
Why Antiplatelet Drugs Are Necessary - and Dangerous
Every year, millions of people take antiplatelet medications like aspirin, clopidogrel, prasugrel, and ticagrelor to prevent heart attacks and strokes. These drugs stop blood clots from forming by blocking platelets - the tiny cells in your blood that stick together to seal cuts. But that same power comes with a serious downside: they make you more likely to bleed, especially in your stomach and intestines.
It’s not a small risk. About 1% of people on these drugs will have a noticeable gastrointestinal bleed within the first month. For those on dual therapy - say, aspirin plus clopidogrel - that risk jumps by 30% to 50%. And over time, up to 40% of aspirin users and 50% of clopidogrel users develop ongoing damage to their stomach lining, even if they feel fine.
Many assume enteric-coated aspirin is safer. It’s not. That coating just delays when the pill dissolves - it doesn’t stop the drug from thinning your blood. The real danger isn’t just the pill irritating your stomach. It’s that your platelets can’t do their job of stopping small leaks in your gut. Those tiny bleeds add up. Over months, they can turn into ulcers. And once an ulcer forms, the risk of a major, life-threatening bleed skyrockets.
Which Antiplatelet Drug Is Riskiest for Your Stomach?
Not all antiplatelet drugs are created equal when it comes to gut damage. Aspirin has been around for decades, and we know its risks well. But newer drugs like clopidogrel, prasugrel, and ticagrelor - while better at preventing heart events - are harder on your digestive system.
Studies show clopidogrel is 80% more likely than aspirin to cause serious gastrointestinal injury. Why? It doesn’t just block platelets. It also stops them from releasing growth factors that help heal stomach ulcers. So even if you have a small sore, your body can’t fix it.
Prasugrel and ticagrelor are even stronger. In the PLATO trial, ticagrelor raised the risk of GI bleeding by 30% compared to clopidogrel. That’s why doctors often choose clopidogrel for patients with a history of stomach problems - not because it’s safe, but because it’s the least bad option.
And here’s something many don’t realize: if you’ve had a prior GI bleed, aspirin alone is the safest choice for long-term heart protection. Stopping all antiplatelet drugs after a bleed increases your risk of dying from a heart attack by 25%. The answer isn’t to quit - it’s to protect your gut while keeping your heart safe.
How Proton Pump Inhibitors (PPIs) Help - and What They Don’t Fix
If you’re on antiplatelet therapy, especially with risk factors like age over 65, past ulcers, or use of NSAIDs like ibuprofen, you almost certainly need a proton pump inhibitor (PPI). Drugs like esomeprazole, omeprazole, and pantoprazole reduce stomach acid, giving your lining time to heal.
Studies show that when patients on clopidogrel take esomeprazole 40mg daily, 92% of ulcers heal within 8 weeks. That’s a huge win. For people with a history of bleeding, guidelines now recommend staying on a PPI indefinitely - not just until the ulcer heals, but for life.
But PPIs aren’t magic. They don’t fix the platelet problem. They only reduce acid. That means if you’re on a high-risk antiplatelet drug like ticagrelor, even a PPI won’t eliminate your bleeding risk. It just lowers it.
And there’s a catch. For years, doctors worried that PPIs might weaken clopidogrel’s effect. The theory was that PPIs block an enzyme (CYP2C19) that clopidogrel needs to become active. But the real-world impact? It’s small. The FDA says the interaction is uncertain. One large study found a 20-30% higher chance of heart events in people taking both - but that could be because those patients were sicker to begin with. Most experts now agree: if you need a PPI, take it. Don’t skip it out of fear.
What to Do If You Start Bleeding
If you notice black, tarry stools, vomit blood, or feel dizzy and weak, get help immediately. Don’t wait. But here’s what you shouldn’t do: stop your antiplatelet drug on your own.
For aspirin, guidelines are clear: keep taking it. Stopping aspirin during a GI bleed doesn’t help stop the bleeding - and it raises your chance of dying from a heart attack. The same goes for most patients on dual therapy. In fact, a 2017 Lancet study showed that stopping antiplatelet drugs during bleeding led to 25% higher mortality.
