Every year, millions of people take the right medicine at the right time - but millions more don’t. Some get the wrong dose. Others take pills that clash with their other meds. Some never even know what they’re supposed to be taking. And too often, the people who could catch these mistakes - the patients themselves - aren’t asked to help.
Medication errors aren’t just rare accidents. They’re systemic. The World Health Organization says avoidable harm from medications affects 1 in 20 people globally. In the U.S. alone, these errors lead to over 7,000 deaths each year. But here’s the thing: patients are the last line of defense. And when they’re engaged, they catch errors that even doctors and pharmacists miss.
What Does It Really Mean to Be an Active Patient?
Being an active patient doesn’t mean becoming a medical expert. It means knowing your own body, your own meds, and having the confidence to ask questions. It’s not about blaming patients when things go wrong - it’s about giving them the tools to be part of the solution.
Think about it: you take your pills every day. You see how your body reacts. You notice if something feels off. No nurse or pharmacist sees you 24/7. But you do. That’s why your role isn’t optional - it’s essential.
The Seven Things You Can Do Right Now
Research from the Institute for Safe Medication Practices shows seven simple actions can cut your risk of harm by more than a third. You don’t need a degree. You just need to pay attention.
- Know your meds by name and why you’re taking them. If your doctor says, “Take this for your blood pressure,” ask: “What’s the name? What does it actually do?” Knowing this cuts error risk by 35%.
- Understand your dosing schedule. “Once a day” doesn’t mean the same thing to everyone. Is it morning? After food? At bedtime? Ask for clarity. People who get this right are 28% less likely to skip or double up.
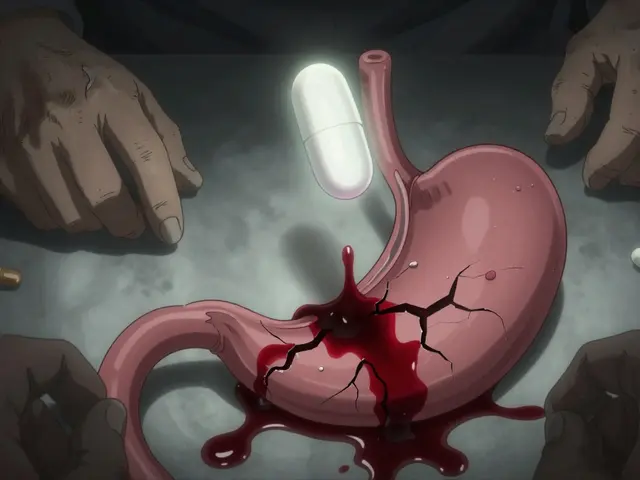
- Learn the side effects. If you feel dizzy, nauseous, or unusually tired, don’t assume it’s just “aging.” It might be your medicine. Recognizing early signs helps catch problems before they turn serious - and 63% of adverse events are caught this way.
- Check what the pill looks like. If your pill suddenly changes color, shape, or size, ask. One in five dispensing errors are caught when patients notice something looks off.
- Question changes. If a new prescription comes in that doesn’t match what you expected - say, a higher dose or a drug you’ve never heard of - speak up. Patients who ask about changes catch 15% of prescription errors.
- Tell your provider about everything you take. That herbal tea? The ibuprofen you grab for headaches? The gummy vitamins? All of it matters. Reporting all medications cuts dangerous interactions by 22%.
- Join in on medication reviews. Every time you switch doctors, go to the hospital, or get discharged, ask for a full list of your meds to be reviewed. Patients who do this cut discrepancies in their meds by half.
Keep a Personal Medication List
Most people don’t have one. But if you do, you’re already ahead of 70% of patients.
A personal medication list (PML) is just a piece of paper - or a note on your phone - with:
- The name of each medicine
- The dose
- How often to take it
- Why you’re taking it
- Who prescribed it
Update it every time something changes. Bring it to every appointment. Studies show people who use a PML have 42% fewer mistakes when moving between hospitals, clinics, or nursing homes.
There’s no app needed. Just write it down. Or use a free template from the Agency for Healthcare Research and Quality.

Why Some Patients Don’t Speak Up
It’s not because they’re careless. It’s because they’re afraid.
One in three patients say they’ve felt dismissed when they questioned a medication. One woman on Reddit shared how she was told, “You’re overreacting,” after asking about her new antibiotic. Two days later, she had a severe allergic reaction.
