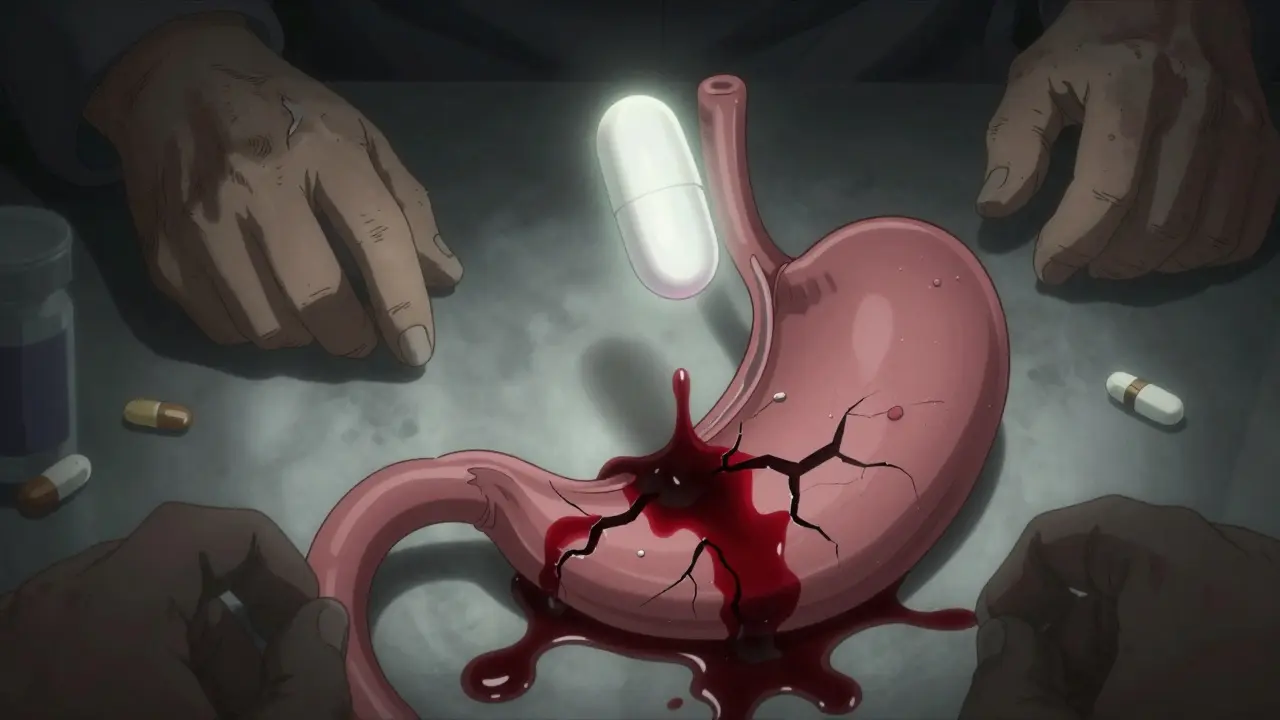
Every year, millions of people reach for ibuprofen, naproxen, or diclofenac to ease aching joints, headaches, or back pain. These are NSAIDs - non-steroidal anti-inflammatory drugs - and they work well. But for many, especially older adults or those with existing health issues, they come with a hidden danger: gastrointestinal bleeding. It’s not rare. It’s not theoretical. It’s a real, life-threatening side effect that often goes unnoticed until it’s too late.
How NSAIDs Damage Your Stomach and Gut
NSAIDs block enzymes called COX-1 and COX-2. COX-2 causes inflammation and pain, so blocking it helps. But COX-1 protects the stomach lining by making mucus and blood flow that keep the tissue healthy. When NSAIDs shut down COX-1, that protection vanishes. The stomach acid starts eating away at the lining. That’s how ulcers form - and how bleeding starts.This isn’t just about big, obvious ulcers. The damage can be silent. Many people don’t feel pain. Instead, they slowly lose blood in tiny amounts. Their iron levels drop. They get tired, pale, dizzy. By the time they see a doctor, they’ve lost enough blood to need a transfusion. One Reddit user shared how their 78-year-old mother needed three units of blood after months of unexplained fatigue - all from daily ibuprofen she never told her doctor about.
Studies show NSAID users are 3 to 4 times more likely to have upper GI bleeding than non-users. And it’s not just the stomach. Up to a third of NSAID-related bleeds happen in the small intestine or colon. You don’t even need a visible ulcer for bleeding to occur. The lining just gets worn thin, and blood leaks out.