For clopidogrel, prasugrel, or ticagrelor, the advice is different. Hold the drug for 5-7 days if bleeding is active and severe. But restart as soon as your doctor says it’s safe. Delaying too long increases your risk of stent clotting - and that can kill you. One Reddit thread from 2023 shared three cases where patients stopped clopidogrel after stomach pain, then had a heart attack within 30 days.
And don’t let anyone give you a platelet transfusion unless it’s absolutely necessary. A small study found transfused patients had 27% mortality compared to 12% in those who didn’t get them. Platelets can make clots worse in this situation.
Who Needs the Most Protection?
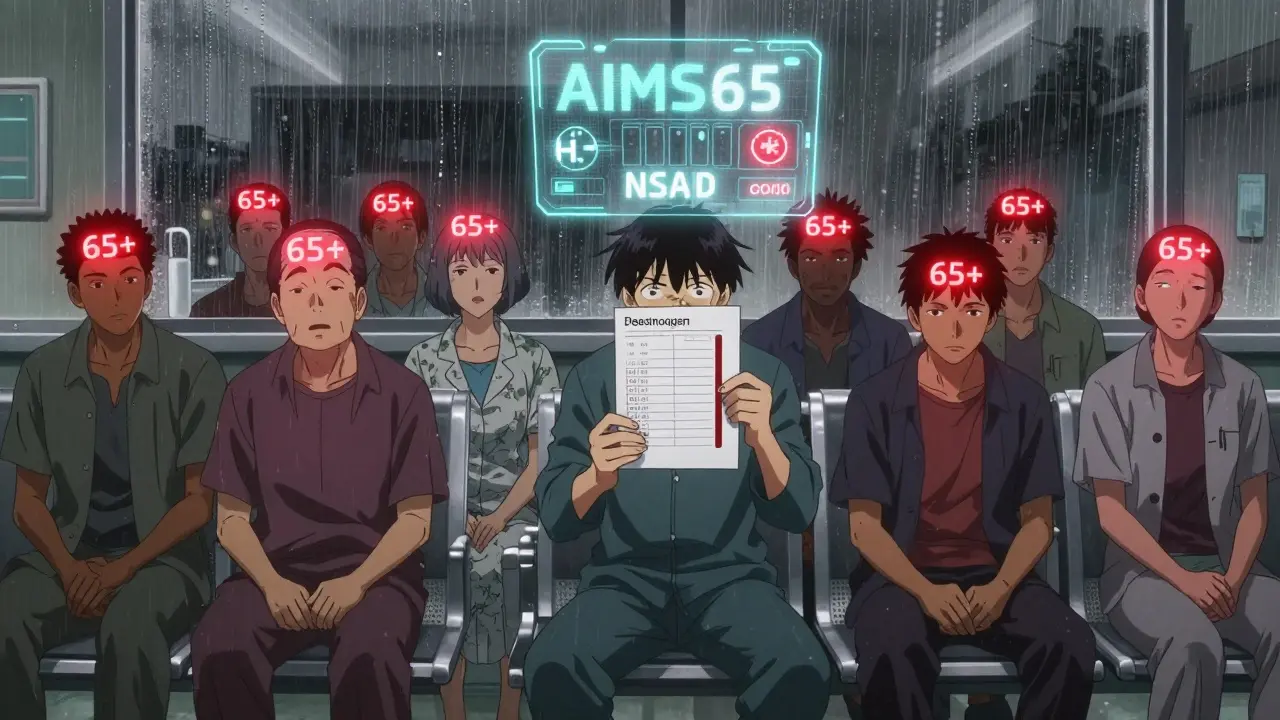
You don’t all need the same level of care. Doctors use tools like the AIMS65 score to figure out who’s at highest risk:
- A - Albumin below 3.0 g/dL
- I - INR above 1.5
- M - Mental status change
- S - Systolic blood pressure below 90
- 65 - Age 65 or older
If you score 2 or higher, you’re in the high-risk group. That means you need aggressive protection: IV PPIs at first, then daily oral doses, and likely lifelong use.
Other red flags? You’re over 65. You take NSAIDs. You’ve had a prior ulcer or GI bleed. You have H. pylori infection. You’re on multiple blood thinners. If any of these apply to you, you should be on a PPI - even if you’ve never bled.
