
When you feel like the room is spinning, you don’t just say you’re dizzy-you say you have vertigo. But if you just feel lightheaded, off-balance, or like you might faint, that’s dizziness. These aren’t the same thing. And confusing them can cost you months-or even years-of unnecessary treatment.
Vertigo Isn’t Just Dizziness With Extra Spin
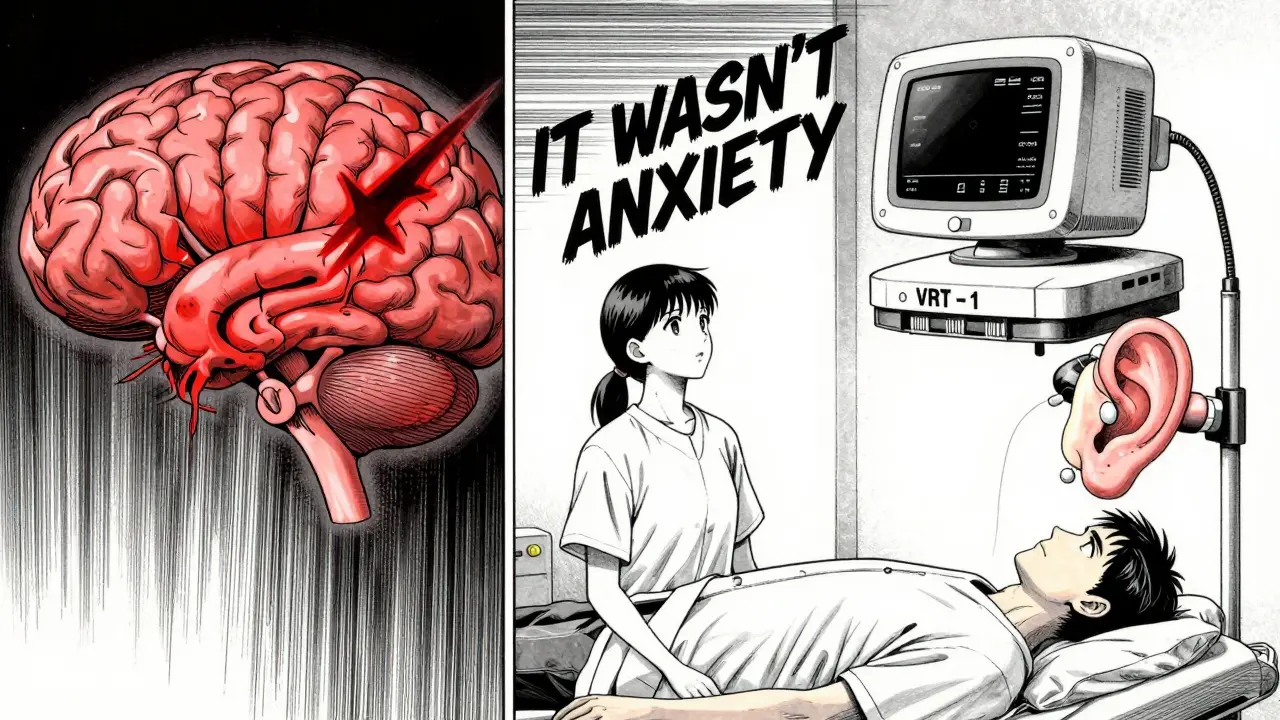
Vertigo is the false sensation that you or your surroundings are moving. It’s not just feeling unsteady. It’s the unmistakable feeling that you’re on a spinning ride, even when you’re lying perfectly still. This isn’t anxiety. It’s not dehydration. It’s your brain getting wrong signals from your inner ear or brainstem.
Dizziness? That’s the umbrella term. It includes feeling faint, woozy, foggy-headed, or unbalanced without any spinning. You might feel like you’re going to pass out when you stand up. Or your legs feel weak. Or your head feels heavy. These are different systems at work-your blood pressure, your blood sugar, your anxiety levels-not your balance organs.
The difference matters because treatment changes completely. If you have vertigo from BPPV (Benign Paroxysmal Positional Vertigo), a 5-minute head maneuver can fix it. If you’re told you just have "dizziness" and get anxiety meds instead? You’ll keep spinning for months.
What’s Actually Causing Your Vertigo?
Most vertigo comes from your inner ear-the vestibular system. It’s like a tiny gyroscope inside your skull, filled with fluid and hair cells that detect movement. When something goes wrong there, your brain gets scrambled signals.
BPPV is the #1 cause. It happens when tiny calcium crystals (otoconia) break loose and float into the wrong part of your ear. Every time you roll over or look up, they shift and trick your brain into thinking you’re spinning. It’s common-up to 30% of vertigo cases-and it’s treatable. The Epley maneuver, done by a trained therapist, repositions those crystals. Success rate? 80-90% after one or two sessions.
