
Every year, more than 90% of prescriptions in the U.S. are filled with generic drugs. They’re cheaper, just as effective for most people, and save the healthcare system billions. But sometimes, a doctor says: no. Not this time. I need the brand name. That’s not a request. It’s a legal override.
What Exactly Is a Prescriber Override?
A prescriber override is when a doctor legally blocks a pharmacist from swapping a brand-name drug for a cheaper generic version. It’s built into state laws that let pharmacists substitute generics by default - unless the doctor says otherwise. This isn’t about personal preference. It’s about clinical necessity. Some patients can’t safely switch. A tiny difference in how a drug is made can cause serious harm.
Think of it like this: most cars run fine on regular gas. But if your engine is tuned for premium, using regular could damage it. For drugs like warfarin, levothyroxine, or phenytoin, the difference between generics isn’t just about price - it’s about stability, absorption, and safety. These are narrow therapeutic index drugs. Even small changes in blood levels can lead to seizures, blood clots, or thyroid storms.
How It Works: The DAW Code System
The override doesn’t happen with a verbal request. It’s coded. Pharmacists rely on the Dispense as Written (DAW) system, a national standard created by the National Council for Prescription Drug Programs. The most common override code is DAW-1: "Substitution Not Allowed by Prescriber."
That code has to be clearly marked on the prescription - whether it’s handwritten, typed in an electronic system, or sent via e-prescribing. If it’s missing or unclear, the pharmacist is legally allowed to substitute the generic. And that’s where things go wrong.
States don’t agree on how to write it. In Illinois, the prescriber must check a box labeled "May Not Substitute." In Kentucky, they must handwrite "Brand Medically Necessary." In Massachusetts, "No Substitution" is enough. In Oregon, a phone call works. But if a doctor in Texas writes "Do Not Substitute" and the pharmacy’s system only recognizes "DAW-1," the generic still gets dispensed. And the patient doesn’t know.
Why Doctors Override: The Real Medical Reasons
Not every override is justified. But when done right, it saves lives.
- Narrow therapeutic index drugs: Warfarin (blood thinner), levothyroxine (thyroid), phenytoin (seizure control). Even 10% variation in absorption can cause overdose or treatment failure.
- Allergies to inactive ingredients: Some generics use different fillers, dyes, or preservatives. A patient allergic to lactose or FD&C yellow dye might react to a generic version of the same drug.
- Therapeutic failure: If a patient was stable on a brand, then switched to a generic and had a seizure, worsening depression, or uncontrolled blood pressure - the doctor must override to get them back on what worked.
- Pediatric or elderly patients: Their bodies process drugs differently. Consistency matters more.
According to Avalere Health, DAW-1 overrides are most common in anticonvulsants (14.8% of prescriptions) and psychiatric drugs (12.3%). These aren’t random choices. They’re based on real data showing higher failure rates with generics in these classes.
The Hidden Cost: When Overrides Go Wrong
Prescriber overrides aren’t free. On average, a DAW-1 prescription costs 32.7% more than a substituted generic. That’s $112 instead of $84 for a 30-day supply. Multiply that across millions of prescriptions, and it adds up.
But the bigger problem isn’t cost - it’s confusion. A 2010 study found only 58.3% of physicians understood their own state’s override rules. One doctor in Florida thought writing "Brand Only" was enough. The pharmacy ignored it. The patient got the generic. Two weeks later, they were in the ER with toxic levels of phenytoin.
Electronic health records make it worse. Many systems default to generic substitution. If the doctor doesn’t actively change the setting, the override doesn’t happen. And most don’t even know they’re supposed to.
Pharmacists report that 68% of override rejections come from improper documentation. A handwritten note on a paper script? Fine. A typed note in an EHR that doesn’t map to the pharmacy’s system? Useless.