Not All NSAIDs Are the Same
Some NSAIDs are riskier than others. Non-selective ones - like ibuprofen, naproxen, and diclofenac - hit both COX-1 and COX-2. That means more stomach damage. Selective COX-2 inhibitors - like celecoxib - spare COX-1, so they’re gentler on the gut. A 2000 Lancet study found celecoxib caused half the number of serious ulcers compared to ibuprofen.But there’s a catch. COX-2 inhibitors raise heart attack and stroke risk. Rofecoxib (Vioxx) was pulled from the market in 2004 after trials showed it doubled heart attack risk. Celecoxib still carries a warning, but it’s considered safer than older COX-2 drugs. So you’re trading one risk for another.
For most people, the safest choice isn’t switching drugs - it’s protecting the stomach while using the NSAID they need.
Who’s Most at Risk?
Not everyone who takes NSAIDs bleeds. But some people are far more vulnerable. The American College of Gastroenterology lists clear risk factors:- Age 70 or older
- History of peptic ulcer or GI bleeding
- Taking blood thinners like warfarin or aspirin
- Using corticosteroids (like prednisone)
- Taking more than one NSAID at a time
- High-dose NSAIDs (over 1,200 mg of ibuprofen daily)
- Chronic conditions like heart failure or kidney disease
If you have two or more of these, your risk jumps dramatically. A 2017 Cochrane review found that patients with two risk factors had a 70% higher chance of bleeding than those with none. And here’s the scary part: many don’t know they’re at risk. A 2022 survey found that 63% of NSAID users had stomach symptoms - bloating, nausea, dark stools - but only 37% told their doctor.

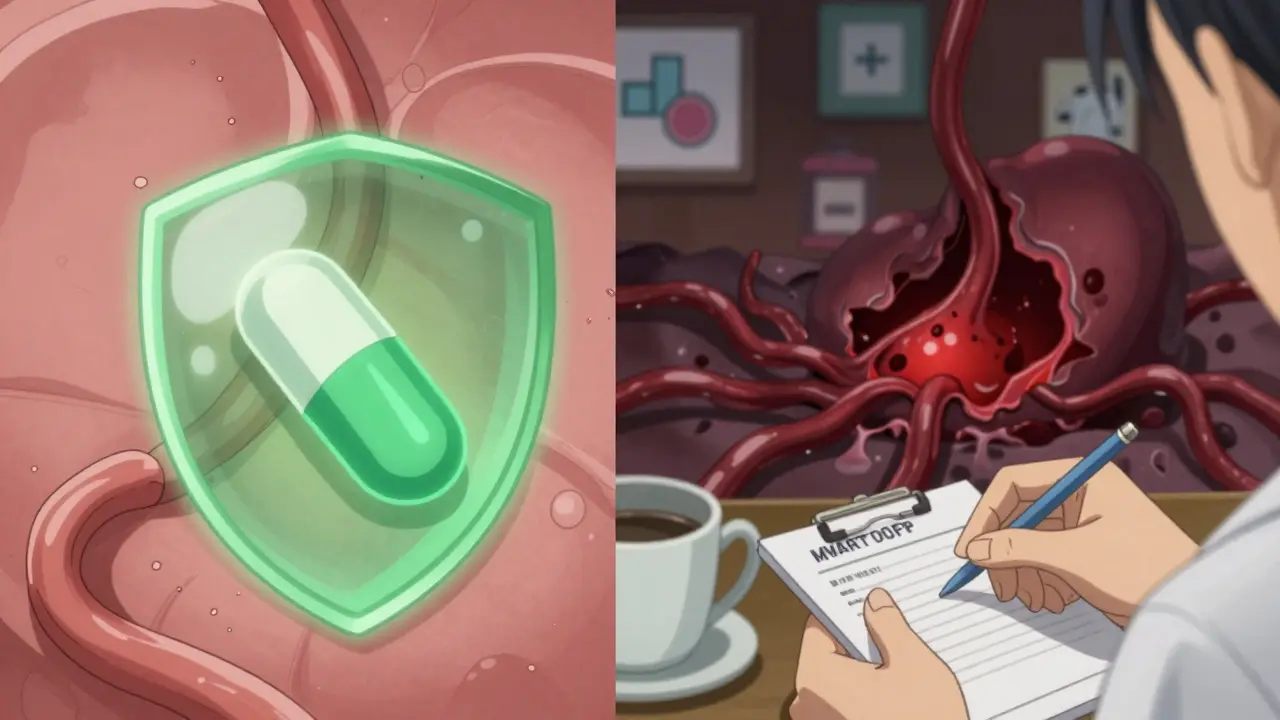
How to Protect Yourself
The good news? You can cut your risk of bleeding by up to 75%. The best tool? Proton pump inhibitors - or PPIs.PPIs like omeprazole, esomeprazole, and pantoprazole shut down stomach acid production. They don’t fix the NSAID damage, but they give the lining time to heal. A 2017 analysis of 33 trials showed PPIs reduced serious NSAID-related ulcers by 75%. That’s not a small benefit. That’s life-saving.
