
Quick Summary
- Saxagliptin is a DPP‑4 inhibitor that lowers blood glucose with low risk of hypoglycemia.
- It can be combined with metformin or other agents for stronger control.
- Clinical data show modest reductions in HbA1c and cardiovascular events.
- Kidney‑friendly dosing expands use for patients with renal impairment.
- Understanding side‑effects and drug interactions helps maximize daily wellbeing.
When managing Saxagliptin a DPP‑4 inhibitor prescribed for Type 2 diabetes, many wonder whether the pill will actually make life feel easier. The answer is often yes-if you know how the drug works, who benefits most, and what pitfalls to avoid. Below we break down everything you need to feel confident about adding saxagliptin to your diabetes toolkit.
What Is Saxagliptin and How Does It Work?
Saxagliptin belongs to the class of DPP‑4 inhibitors that prevent the breakdown of incretin hormones. Incretins, mainly GLP‑1 and GIP, tell the pancreas to release insulin after a meal and to suppress glucagon, the hormone that raises blood sugar. By blocking the enzyme dipeptidyl‑peptidase‑4 (DPP‑4), saxagliptin keeps incretins active longer, leading to smoother post‑meal glucose curves without a big spike in insulin.
Why Choose a DPP‑4 Inhibitor?
Compared with older drugs like sulfonylureas, DPP‑4 inhibitors offer:
- Low risk of hypoglycemia because they only boost insulin when glucose is high.
- Weight neutrality-most patients neither gain nor lose significant weight.
- Convenient once‑daily oral dosing.
These benefits translate directly into day‑to‑day quality of life: fewer emergency snack episodes, less worry about sudden drops, and a simple pill routine.
Clinical Impact on Blood Sugar and HbA1c
Large‑scale trials, such as the SAVOR (Saxagliptin Assessment of Vascular Outcomes) study, showed an average reduction of 0.5-0.7 % in HbA1c a key marker of long‑term glucose control over 24 weeks when added to metformin. While not as dramatic as insulin, this drop is enough to move many patients from the “uncontrolled” to the “controlled” bracket (e.g., from 8.2 % to 7.5 %).
Beyond numbers, the SAVOR trial also reported a 15 % relative risk reduction in a composite of cardiovascular death, myocardial infarction, or stroke-an outcome that matters for overall wellbeing.
Who Benefits Most?
Ideal candidates include:
- Adults with Type 2 diabetes characterized by insulin resistance and relative insulin deficiency who are already on metformin but need additional glucose lowering.
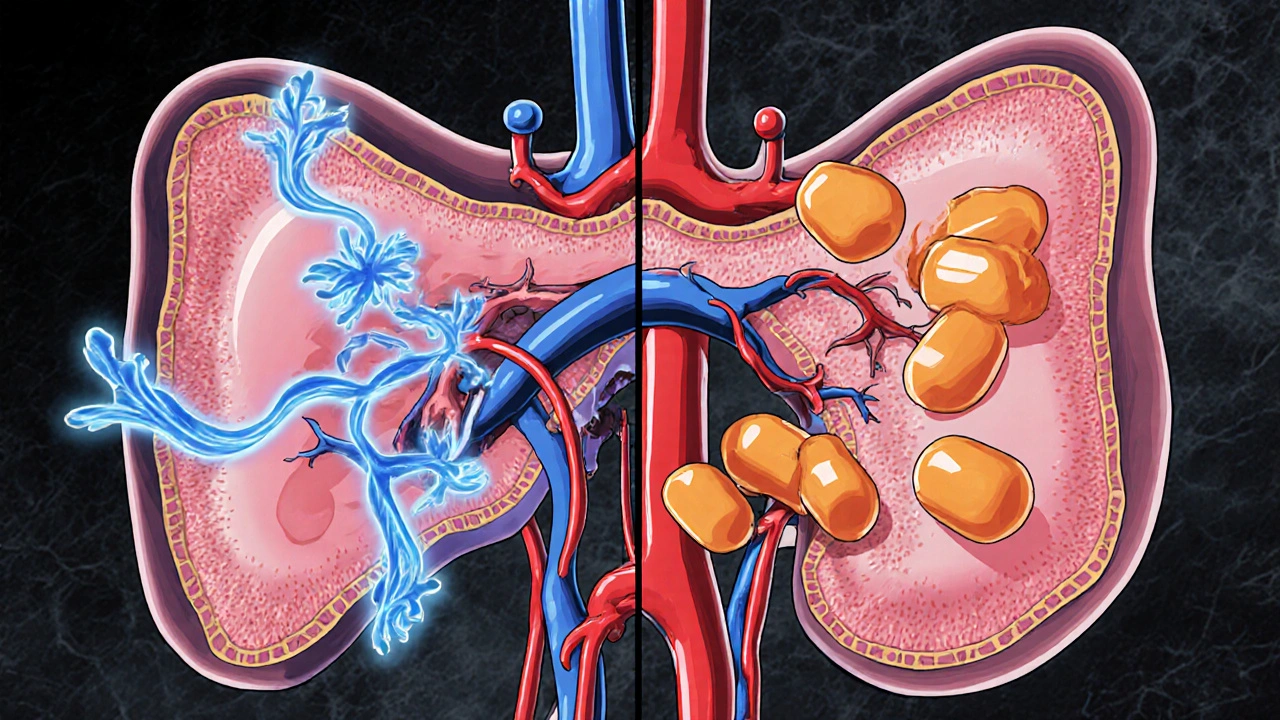
- Patients with mild to moderate kidney function impairment (eGFR ≥ 30 mL/min/1.73 m²)-saxagliptin can be used down to an eGFR of 30 without dose adjustment.