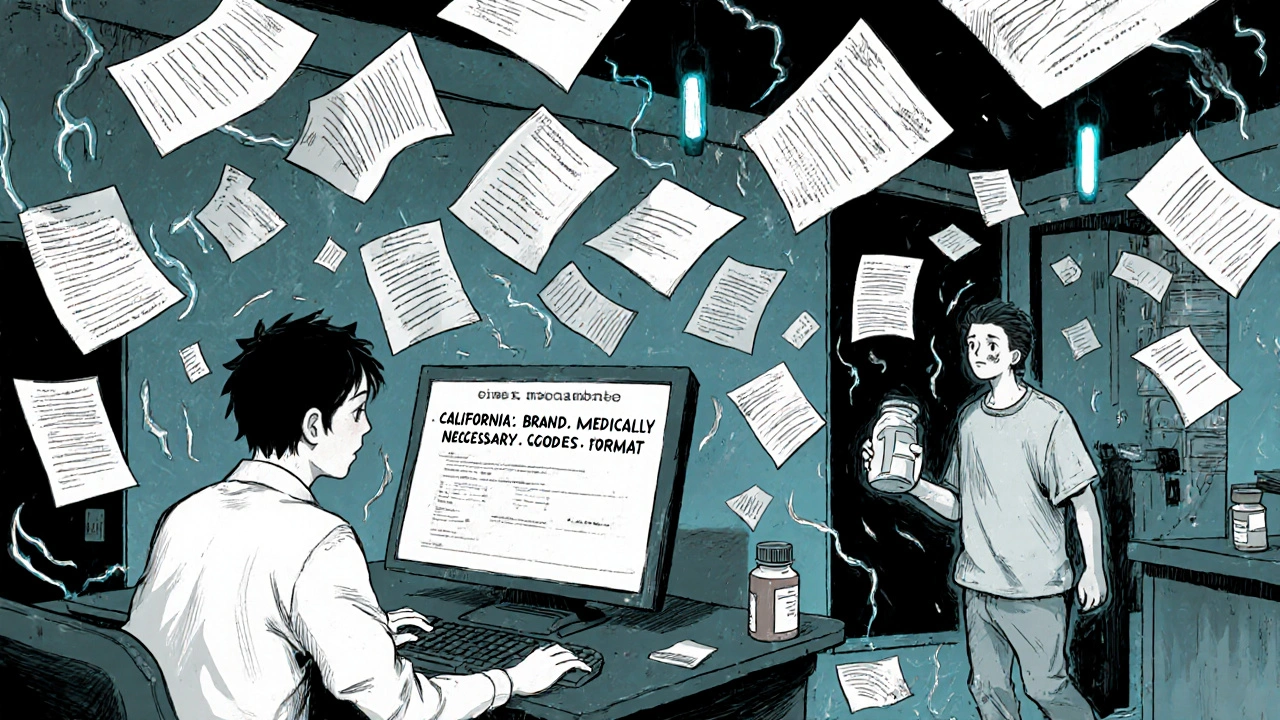
State Laws: A Patchwork That Confuses Everyone
The U.S. has 50 different rulebooks. That’s not a system. It’s a minefield.
Thirty-five states require pharmacists to substitute generics unless the doctor says no. Fifteen states let pharmacists decide. Some states require patient consent before substitution. Others don’t. In presumed consent states, the pharmacist can switch the drug without telling the patient - unless the doctor overrides.
Here’s how it breaks down:
| State | Override Requirement | Acceptable Format |
|---|---|---|
| California | "Brand Medically Necessary" | Handwritten or electronic, with signature |
| Texas | Two-line format | Must include "Dispense as Written" and prescriber signature |
| Michigan | "DAW" or "Dispense as Written" | Handwritten only on paper scripts |
| Oregon | No substitution specified | Written, phone, or electronic - no default values |
| Illinois | Check the box | Pre-printed form with "May Not Substitute" |
The FDA’s Orange Book tells pharmacists which generics are therapeutically equivalent. But it’s not law. States use it as a guide - and some don’t even check it. That means a doctor might override a drug that’s perfectly substitutable, thinking it’s risky. Or worse - they might not override one that actually needs it.
Real Stories: When Overrides Fail
On Reddit, a physician posted about a patient who developed thyroid storm after being switched from brand levothyroxine to a generic. The doctor had written "DAW-1" - but the EHR auto-filled it as "substitute allowed." The patient ended up in intensive care.
In Michigan, a clinic tracked override errors for a year. They found 37% of DAW-1 requests were processed incorrectly because the EHR didn’t match the state’s format. After they created a standardized template and trained staff, errors dropped by 42%.
The Institute for Safe Medication Practices documented 27 serious adverse events between 2018 and 2022 from improper generic substitution of warfarin, levothyroxine, or phenytoin. All of them involved a missing, unclear, or ignored override.