Another option is misoprostol, a drug that replaces the protective mucus lost from NSAIDs. But it causes diarrhea in up to 20% of users and cramps in 15%. Most people can’t tolerate it long-term. That’s why PPIs are the standard.
There’s also a newer option: Vimovo. It’s a single pill that combines naproxen with esomeprazole. In a 2022 trial, only 7.3% of people on Vimovo had ulcers compared to 25.6% on naproxen alone. It’s more expensive, but for high-risk patients, it’s a smart choice.
What You Should Do Right Now
If you take NSAIDs regularly - even just a few times a week - ask yourself these questions:- Are you over 65?
- Have you ever had an ulcer or GI bleed?
- Do you take aspirin, warfarin, or steroids?
- Do you feel bloated, nauseous, or unusually tired?
If you answered yes to any of these, talk to your doctor. Don’t wait for bleeding to happen. Get a PPI prescribed. Switch to a COX-2 inhibitor if appropriate. Or better yet - see if you can reduce NSAID use entirely.
For arthritis or chronic pain, physical therapy, weight loss, or acetaminophen might be safer alternatives. NSAIDs aren’t the only option. And for occasional headaches or muscle soreness, taking them every day isn’t necessary.
The Bigger Picture
NSAIDs cause about 107,000 hospitalizations and 16,500 deaths in the U.S. every year. That’s more than traffic accidents. The cost? Over $2 billion annually. And yet, they’re still the go-to for pain. Why? Because they work. They’re cheap. And most people don’t realize how dangerous they can be.Regulators have tried. Since 2005, the FDA has required black box warnings on all NSAID labels about GI and heart risks. But warnings on a pill bottle don’t help if you don’t read them - or if your doctor doesn’t explain them.
Real change happens when patients and doctors talk. When someone says, “I take ibuprofen every day for my knees,” and the doctor replies, “Let’s put you on omeprazole too.” That’s the moment a bleed gets prevented.
What’s Next?
Researchers are working on better options. New drugs called CINODs - like naproxcinod - combine NSAIDs with nitric oxide, which helps protect the stomach lining. Early trials show 50% fewer ulcers than traditional NSAIDs. But they’re still in testing.For now, the best strategy is simple: know your risk. Use the lowest dose for the shortest time. And if you’re high-risk, always pair NSAIDs with a PPI. It’s not extra. It’s essential.
NSAIDs aren’t evil. They’re tools. But like any tool, they can hurt you if you use them wrong. Don’t assume you’re safe just because you feel fine. Bleeding doesn’t always come with pain. Sometimes, it comes with silence - and fatigue. And by the time you notice, it’s already too late.
Can I take ibuprofen if I’ve had a stomach ulcer before?
No, not without protection. If you’ve had a peptic ulcer or GI bleed, taking NSAIDs like ibuprofen again puts you at very high risk of another bleed - up to 5 times higher. If you need pain relief, your doctor should prescribe a COX-2 inhibitor like celecoxib along with a proton pump inhibitor (PPI) like omeprazole. This combination reduces your risk by about 75%. Never restart NSAIDs after a previous bleed without medical advice.
Do over-the-counter NSAIDs carry the same risk as prescription ones?
Yes, absolutely. Many people think OTC NSAIDs are safer because they’re available without a prescription. But the risk of bleeding is the same whether you buy ibuprofen at the pharmacy or get a prescription for naproxen. In fact, a 2021 study found that 26% of people take OTC NSAIDs at doses higher than recommended - often daily - without telling their doctor. This makes them more dangerous, not less.
How long does it take for NSAIDs to cause stomach damage?
Damage can start within days. Studies show that even short-term use - just one to two weeks - can cause visible erosions in the stomach lining. For some people, especially older adults or those with risk factors, bleeding can occur within the first week. That’s why you can’t assume you’re safe just because you’ve taken NSAIDs for years without problems. Risk builds over time, and it can strike suddenly.
