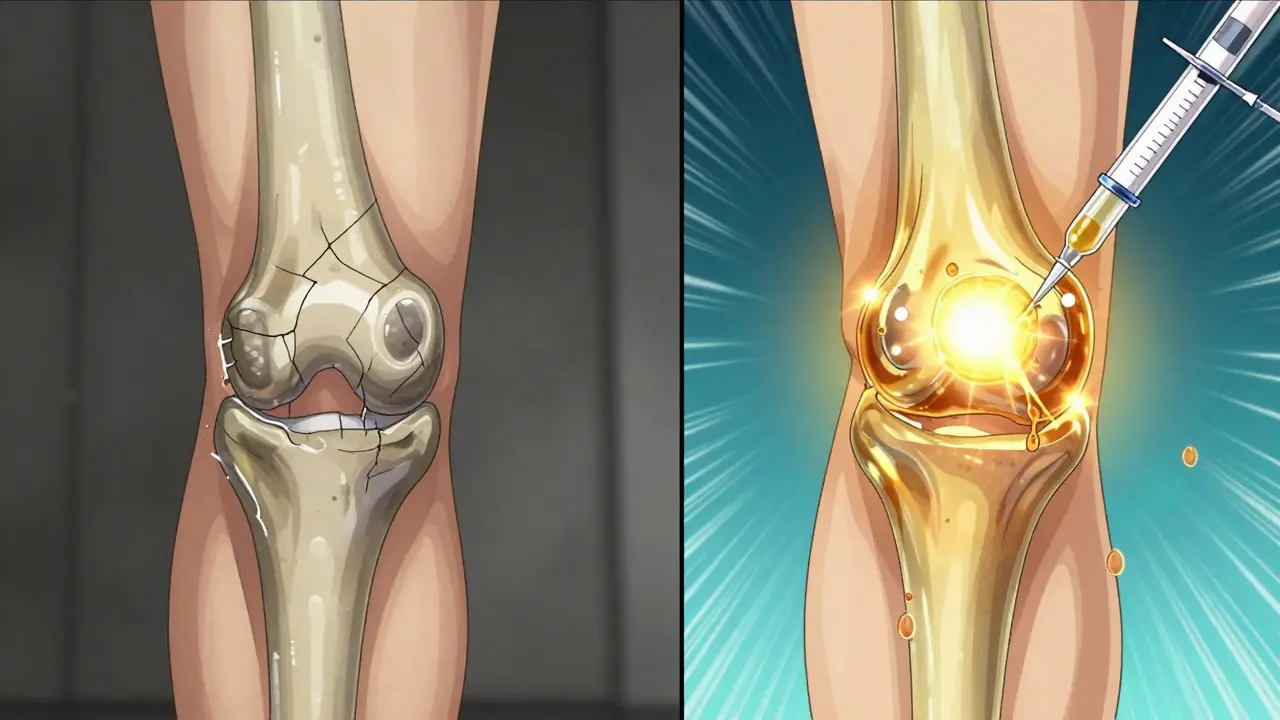
Hyaluronic acid injections, also called viscosupplementation, are shots given directly into the knee joint to help with osteoarthritis pain. They work by replacing the natural lubricant in your joint that breaks down over time. Healthy joints have a thick, slippery fluid called synovial fluid that cushions the bones and lets them glide smoothly. But in osteoarthritis, that fluid gets thin and watery - its hyaluronic acid levels drop by 30% to 50%. The injections aim to restore that thickness, reduce friction, and calm inflammation.
The first FDA-approved product, Hyalgan, came out in 1997 and was made from rooster combs - which is why some people still call these shots "rooster comb injections." Today, most are made using bacterial fermentation, not animal sources. Brands like Euflexxa, Synvisc, Gel-One, and Orthovisc all contain hyaluronic acid but differ in molecular weight, number of shots needed, and how long they last.
Who Gets These Injections?