- Individuals who cannot tolerate weight‑gain side effects of sulfonylureas or the gastrointestinal upset of GLP‑1 agonists.
For those with severe renal disease (eGFR < 30), alternatives like linagliptin may be preferable.
Combining Saxagliptin with Other Medications
Most clinicians pair saxagliptin with Metformin the first‑line oral agent for Type 2 diabetes. The combo achieves an additive HbA1c drop of roughly 1 %.
If additional control is needed, a third agent such as a SGLT‑2 inhibitor (e.g., empagliflozin) or a basal insulin can be added. However, watch for overlapping side‑effects like urinary tract infections (SGLT‑2) or weight increase (insulin).
Safety Profile and Common Side‑Effects
Overall, saxagliptin is well‑tolerated. The most frequently reported events are mild gastrointestinal complaints (nausea, mild abdominal pain) and occasional upper‑respiratory infections.
Serious concerns to monitor:
- Heart failure risk: The SAVOR trial noted a slight uptick in hospitalization for heart failure (≈0.8 % vs 0.5 % on placebo). Patients with a history of CHF should discuss alternatives with their doctor.
- Pancreatitis: Rare but possible; seek immediate care for severe abdominal pain.
- Skin reactions: Rash or itching may occur, though uncommon.
Because saxagliptin does not generally cause hypoglycemia, you won’t need to constantly carry glucose tablets-another quality‑of‑life boost.
Drug Interactions You Need to Know
Some medicines can affect saxagliptin levels or vice‑versa. Key interactions include:
- CYP3A4 inhibitors such as ketoconazole, erythromycin, or grapefruit juice - may increase saxagliptin exposure; dose adjustment may be required.
- CYP3A4 inducers like rifampin or carbamazepine - can lower drug levels, reducing efficacy.
- Concurrent use with other DPP‑4 inhibitors offers no added benefit and raises cost without improving control.
Always tell your pharmacist about over‑the‑counter meds and supplements.
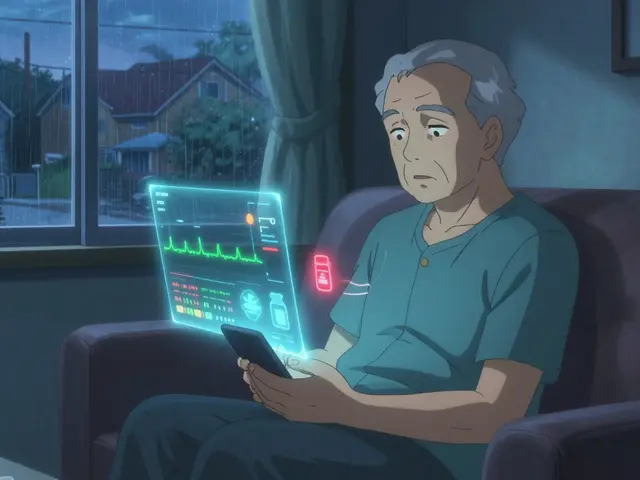
Monitoring and Follow‑Up
When you start saxagliptin, your doctor will typically check:
- Baseline HbA1c to gauge long‑term glucose control.