Are PPIs safe to take long-term with NSAIDs?
For most people, yes. PPIs like omeprazole have been used safely for decades in patients on long-term NSAIDs. The benefits of preventing life-threatening bleeding far outweigh the risks of long-term PPI use. That said, long-term PPIs can slightly increase the risk of bone fractures, kidney issues, or low magnesium. But these are rare. Your doctor can monitor you and adjust if needed. Never stop a PPI without talking to your doctor - stopping suddenly can cause rebound acid.
What are the signs of NSAID-induced bleeding?
Signs can be subtle. Overt bleeding means black, tarry stools (melena) or vomiting blood. But most bleeding is occult - hidden. Look for unexplained fatigue, pale skin, dizziness, or shortness of breath - these can mean low iron from slow blood loss. A simple blood test can check your hemoglobin and iron levels. If you’re on NSAIDs and feel unusually tired, don’t ignore it. Get tested.
Is there a safer NSAID for the stomach?
Celecoxib (Celebrex) is the safest NSAID for the stomach among commonly used options - it causes about half the ulcers of ibuprofen or naproxen. But it’s not risk-free. It still carries a cardiovascular warning. The best approach isn’t finding the “safest NSAID,” but using the lowest effective dose for the shortest time, and always pairing it with a PPI if you’re at risk. For many, acetaminophen (paracetamol) is a better first choice for pain.
Write a comment
Your email address will not be published.





8 Comments
I used to pop ibuprofen like candy for my lower back. Then one day I just felt... drained. Like my bones were made of wet cardboard. Got a blood test-hemoglobin was 8.5. Turns out I’d been bleeding silently for months. My doctor said if I’d waited another two weeks, I might’ve needed an ICU bed. Now I take naproxen with omeprazole. No more fatigue. No more scares. Just because you don’t feel pain doesn’t mean your gut isn’t screaming.
It’s wild how we treat our bodies like machines you can just keep running on duct tape and caffeine. We’ll take a pill to numb the symptom but never ask why the machine broke in the first place. Maybe the real problem isn’t NSAIDs-it’s that we’ve forgotten how to rest. 🤔
My grandpa took aspirin every day for 40 years and never had a single ulcer. He also ate bacon for breakfast, smoked cigars, and walked 5 miles daily. Maybe the real villain isn’t the drug-it’s the sedentary, processed-food lifestyle we’ve normalized.
The COX-1/COX-2 dichotomy is a useful heuristic, but it’s reductive. The gut microbiome modulates NSAID-induced injury-certain strains of Lactobacillus can upregulate mucosal defense pathways. PPIs suppress gastric acid, yes, but they also alter microbiota composition, potentially increasing susceptibility to C. diff. So while PPIs reduce ulceration, they may introduce other dysbiosis-related risks. We’re playing whack-a-mole with physiology here. The real solution? Personalized pharmacogenomics. Not blanket prescriptions.
And before you say ‘that’s too expensive’-the cost of a GI bleed is $25K minimum. Investing in precision medicine is cheaper than emergency transfusions.
It is, frankly, a disgrace that over-the-counter NSAIDs are sold without mandatory physician consultation. The FDA’s black-box warning is a pathetic gesture toward responsibility. The pharmaceutical industry has successfully marketed these drugs as ‘safe’ through aggressive advertising campaigns targeting the elderly and fitness enthusiasts alike. This is not a medical issue-it is a corporate malfeasance disguised as consumer autonomy.
Wait-so you’re telling me that the same pills that help me hike with my grandkids are quietly killing me?? And the doctors just shrug and hand me a PPI like it’s a lollipop?? What’s next? They’ll give me a sugar pill to counteract the sugar pill?? This system is BROKEN. 🤬
They’re all in on it. Big Pharma, the FDA, the AMA-they all get kickbacks from PPI manufacturers. You think they want you to heal? No. They want you to buy more pills. NSAIDs? Fine. But PPIs? That’s the real money-maker. And they’ll scare you into taking them forever. Wake up. 🇺🇸
My mom took naproxen daily for arthritis. She never had symptoms. Then she passed out at the grocery store. Turned out she’d lost half her blood volume. She’s fine now-on celecoxib + omeprazole. But she almost didn’t make it. If you’re on NSAIDs and feel even a little off, get your blood checked. Seriously. Just do it.