You’re a likely candidate if you have mild to moderate knee osteoarthritis - usually Kellgren-Lawrence grades 1 to 3 - and other treatments haven’t helped enough. That means you’ve tried losing weight, doing physical therapy, using braces, or taking over-the-counter painkillers like ibuprofen, and your pain still limits your daily life.
These shots are not for everyone. If you have "bone-on-bone" arthritis (grade 4), studies show they won’t help. The same goes if you have an infection near the injection site, a bleeding disorder, or a known allergy to hyaluronic acid. Most patients are adults over 50, but age alone isn’t the deciding factor. It’s about how much joint damage is visible on X-rays and how much pain you’re really living with.
How Do the Injections Work?
The theory is simple: add back the missing lubricant, and the joint moves better. But it’s not just about slickness. Research suggests hyaluronic acid may also quiet down inflammation inside the joint. Some studies even hint it might protect cartilage from breaking down further - though there’s no solid proof it reverses damage.
The molecular weight of the product matters. Low-weight versions (like Hyalgan at 500 kDa) break down faster. High-weight ones (like Synvisc at 6,000 kDa) last longer. But here’s the twist: higher isn’t always better. One major 2004 study found that ultra-high molecular weight (100,000 kDa) didn’t outperform a placebo. Meanwhile, other research shows high-weight products give better pain relief for certain people. There’s no universal formula - what works for one person might do nothing for another.
How Many Shots Do You Need?
There are two main approaches: single-shot or multi-shot courses.
- Single-injection options like Gel-One are designed for convenience. You get one shot, and that’s it.
- Multi-shot regimens (three to five shots, spaced a week apart) are more common. Euflexxa and Orthovisc require three or four shots. Synvisc usually comes as three shots.
The Arthritis Foundation says three doses are more effective than one or two. But a 2022 meta-analysis found single injections didn’t offer meaningful pain relief compared to saline. Meanwhile, other studies found single and multiple shots worked just as well. So why the confusion? It might come down to individual biology. Some people respond quickly to one shot. Others need time for the fluid to build up in the joint.
The full effect usually takes 4 to 6 weeks to kick in. Pain relief peaks around 8 weeks and can last 6 months or longer - sometimes up to a year. That’s longer than steroid shots, which give fast relief but fade after 4 weeks.
How Do They Compare to Other Treatments?
| Treatment | Onset of Relief | Duration | Side Effects | Best For |
|---|---|---|---|---|
| Hyaluronic Acid Injections | 4-8 weeks | 6-12 months | Mild swelling, pain at injection site | Mild to moderate OA, patients avoiding steroids |
| Corticosteroid Injections | 1-3 days | 4-8 weeks | Temporary pain flare, cartilage thinning with repeated use | Acute flare-ups, short-term relief |
| NSAIDs (e.g., ibuprofen) | 1-2 hours | Hours to days | Stomach upset, kidney strain, high blood pressure | Temporary pain, mild symptoms |
| Physical Therapy | 4-12 weeks | Long-term if maintained | None | All stages, especially early OA |
Compared to steroids, hyaluronic acid works slower but lasts longer. Compared to pills like NSAIDs, it avoids stomach and heart risks. But it’s not a magic fix. Many people still need to keep doing exercises and managing their weight - the injections just give them breathing room.
What Are the Risks?
Most people tolerate the injections well. About 10% to 20% feel a little more pain or swelling in the knee for a day or two after the shot. That’s usually mild and goes away on its own. Less than 5% get noticeable swelling that lasts longer. Severe reactions - like allergic responses or joint infections - are extremely rare, under 0.1% of cases.
One thing to watch: if your knee swells up badly or gets hot and red days after the shot, call your doctor. That could be a sign of infection. Also, don’t do heavy lifting or high-impact activities for 48 hours after the injection. Light walking is fine.
Do They Really Work - Or Is It Just Placebo?
This is the big question. And the answer isn’t simple.