What Doctors Need to Do Right Now
If you prescribe any of these drugs - or any drug where consistency matters - here’s what you must do:
- Know your state’s rules. Visit the National Association of Boards of Pharmacy’s interactive map. It’s updated quarterly.
- Use the right code. Don’t write "no generic." Write "DAW-1" or the exact phrase your state requires.
- Check your EHR. Make sure your template matches your state’s law. If it doesn’t, customize it.
- Confirm with the pharmacy. If a patient says they got the wrong drug, call the pharmacy. Ask what code was used.
- Document the reason. Not just "DAW-1" - write "Therapeutic failure with generic" or "Allergy to dye in generic." It helps if the payer questions it.
It adds 1.7 minutes per prescription. But it prevents hospitalizations. That’s worth it.
The Bigger Picture: Cost vs. Safety
Generics saved $2.2 trillion between 2010 and 2019. That’s huge. But forcing substitution where it’s unsafe doesn’t save money - it costs more. Hospital stays, ER visits, lost work time - those bills are way higher than the drug difference.
Insurance companies hate DAW-1. Express Scripts says 18.4% of their brand-drug spending is avoidable because of incorrect overrides. But they’re not looking at the clinical side. They’re looking at the bottom line.
Meanwhile, the federal government is trying to fix this. A 2023 bill proposed a national override standard. The NCPDP is updating e-prescribing rules to embed state requirements directly into software by late 2024. That’s progress.
But until then, the burden is on the doctor. You’re the last line of defense. If you don’t override properly, no one else will.
What’s Next?
Biologics and biosimilars are coming. These are complex drugs - think insulin, rheumatoid arthritis treatments, cancer drugs. They’re not like simple pills. Switching them isn’t like swapping one brand of aspirin for another.
The FDA’s Orange Book now includes biosimilar interchangeability codes. That means in the next few years, prescriber overrides will be needed for these too. And the same confusion will follow.
The system isn’t broken. It’s just outdated. It was built for pills. Now we need it to handle complex biologics, patient-specific needs, and digital prescriptions across state lines.
For now, the rule is simple: if you’re not sure, override. If you’re sure it’s safe to switch, don’t. But always document why.
Can a pharmacist override a doctor’s DAW-1 request?
No. Once a prescriber uses a valid DAW-1 code, the pharmacist is legally required to dispense the brand-name drug. They cannot substitute a generic without violating state law. If they do, they risk losing their license.
What if the patient wants the generic even though the doctor wrote DAW-1?
The doctor’s order takes priority. Even if the patient asks for the cheaper version, the pharmacist must follow the prescriber’s instructions. Patient preference doesn’t override a DAW-1. However, if the patient refuses the brand and insists on the generic, the doctor can re-evaluate and issue a new prescription without the override.
Do insurance companies cover DAW-1 prescriptions?
Yes - but they often require prior authorization. Most Medicare Part D and commercial plans treat DAW-1 prescriptions as non-preferred. The doctor may need to submit clinical documentation to justify the brand. If they don’t, the patient may pay full price.
How do I know if a drug has a narrow therapeutic index?
Check the FDA’s Orange Book. Drugs with an "A" rating are generally substitutable. But for drugs like warfarin, levothyroxine, phenytoin, carbamazepine, and cyclosporine, even if they’re rated "A," many experts still recommend avoiding substitution. Your pharmacy’s clinical guidelines or a drug reference app like Lexicomp will flag these.
Can I use DAW-1 for every prescription to avoid hassle?
No. Using DAW-1 unnecessarily is considered inappropriate override. It drives up costs and undermines efforts to control healthcare spending. Payers may audit your prescribing patterns. If you override too often without clinical justification, you could face scrutiny from insurance companies or state medical boards.
Final Takeaway
Prescriber override isn’t about being difficult. It’s about being precise. For most patients, generics are perfect. For a small group, they’re dangerous. The system works - if you know how to use it. Learn your state’s rules. Fix your EHR. Document clearly. And when in doubt, override. Because when it comes to these drugs, the difference between brand and generic isn’t just dollars. It’s safety.
Write a comment
Your email address will not be published.






8 Comments
Let’s be real - this isn’t about patient safety. It’s about doctors being lazy and not updating their EHR templates. I’ve seen 70-year-old GPs write 'DAW-1' on a napkin and expect the pharmacy to magically interpret it. Meanwhile, the system auto-substitutes because the code isn’t mapped. It’s not the pharmacist’s fault. It’s systemic incompetence. And yeah, I’ve had patients show up with seizures because their levothyroxine got swapped. Fix your damn software, not just your prescriptions.