Doctors aren’t always trained to welcome questions. But that’s changing. The American Medical Association now recommends structured safety training at every visit. And studies show patients who get this training are nearly twice as likely to catch errors.
Here’s how to speak up without sounding confrontational:
- “I want to make sure I understand this correctly.”
- “Can you explain why this medicine was added?”
- “I’ve never taken this before - what should I watch for?”
You’re not challenging their expertise. You’re helping them do their job better.
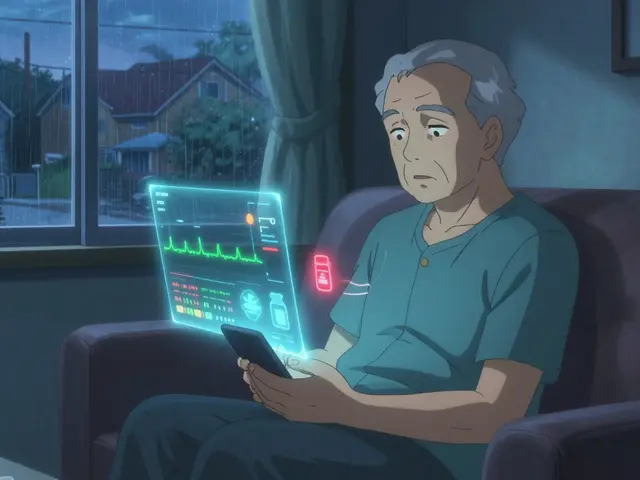
The Digital Divide and Who Gets Left Behind
Many clinics now offer apps to track meds. But not everyone can use them.
Only 44% of people over 65 regularly use digital tools for meds. That’s not because they’re resistant - it’s because the apps are often too complex. One elderly user on Trustpilot wrote: “Too many steps just to check if I took my pill.”
Meanwhile, younger patients using interactive apps see 25% better safety outcomes than those using static lists.
Here’s the truth: tech helps - but it’s not the only way. A printed list, a pill organizer with alarms, or even a family member helping you check your meds can be just as powerful.
What Works - And What Doesn’t
Not all education helps equally.
Just handing out a pamphlet? That reduces errors by only 8%. But teaching patients with the “teach-back” method - where they repeat the info back in their own words - boosts safety behavior from 31% to 67%.
And programs like “Ask Me 3” - which asks patients: “What is my main problem? What do I need to do? Why is it important?” - cut errors by 31% compared to standard instructions.
On the flip side, passive info - like a printed discharge sheet with tiny print and medical jargon - fails 63% of the time. That’s because 88 million Americans have trouble understanding basic health info.

Real Stories - What Happens When Patients Act
A mother in Ohio noticed her child’s new antibiotic looked different. She called the pharmacy. Turns out, the wrong drug had been filled - a 10-fold overdose risk.
A man in Florida asked why his blood thinner dose had doubled. His doctor admitted it was a mistake - the system had auto-filled the wrong number.
A nurse in New York says 70% of the near-misses she’s seen were caught because a patient said, “That doesn’t look right.”
These aren’t lucky breaks. They’re proof that patients aren’t just recipients of care - they’re part of the safety net.
What’s Changing - And What’s Coming
Hospitals are starting to treat patients as partners. The Joint Commission now requires medication reconciliation at every transition of care. The FDA has trained over 12,000 patients as “Safety Ambassadors” to teach others in their communities. By 2027, 85% of healthcare organizations plan to have formal patient safety roles.
And AI is coming. New tools will soon let you snap a photo of your pill and instantly verify it against your prescription. But even these won’t replace your voice. They’ll just support it.
The goal isn’t to make you a pharmacist. It’s to make you a confident, informed partner in your own care.
Start Today - One Small Step
You don’t need to overhaul your life. Just pick one thing:
- Write down your current meds - even if it’s just on your phone.
- Next time you get a new prescription, ask: “What’s the name? Why am I taking it?”
- Before you leave the clinic, say: “Can we review my list together?”
These aren’t big asks. But they’re powerful. Every time you speak up, you’re not just protecting yourself - you’re helping the whole system work better.
Medication safety isn’t just about hospitals and pharmacies. It’s about you. And you’re more important to it than you think.