- Renal function (eGFR) before prescribing and annually thereafter.
- Blood pressure and lipid profile - many patients see modest improvements.
Re‑check HbA1c after 12 weeks; if the reduction is ≥0.5 %, the drug is likely helping. If not, dosage adjustment or a different agent may be needed.

Comparison with Other DPP‑4 Inhibitors
| Attribute | Saxagliptin | Sitagliptin | Linagliptin |
|---|---|---|---|
| Typical dose | 5 mg once daily | 100 mg once daily | 5 mg once daily |
| Renal adjustment needed? | Yes, if eGFR < 50 mL/min | Yes, if eGFR < 30 mL/min | No |
| HbA1c reduction (average) | 0.5-0.7 % | 0.5-0.8 % | 0.5-0.9 % |
| Heart‑failure signal | Small increase in hospitalization | Neutral | Neutral |
| Weight effect | Neutral | Neutral | Neutral |
If you have any heart‑failure concerns, sitagliptin or linagliptin may be safer choices. Otherwise, saxagliptin remains a solid, cost‑effective option.
Real‑World Stories
John, a 58‑year‑old accountant from Manchester, added saxagliptin to his metformin regimen after his HbA1c plateaued at 8.0 %. Within three months, his reading dropped to 7.2 %, and he reported fewer midday cravings. Because he rarely experienced low‑blood‑sugar symptoms, he felt more confident driving and traveling for work.
Maria, 45, struggled with mild kidney impairment (eGFR 35). Her endocrinologist chose saxagliptin because it can be used down to that level without dose change. After six months, Maria’s blood pressure improved and she hasn’t needed extra insulin flashes.
Tips to Maximize Quality of Life While on Saxagliptin
- Take the pill with or without food at the same time each day to build routine.
- Combine with a balanced diet rich in fiber-this helps the drug’s glucose‑lowering effect.
- Stay active; even a 30‑minute walk after meals can further blunt spikes.
- Use a simple glucometer to track fasting and post‑meal glucose; look for trends rather than occasional outliers.
- Keep a medication list handy and share it with any new healthcare provider.
Following these habits turns a once‑daily tablet into a catalyst for a steadier, more energetic life.
Frequently Asked Questions
Can I take saxophone with saxagliptin?
Saxagliptin does not affect your ability to play musical instruments. Enjoy your saxophone sessions!
How quickly does saxagliptin start lowering blood sugar?
Blood glucose begins to improve within a week, but the full HbA1c effect shows after 8-12 weeks of consistent use.
Is saxagliptin safe during pregnancy?
It is classified as pregnancy category C, meaning risk cannot be ruled out. Discuss alternatives with your obstetrician.
Do I need to monitor my kidney function while on saxagliptin?
Yes. Baseline eGFR and yearly checks ensure the dose remains appropriate and safe.
Can saxagliptin cause weight gain?
Weight change is typically neutral; most patients report no noticeable gain or loss.
What should I do if I miss a dose?
Take it as soon as you remember unless it’s almost time for the next dose. Then skip the missed one-don’t double up.
Are there any foods I must avoid?
No strict bans, but limit excessive alcohol and high‑sugar snacks that can overwhelm any medication’s effect.
By understanding how Saxagliptin works, who it helps most, and how to pair it with lifestyle steps, you can turn a prescription into a real boost for daily comfort and long‑term health.
Write a comment
Your email address will not be published.





14 Comments
Honestly, reading about saxagliptin feels like watching a drama unfold in a pharmacy aisle-glucouse levels tango, side‑effects whisper, and hope glimmers. The drug’s low hypoglycemia risk is a real game‑changer for anyone scared of sudden lows. It pairs nicely with metformin, making the combo feel like a well‑rehearsed duet. For those with mild kidney issues, the dosing is just as gentle as a lullaby. Overall, it’s a solid addition, even if the name makes you think of a saxophone.
From a mechanistic standpoint, saxagliptin inhibits DPP‑4, prolonging incretin activity, which directly boosts insulin secretion post‑meal while curbing glucagon. Clinically, that translates to a modest 0.5‑0.7% HbA1c reduction, which is quite meaningful for many patients. Moreover, its weight‑neutral profile and once‑daily dosing enhance adherence, especially in busy lifestyles.
You're right on the money-adding saxagliptin often feels like giving your regimen a confidence boost. It’s easy to incorporate, and the low hypoglycemia risk means fewer “oops” moments during the day.
