Every time you pick up a prescription, you’re handed a small piece of paper that could mean the difference between healing and harm. But most people glance at it, tuck it in a bag, and never really read what’s written there. That’s dangerous. Prescription labels aren’t just bureaucratic paperwork-they’re your personal safety guide. And if you don’t understand them, you’re guessing your way through your own treatment.
The Patient Name: Your First Line of Defense
Your name is printed right at the top of the label-not because it looks nice, but because it’s a life-saving check. Every year in the U.S., over 1.5 million medication errors happen because someone gets the wrong drug. Most of those are mix-ups between patients. Your name on the label stops that. If you see someone else’s name, don’t take it. Even if the pill looks right, it’s not yours. Pharmacists are trained to verify this, but you’re the last line of defense. Always double-check it before walking out the door.
Medication Name: Brand vs. Generic
You’ll see two names here: one big, one small. The big one is the brand name-like Abstral. The smaller one underneath is the generic name-fentanyl. The brand name is what the drug company calls it. The generic name is the actual chemical. They’re the same thing. But knowing the generic name matters. If your insurance won’t cover the brand, your pharmacist can switch you to the generic without changing how the medicine works. It’s also how doctors talk to each other. If you’re seeing a new provider, telling them you’re on "fentanyl" instead of "Abstral" helps them understand your treatment faster.
Dosage Strength: How Much Is Really in There?
This part tells you how strong each pill, capsule, or milliliter of liquid is. For example: "100 mcg" means 100 micrograms of the active drug. That’s not the same as "100 mg"-micrograms are 1,000 times smaller. Mix those up, and you could overdose. The dosage is always listed with the unit: mg, mcg, mL, IU. Never assume. If you’re unsure, ask your pharmacist to show you the difference between 5 mg and 50 mg. A single decimal point error has killed people. This is why your label must be crystal clear.
Directions for Use: What, When, and How
"Take one tablet by mouth every 4 hours as needed for pain" sounds simple. But what does "as needed" really mean? Does it mean only when the pain is sharp, or anytime you feel it coming? Does "every 4 hours" mean exactly every 4 hours, even if you’re sleeping? The label doesn’t always spell it out. That’s why your pharmacist should explain it. But if they don’t, here’s what to look for:
- "Take with food" means don’t swallow it on an empty stomach-it could upset your gut.
- "Take on an empty stomach" means wait at least an hour before or after eating.
- "Take at bedtime" means right before you sleep, not at 8 p.m. if you’re going to bed at midnight.
- "PRN" means "as needed," but only if your doctor said it’s okay to use it that way.
Abbreviations like "tid" or "q6h" are outdated and confusing. The FDA and USP now recommend spelling everything out: "three times a day," "every 6 hours." If your label still uses shorthand, ask for a clearer version. You have the right to understand your own meds.
Expiration Date: When It’s No Longer Safe
That date on the label isn’t just a suggestion. It’s the last day the manufacturer guarantees the drug will work as intended. After that, it might not kill you-but it might not help either. Some pills lose potency fast. Antibiotics, insulin, and liquid medicines degrade quickly. The FDA says most pills are stable for 12 to 18 months after being filled. But if your bottle says "exp. 06/2025," and today is January 2026, you’ve got a few months left. Still, don’t wait. If the pill looks cracked, discolored, or smells weird, toss it. Never take expired medicine, even if it looks fine.
Prescription Number: Your Medication’s ID
This is a unique number assigned to your prescription when it was filled. It’s not your insurance ID or your doctor’s number. It’s the pharmacy’s way of tracking your specific order. You need this number if you call for a refill. If you lose your bottle and need a new one, the pharmacist will ask for it. If you’re switching pharmacies, you’ll need to give them this number so they can transfer your prescription. Keep it somewhere safe-maybe write it in your phone notes. Don’t ignore it. It’s the key to getting your meds without delays.