I’ve worked in community pharmacies for 18 years, and I’ve seen everything. I remember this one elderly woman who came in crying because she’d been switched from brand Synthroid to a generic and started having panic attacks. She said her heart felt like it was gonna explode. We called the doctor, who had literally forgotten to check the box. We called the patient back, gave her the brand, and she cried again - this time from relief. This isn’t about money. It’s about people. A 10% difference in absorption doesn’t sound like much until your mom’s thyroid crashes. I wish more doctors understood that. It’s not just a pill. It’s someone’s stability. Their sleep. Their ability to hold a job. To hug their grandkids without feeling like they’re gonna die. We’re not vending machines. We’re the last line before disaster.
DAW-1 = $$$ 😒
Doctors: 'I'm protecting my patients!'
Reality: 'I'm too lazy to click the right box.' 💸
Man, I get why this is such a mess. I’m not a doc, but I’ve got a kid on phenytoin, and I’ve been down this road. The first time we got the generic, he had a seizure in the shower. Scared the hell out of us. We called the pharmacy, they said 'it was approved.' We called the doctor, he was like 'oh shit, I forgot to check the box.' We fixed it, but man - if I hadn’t caught it, who knows? I just wish the system made it easier. Like, why can’t the EHR just auto-prompt you when you prescribe warfarin or levothyroxine? Why do we still need to know state-by-state rules? That’s 2005 thinking in 2024. We’re all just trying to keep people alive. Let’s make this less of a puzzle and more of a safety net.
Let me break this down in Naija logic: You got a system designed for 1990s paper scripts trying to handle 2024 digital prescriptions across 50 different rulebooks. That’s not healthcare - that’s bureaucratic roulette. And now you want to throw biosimilars into the mix? Bro, we ain’t ready. The Nigerian health system can’t even get antiretrovirals to the right clinic on time, and y’all are arguing over whether 'DAW-1' needs to be handwritten or typed? This ain’t innovation. This is institutional schizophrenia. Someone needs to build a universal override API - not another pamphlet. The FDA’s Orange Book? It’s a Wikipedia page with a seal. It ain’t law. It’s a suggestion with a badge.
They’re using generics to kill us. You think this is about cost? Nah. It’s about the Pharma-Industrial Complex. The FDA is in bed with the generics manufacturers. They say 'therapeutic equivalence' - but they don’t test for long-term bioaccumulation. They don’t test how the fillers affect your gut microbiome over 20 years. The brand-name drugs? They’re made in Germany. The generics? Made in India with cheap dyes and talc. You think your 'safe' generic isn’t loaded with microplastics? I’ve seen the reports. The government doesn’t want you to know. But I do. And if you’re still taking generics for warfarin, you’re playing Russian roulette with your blood. DAW-1 isn’t a loophole - it’s your last defense.
Ah, the sacred ritual of the DAW-1 - a modern-day incantation whispered into the void of EHRs, hoping the algorithm hears the divine truth of the prescriber’s will. We’ve turned medicine into a bureaucratic liturgy where the sacrament of safety is encoded in a single checkbox, and the priesthood - the pharmacists - are left to interpret the runes of state law like medieval monks deciphering a lost gospel. Is this not the apotheosis of late-capitalist healthcare? Where the body becomes a data point, the drug a commodity, and the doctor - the last prophet - must scribble the holy word in the correct dialect, lest the patient be sacrificed on the altar of efficiency. The FDA’s Orange Book? A dusty altar stone. The EHR? A temple built on sand. We are not curing illness. We are optimizing for compliance. And the soul of medicine? Buried under layers of form fields and state-specific syntax.
I’m from India, where generics are the only option for 90% of people. We don’t have brand-name drugs unless you’re rich. But here’s the thing - we don’t have this problem because we don’t have the same patchwork of laws. Pharmacists know what’s equivalent. Doctors trust the system. We don’t have 50 different rules - we have one rule: if it’s on the WHO list, it’s safe. Maybe the U.S. needs less complexity, not more. Not every difference is dangerous. Maybe we’re over-medicalizing what’s just a supply chain issue. I’m not saying no overrides. But maybe we’re scared of generics because we’ve lost trust in the system - not the science.