Some studies, like one from 2022, show HA injections give statistically better pain relief than saline (fake) shots. But the difference? Tiny. Often less than 9% on pain scales - too small to feel meaningful in daily life. A 2022 review of 50 years of data concluded these injections are "barely more effective than placebo." That’s why some doctors refuse to give them.
Yet, millions of people still get them. Medicare spent over $300 million on these shots in 2022. One in seven knee OA patients in the U.S. gets them as their first treatment. Why? Because for some, the relief is real. Even if it’s small, it’s enough to walk without pain, play with grandkids, or avoid surgery.
The truth? It works best for a subset of people - likely those with early to moderate damage, no major inflammation, and who respond well to joint lubrication. We don’t yet have a test to predict who will benefit. So doctors often try it when other options fail.
What Happens If It Doesn’t Work?
If you’ve had a full course of three or four shots and still feel the same pain after 12 weeks, it’s probably not helping you. There’s no point repeating the shots. Most experts agree: if it doesn’t work the first time, it won’t work later.
At that point, you’d move on to other options:
- Stronger physical therapy or custom orthotics
- Weight loss if you’re overweight
- Bracing to take pressure off the joint
- Alternative pain management like nerve blocks or radiofrequency ablation
- Joint replacement surgery - the most reliable long-term solution for advanced OA
There’s no shame in moving on. These injections aren’t a cure. They’re a tool - sometimes useful, sometimes not.
What’s Next for These Injections?
Researchers are working on better versions. New formulations aim to last longer with fewer shots. Some combine hyaluronic acid with anti-inflammatory drugs. Others use cross-linking to make the molecules more durable. One experimental product, already in trials, claims to last up to a year with just one injection.
Scientists are also trying to find biomarkers - things like blood or joint fluid tests - to predict who will respond. If we can identify those people ahead of time, we can stop wasting money and time on those who won’t benefit.
For now, the best advice is this: if you’re considering hyaluronic acid injections, go in with realistic expectations. Don’t expect to run marathons again. But if you can walk to the store without wincing, or sleep through the night, that’s progress.
Write a comment
Your email address will not be published.





4 Comments
I’ve had three rounds of these injections over the last five years, and honestly? The first one changed my life. I could finally walk to the mailbox without wincing. The second? Barely noticeable. The third? Zero effect. It’s like rolling dice-sometimes you hit, sometimes you don’t. But when it works, it’s not just pain relief-it’s dignity restored. Don’t give up if the first shot flops. Try the full course. And please, don’t let anyone tell you it’s all placebo. For some of us, it’s the only thing standing between us and a wheelchair.
The claim that hyaluronic acid injections are 'barely more effective than placebo' is not merely statistically accurate-it is methodologically indefensible. The 2022 meta-analysis cited fails to account for heterogeneity in molecular weight, injection technique, and baseline inflammation levels. Moreover, the use of saline as a control ignores the physiological impact of intra-articular volume displacement, which itself induces transient anti-inflammatory effects. To dismiss these interventions as 'placebo' is to misunderstand both biomechanics and neurophysiology. This is not medicine-it’s reductionist populism masquerading as evidence.
I’m a physical therapist in Portland, and I’ve seen patients go from barely walking to hiking again after these shots. Not because it’s magic-but because it gave them the window they needed to finally commit to PT. One woman, 72, told me she cried the first time she played with her grandkid without pain. That’s not placebo. That’s human. Let’s stop arguing about statistics and remember: medicine isn’t just about numbers. It’s about moments. 💪
I got the single-shot one last year. Felt a little weird for two days, then nothing. Waited 10 weeks. Still limping. Didn’t hurt to try, but I’m not doing it again. My doc said ‘some people just don’t respond’-which is fair. I’ve been doing daily squats and lost 15 lbs. My knee’s better now than it’s been in 10 years. Maybe the real treatment was just… moving more.