Pharmacy and Prescriber Info: Who to Call When Something’s Wrong
Look for the pharmacy’s name, phone number, and address. This isn’t just for show. If you have side effects, if the pill looks different than last time, or if you’re confused about the instructions-call them. Don’t call your doctor first. Your pharmacist is the expert on the medication itself. They know how it interacts with other drugs you take. They also know if there’s a recall. And they’re required to answer your questions. The prescriber’s name is there too. That’s your doctor or nurse practitioner who ordered it. If you’re unsure why you’re taking it, ask your pharmacist. They can contact your doctor to confirm the reason.
Physical Description: What Your Pill Should Look Like
"White, round, film-coated tablet, imprinted with 'A123'"-this part tells you what your medicine should actually look like. It’s there so you can spot a mistake. Maybe your pill was blue last time, and now it’s yellow. That’s not normal. Maybe the imprint is different. That could mean you got a different brand or a counterfeit. Even if the name and dosage match, if the pill looks off, don’t take it. Call your pharmacy. This is why some pharmacies now include a photo on the label. The FDA encourages it. If yours doesn’t, ask for one.
National Drug Code (NDC): The Universal Barcode
You’ll see a long string of numbers-usually 10 or 11 digits. That’s the NDC. It’s like a fingerprint for your drug. It tells you exactly which company made it, what the product is, and what size bottle you got. It’s not meant for you to memorize, but it’s there for the system. If you’re ever in the hospital or need to report a side effect, they’ll ask for it. If you’re using a medication app, you can scan it. It’s also how the government tracks drug shortages and recalls. If you’re curious, you can look it up online using the FDA’s NDC directory. But you don’t need to. Just know it’s there to make sure you’re getting the right drug, every time.

Storage Instructions: Keep It Right, Keep It Safe
"Store at room temperature" sounds vague. What’s room temperature? The FDA says 68°F to 77°F. That’s not your bathroom cabinet, which gets steamy. It’s not your car, which gets too hot in summer. Some meds need refrigeration. Others need to stay dry. If your label says "protect from moisture," don’t leave it in the medicine cabinet. Keep it in a cool, dry drawer. Insulin? Refrigerate it until you open it. Then keep it at room temp for up to 28 days. If you store it wrong, the medicine breaks down. You won’t know until it doesn’t work-and by then, it’s too late.
Warnings: The Red Flags You Can’t Ignore
This is the most important part-and the most ignored. Warnings tell you when not to take the drug. "Do not use if you have liver disease." "May cause drowsiness-do not operate machinery." "Avoid alcohol." These aren’t suggestions. They’re rules. Some warnings are so serious they’re printed in a box at the top of the professional label. Those are called "Boxed Warnings." They mean the drug can cause death or permanent injury. If your label has one, you need to know what it says. Ask your pharmacist to explain it. If you’re pregnant, breastfeeding, or over 65, some warnings apply extra hard to you. Don’t assume it’s fine because you’ve taken it before. Your body changes. So do your risks.
The Missing Piece: Why You’re Taking This
Most labels still don’t say why you’re taking the drug. Is it for high blood pressure? Depression? A skin infection? That’s a huge gap. A 2020 FDA study found that 78% of patients take their meds wrong because they don’t know the reason. They think it’s for headaches, but it’s actually for migraines. They think it’s a painkiller, but it’s an antidepressant. That’s why USP is pushing for all labels to include the indication by 2025. Some pharmacies already do. If yours doesn’t, ask for it. Write it on the label yourself. "For anxiety" or "for thyroid"-just add it. It’s not on the official label, but it’s the most important thing you need to know.
What to Do When You’re Still Confused
Even with all this, you might still have questions. That’s normal. Don’t feel bad. Here’s what to do next:
- Call your pharmacy. They have to answer your questions. Don’t wait until your next refill.
- Ask your pharmacist to explain the label using the "5 Questions" method: What’s the name? What’s it for? How do I take it? What if I miss a dose? What side effects should I watch for?
- Use the "teach-back" method: After they explain, say it back to them in your own words. If they nod, you got it. If they correct you, ask again.