Vestibular neuritis is another big one. It’s usually caused by a virus that inflames the nerve connecting your inner ear to your brain. You wake up with intense spinning, nausea, and trouble walking. No hearing loss. Just pure vertigo that lasts days, then slowly fades. Treatment? Rest, anti-nausea meds, and then vestibular rehab to retrain your brain.
Ménière’s disease is less common but more complex. It involves fluid buildup in the inner ear, causing spinning episodes, ringing in the ear, and hearing loss. Episodes can last hours. There’s no cure, but diet changes (low salt), diuretics, and sometimes injections can help control it.
When Vertigo Comes From Your Brain (Not Your Ear)
Not all vertigo is ear-related. About 5-10% comes from the brain. This is called central vertigo. It’s more dangerous-and often missed.
Strokes can cause vertigo. Yes, a stroke in the back of your brain can make you feel like you’re spinning. But unlike BPPV, it won’t get better with head movements. You’ll also have other red flags: trouble walking, slurred speech, double vision, numbness on one side, or sudden severe headache. These aren’t "just dizziness." They’re neurological emergencies.
Vestibular migraine is another sneaky one. You don’t need a headache to have it. Just 5 episodes of spinning lasting 5 minutes to 72 hours, plus nausea, light/sound sensitivity, or a history of migraines. Doctors miss this 30% of the time. Patients are told it’s anxiety or sinusitis. But it’s a brain wiring issue-same as migraines, just affecting balance instead of pain.
Multiple sclerosis can also cause vertigo. It damages the nerves that carry balance signals. If you’re young and get vertigo with vision problems or numbness, it’s worth checking.
Why Dizziness Is a Bigger, Messier Problem
Dizziness doesn’t have one clear source. It’s a symptom with dozens of causes.
Orthostatic hypotension-your blood pressure dropping when you stand-is a major culprit. If your systolic pressure falls 20 mmHg or more, you’ll feel lightheaded. This is common in older adults, diabetics, or people on blood pressure meds.
Anemia and low blood sugar? They make you feel weak, foggy, and faint. No spinning. Just exhaustion and a sense that you’re about to pass out.
Medications are huge. Antidepressants, blood pressure pills, sedatives, even some antibiotics can cause dizziness as a side effect. If you started a new drug and then felt off, it’s likely the cause.
And then there’s anxiety. Chronic dizziness can become a loop: you feel dizzy → you worry you’re having a stroke → you panic → your breathing changes → you feel more dizzy. This is called persistent postural-perceptual dizziness (PPPD). It’s real. It’s not "all in your head." It’s your nervous system stuck in overdrive.
How Doctors Tell Them Apart
There’s no single test. Diagnosis is about patterns.
Doctors look for nystagmus-fast, involuntary eye movements. If your eyes jerk in a specific pattern when you move your head, it’s likely peripheral vertigo (ear-related). If the eye movements are irregular, don’t follow the rules, or happen when you’re still, it’s probably central (brain-related).
VNG (videonystagmography) is the gold standard test. Tiny cameras track your eye movements as you follow lights or get cold/warm air blown in your ears. It shows if your inner ear is working right. It’s 95% accurate for detecting inner ear problems.
Head impulse testing is simpler. The doctor quickly moves your head side to side while you stare at their nose. If your eyes jerk away and then snap back, your inner ear nerve isn’t firing right. That’s vestibular neuritis.
For central causes, an MRI is needed. But only if you have red flags: new weakness, trouble speaking, double vision, or loss of coordination. Most vertigo cases don’t need imaging. But if you have them, don’t delay.
What Actually Works-And What Doesn’t
For BPPV: The Epley maneuver. Done right, it works in minutes. Done wrong? It does nothing. Find a physical therapist trained in vestibular rehab-not just any PT.
For vestibular neuritis: Rest for a few days, then start moving. Stay active. Your brain needs to relearn balance. Vestibular rehab exercises-like standing on one foot, walking while turning your head, or focusing on a target while moving-help rebuild your balance system. Most people improve in 6-8 weeks.
For vestibular migraine: Avoid triggers (stress, caffeine, skipped meals). Some meds like beta-blockers or topiramate help prevent attacks. Anti-nausea meds during episodes.
For dizziness from low blood pressure: Drink more water. Stand up slowly. Wear compression socks. Check your meds with your doctor.
For PPPD: Cognitive behavioral therapy (CBT) combined with vestibular rehab is the only thing that works long-term. Antidepressants alone? They don’t fix the balance issue. They just numb the anxiety.