And here’s a surprise: about 1 in 5 people who take PPIs long-term develop side effects - joint pain, diarrhea, low magnesium, or even kidney issues. If you’re one of them, talk to your doctor. There are alternatives like H2 blockers (famotidine), though they’re not as strong. Never stop a PPI cold turkey - you can get rebound acid.
The Future: Safer Drugs and Personalized Care
Drug companies are working on new antiplatelet agents that don’t wreck your stomach. One called selatogrel, currently in late-stage trials, shows 35% less gut injury than ticagrelor in early studies. That’s promising.
Another frontier is genetic testing. About 30% of people have a variant in the CYP2C19 gene that makes clopidogrel less effective. For them, switching to ticagrelor or prasugrel might actually be safer - not just because it works better, but because they don’t need to rely on a drug their body can’t activate properly. That could reduce the need for high-dose PPIs in some patients.
Researchers are also looking at blood tests for pepsinogen and gastrin-17 - markers that show how damaged your stomach lining is. In five years, you might get a simple blood test before starting antiplatelet therapy to see if you’re a high-risk candidate for bleeding. Then, your doctor can pick the right drug and the right protection - tailored just for you.
Bottom Line: Don’t Fear the Drug - Manage the Risk
Antiplatelet drugs save lives. But they’re not harmless. The key isn’t to avoid them - it’s to use them smartly. If you’re on one, ask your doctor: Do I need a PPI? Am I on the safest option for my risk level? What should I do if I bleed?
Don’t stop your meds because you’re scared. Talk to your doctor. Get tested for H. pylori. Avoid NSAIDs. Stick to your PPI. And remember: your heart needs these drugs more than your stomach needs to be completely free of risk. The goal isn’t zero bleeding - it’s minimizing risk while keeping your heart protected.
Write a comment
Your email address will not be published.






11 Comments
I've been on clopidogrel for three years and never realized my stomach lining was slowly deteriorating. No symptoms, no warning. Just a routine endoscopy last month showed early ulcers. PPI saved me.
This is exactly why I stopped taking aspirin without consulting my doctor after I started passing black stools. I didn't know stopping could be more dangerous than continuing. Learned the hard way.
The FDA's stance on PPI-clopidogrel interaction is a joke. They ignore real-world data because drug companies fund their studies. You think they care if you bleed or have a heart attack? No. They care about profits.
I've seen too many patients self-discontinue antiplatelets after reading Reddit posts like this one. You're not a doctor. You're not a researcher. You're a person with a Google account and a panic attack. Stop making life-or-death decisions based on anecdotes.
In India, we don't have easy access to PPIs or genetic testing. Many just take aspirin with milk and hope. It's not ideal, but it's survival. The real issue isn't the drug-it's the system that makes you choose between heart and gut because you can't afford both protections.
If you're over 65 and on dual therapy you need a PPI period. No debate. No exceptions. Your stomach doesn't heal like it used to and your platelets are already running on fumes. Don't wait for a bleed to start protecting yourself
I got my CYP2C19 tested last year. Turns out I'm a poor metabolizer. My cardiologist switched me from clopidogrel to ticagrelor and my stomach stopped hurting. No PPI needed. Genetic testing isn't luxury-it's necessity.
The notion that enteric-coated aspirin is safer is a pharmaceutical myth perpetuated by marketing departments. The pharmacodynamics remain unchanged: irreversible COX-1 inhibition, reduced mucosal defense, and microvascular leakage. The coating is a placebo for the anxious.
I was terrified to start a PPI after reading about bone density loss and kidney risks. But my GI doc said: 'You can fix a weak kidney. You can't fix a dead heart.' So I took it. Still taking it. And I'm alive.
They're hiding the truth. PPIs are linked to dementia. Platelet drugs cause cancer. The whole system is rigged. Why do you think they push PPIs so hard? Because they make more money from lifelong prescriptions than they do from saving lives. Wake up.
As a physician who has managed over 200 patients on antiplatelet therapy, I can confirm: the most critical intervention is not the drug choice, but the patient education. The majority of adverse events stem from misinformation, not medication failure. Knowledge is the true prophylaxis.