- If you’re still unsure, ask your doctor to write a simple note on the prescription. Many will.
Medication errors kill about 7,000 people in the U.S. every year. Most of those are preventable. You don’t need to be a doctor to keep yourself safe. You just need to read the label-and ask when you don’t understand.
What should I do if my prescription label looks different from last time?
Don’t take it. Even if the name and dosage match, a change in color, shape, size, or imprint could mean you got a different brand or a counterfeit. Call your pharmacy immediately. They’ll check if it’s a legitimate change or an error. Most of the time, it’s just a different manufacturer-but you need to confirm it’s safe.
Can I take my medication after the expiration date?
It’s not recommended. Most pills lose potency over time, especially liquids, insulin, and antibiotics. Taking expired medicine might not help, and in rare cases, it can break down into harmful substances. The FDA says you should dispose of expired drugs properly. If you’re in a pinch and have no other option, consult your pharmacist-they can tell you if it’s safe for that specific drug.
Why doesn’t my label say why I’m taking this medicine?
Many pharmacies still don’t include the indication (reason for use) because their systems don’t support it. But it’s becoming standard. The USP plans to require it by 2025. Until then, ask your pharmacist or doctor to write it down. You can even write it on the bottle yourself. Knowing why you’re taking a drug reduces errors by over 50%, according to the Institute for Safe Medication Practices.
What’s the difference between a brand-name and generic drug?
They contain the same active ingredient and work the same way. The brand name is what the company originally developed it under. The generic is the same medicine sold under its chemical name. Generics are cheaper and FDA-approved to be just as safe and effective. The only differences might be in the inactive ingredients (like fillers), which rarely affect how the drug works.
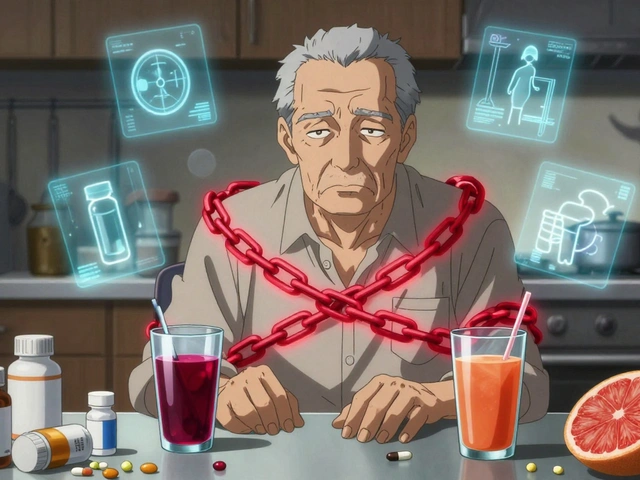
How do I know if my medication is interacting with something else?
Your pharmacist should check for interactions when filling your prescription. But you should still tell them everything you take-including vitamins, supplements, and over-the-counter drugs. Some common ones like St. John’s Wort or grapefruit juice can seriously interfere with medications. If you start a new drug, ask: "Will this interact with anything else I’m taking?" Write down the answer.
Next Steps: Take Control of Your Medications
Start today. Grab your next prescription label. Read it out loud. Circle the parts you don’t understand. Call your pharmacy. Ask them to explain it like you’re 12 years old. Don’t be embarrassed. Every person who’s ever taken medicine has been confused by a label. The goal isn’t to memorize every detail. It’s to know enough to spot a mistake before it hurts you. You’re not just a patient-you’re the most important part of your own care team. And your label? It’s your tool. Use it.
Write a comment
Your email address will not be published.




1 Comments
Wow, someone actually wrote a guide that doesn’t sound like it was drafted by a robot hired by Big Pharma. Finally, someone gets it-labels aren’t filler, they’re your armor. I once took someone else’s blood pressure med because I was in a rush and didn’t check the name. Ended up in the ER with a heart rate of 48. Don’t be me.