And here’s the truth: Many people with dizziness get treated for anxiety because doctors don’t know how to test for vestibular problems. Only 12% of primary care doctors feel confident diagnosing vertigo. That’s why so many people wait 8 months or more for answers.
What to Do If You’re Still Struggling
If you’ve been told it’s "stress" or "aging" and you’re still dizzy or spinning:
- Ask for a referral to a vestibular specialist or neuro-otologist.
- Request a VNG test if you haven’t had one.
- Keep a symptom diary: When does it happen? What were you doing? How long does it last? Any triggers?
- Don’t accept "it’s all in your head." If your symptoms are real, there’s a physical cause.
- Find a vestibular rehab therapist. Look for someone certified by the Vestibular Disorders Association (VEDA).
One woman in Manchester, after 18 months of being told it was anxiety, finally got a VNG test. It showed BPPV. One Epley maneuver. Gone. She said: "I didn’t know I could feel normal again."
What’s Changing in 2026
AI is now helping diagnose vertigo faster. Johns Hopkins developed an algorithm that analyzes eye movement videos and tells doctors if it’s a stroke or BPPV-with 85% accuracy. It’s not everywhere yet, but it’s coming.
There’s also new FDA-approved devices for vestibular rehab. One, called VRT-1, guides patients through home exercises with real-time feedback. It’s like a Fitbit for your balance.
And research is moving toward regenerating inner ear hair cells. Stanford started human trials in 2023. If it works, we could one day cure permanent vestibular damage.
But right now, the biggest gap isn’t technology. It’s awareness. Most people still think dizziness is normal. It’s not. And vertigo isn’t just bad luck. It’s a signal. Listen to it.
Is vertigo the same as dizziness?
No. Dizziness is a general feeling of lightheadedness, unsteadiness, or faintness. Vertigo is a specific type of dizziness where you feel like you or your surroundings are spinning. Vertigo always involves a motion illusion; dizziness does not.
Can anxiety cause vertigo?
Anxiety doesn’t cause true vertigo, but it can trigger or worsen dizziness. Chronic anxiety can lead to PPPD (persistent postural-perceptual dizziness), where the brain becomes hypersensitive to balance signals. This feels like vertigo but has no inner ear damage. Treatment requires vestibular rehab and CBT-not just anti-anxiety meds.
How do I know if my vertigo is from my ear or my brain?
Ear-related vertigo (peripheral) usually comes with nausea, vomiting, and lasts minutes to hours. It’s often triggered by head movement. Brain-related vertigo (central) often comes with other neurological symptoms: double vision, slurred speech, weakness, numbness, or trouble walking. If you have these, get an MRI immediately. Also, central vertigo doesn’t improve with the Epley maneuver.
Can BPPV come back after treatment?
Yes. About 30-50% of people with BPPV have a recurrence within five years. It’s not dangerous, but it’s annoying. If it returns, repeat the Epley maneuver. Some people learn to do it at home after being shown once. Keeping your head upright for 48 hours after treatment helps prevent recurrence.
What’s the best test for vertigo?
Videonystagmography (VNG) is the most accurate. It records your eye movements during different head and position changes to check inner ear function. Head impulse testing is simpler and often done in clinics. For suspected brain causes, an MRI is needed. Blood tests or X-rays won’t help-this is a neurological balance issue, not an infection or structural problem.
When should I go to the ER for dizziness?
Go to the ER if you have vertigo with any of these: sudden severe headache, double vision, slurred speech, weakness or numbness on one side, trouble walking, loss of consciousness, or chest pain. These could signal a stroke or other serious neurological event. Don’t wait. Even if you think it’s "just dizziness," these red flags mean you need urgent care.
Is vestibular rehab worth it?
Yes-especially if your dizziness or vertigo lasts more than a few weeks. Studies show 89% of people improve with vestibular rehab. It’s not magic. You have to do the exercises daily for 6-8 weeks. But it retrains your brain to rely on other balance signals when your inner ear is damaged. It works for BPPV, neuritis, PPPD, and even after concussions.
Write a comment
Your email address will not be published.




1 Comments
Okay but like… if you’re not a neuro-otologist, you’re just guessing. I read this and now I’m convinced my coffee is causing vertigo. My barista should be held accountable. I’ve been spinning since Tuesday. I demand a refund and a VNG test.
Also, who let a non-doctor write this? This is worse than my cousin’s TikTok medical advice.
And why is there an AI thing in 2026? That’s not even next year. Are we time-traveling now? I’m confused.
Also, I tried the Epley maneuver and now my cat is spinning. Not sure if that’s progress.
Someone call the FDA. This is a public health crisis.