Sounds like a decent option for stable glucose control.
Let’s break it down: saxagliptin is a DPP‑4 inhibitor, so think of it as an enzymatic brake on incretin degradation-fancy talk for “keeps your pancreas responsive.” The cardiovascular signal is a modest 15% relative risk dip, which in the grand scheme is like a bonus feature on a streaming service-nice but not a show‑stopper. For patients wary of weight gain, its neutral impact is a win, especially compared to sulfonylureas that can add the “fluff” factor. Just keep an eye on that heart‑failure signal; it’s the only real red flag in an otherwise smooth profile.
Saxagliptin’s renal dosing is straightforward, but patients below eGFR 30 should consider alternatives.
Great point about routine-taking the pill at the same time each day builds consistency. Pair it with a fiber‑rich diet, and you’ll notice steadier post‑meal glucose spikes. Also, a simple walk after meals can amplify the drug’s effect without any extra cost.
Okay, let’s dive deep because the nuance matters more than a headline grab. First, saxagliptin’s pharmacokinetics are such that it reaches steady‑state concentrations in about five days, not instantly, so patience is key. Secondly, the drug’s half‑life sits around 12 hours, which is why a once‑daily dose works-no need for night‑time dosing that can disturb sleep patterns. Third, when you combine it with metformin, the additive HbA1c drop is roughly 1%, which is clinically relevant and often enough to push a patient from the “uncontrolled” to the “controlled” category. Fourth, renal considerations are pivotal; while the label allows use down to eGFR 30, the clearance does decrease, so you might need to monitor creatinine more often. Fifth, the heart‑failure signal observed in the SAVOR trial, although modest, should not be dismissed-if you have a history of CHF, discuss alternatives such as linagliptin. Sixth, the pancreatitis risk is rare but real; any acute abdominal pain warrants immediate evaluation. Seventh, drug‑drug interactions-CYP3A4 inhibitors like ketoconazole can raise saxagliptin levels, possibly necessitating dose adjustments. Eighth, conversely, strong inducers like rifampin can dilute its effect, leading to sub‑therapeutic exposure. Ninth, unlike GLP‑1 agonists, saxagliptin doesn’t cause significant nausea, making it more tolerable for patients sensitive to GI upset. Tenth, the weight neutrality is a double‑edged sword-it won’t cause weight gain, but it also won’t promote weight loss which some patients desire. Eleventh, adherence improves with the pill’s simplicity; no titration schedule, just one tablet a day. Twelfth, cost considerations matter-saxagliptin is often cheaper than newer agents, which can affect insurance coverage decisions. Thirteenth, monitoring should include baseline HbA1c, eGFR, and periodic cardiovascular assessment if risk factors exist. Fourteenth, patient education is paramount; they need to understand that this isn’t a cure but a tool to smooth glucose curves. Fifteenth, lifestyle integration-regular meals, balanced carbs, and activity amplify the drug’s benefit. Finally, if after 12 weeks the HbA1c hasn’t dropped at least 0.5%, you might need to reassess the regimen or consider adding a third agent.
While the data sounds promising, one must remember that a 0.5% HbA1c drop is modest and doesn’t justify blanket adoption. The heart‑failure uptick, albeit small, could be a deal‑breaker for high‑risk patients. In practice, I’ve seen clinicians overlook these nuances in favor of marketing hype.
Engaging with your doctor about renal dosing can prevent unnecessary complications. Keep a medication list handy for any new prescriber.
Mixing saxagliptin with an SGLT‑2 inhibitor can give you that extra 1% HbA1c reduction, but watch for urinary tract infections. Always inform your pharmacist about over‑the‑counter supplements.
In summation, saxagliptin epitomizes a judicious balance between efficacy and tolerability, rendering it a commendable adjunct in the therapeutic armamentarium for type‑2 diabetes mellitus. Its pharmacodynamic profile, characterised by incretin preservation, confers a modest yet clinically salient decrement in glycated haemoglobin. Nevertheless, prudent patient selection remains indispensable to mitigate the marginally elevated risk of congestive heart failure.
Honestly, the whole thing sounds like a marketing fluff parade-decent enough if you’re desperate, but don’t expect miracles.
One might argue that saxagliptin’s modest HbA1c reduction is merely a statistical footnote, yet for many patients it constitutes a tangible quality‑of‑life improvement. Thus, it deserves a measured place in the treatment algorithm, not a hasty blanket endorsement.