
When your lungs start to stiffen and scar, breathing becomes harder-not just when you’re running, but even when you’re sitting still. This isn’t just aging. It’s interstitial lung disease, a group of over 200 conditions where the tissue around your air sacs slowly turns to scar tissue, making it impossible for oxygen to get into your blood the way it should. Unlike a cold or pneumonia, this doesn’t go away. Once the scarring happens, it’s permanent. But catching it early can change everything.
What Exactly Is Happening in Your Lungs?
Your lungs aren’t just bags of air. Inside them, tiny air sacs called alveoli are surrounded by a thin layer of tissue-the interstitium. In healthy lungs, this layer is less than 0.1mm thick. In interstitial lung disease (ILD), it thickens to 1mm or more. That’s like putting a blanket over your air sacs. Oxygen can’t pass through easily. Your blood doesn’t get enough of it. Your body knows something’s wrong. You feel out of breath, even when you haven’t moved. This scarring doesn’t happen overnight. It creeps in. At first, you might just feel tired after walking up the stairs. Then, you stop going for walks. You notice a dry cough that won’t quit. Your fingers start to look rounded at the tips-a sign called clubbing. By the time you see your doctor, the damage is often already advanced. Nearly 80% of people with ILD are misdiagnosed at first. Many are told it’s asthma, or just getting older.The Most Common Type: Idiopathic Pulmonary Fibrosis
About one in four ILD cases is idiopathic pulmonary fibrosis, or IPF. That means no clear cause-no job exposure, no autoimmune disease, no drug trigger. Just scarring. It’s the most aggressive form. Without treatment, most people live only 3 to 5 years after diagnosis. But with the right drugs, that timeline can stretch. Two medications-pirfenidone and nintedanib-are now standard. They don’t cure IPF, but they slow the scarring down by about half over a year. Pirfenidone (Esbriet®) is taken as three pills a day. Side effects? Sun sensitivity-so you can’t sit outside without protection-and stomach upset. Nintedanib (Ofev®) is taken twice daily. It causes diarrhea in more than half of users. Both cost over $9,000 a month in the U.S., though insurance often covers them. In the UK, these drugs are available through the NHS, but access can vary by region.Not All ILD Is the Same
ILD isn’t one disease. It’s a family. And each member behaves differently.- Connective tissue disease-associated ILD (like from rheumatoid arthritis or scleroderma) often progresses slower. Some people live 10+ years with proper treatment.
- Sarcoidosis affects 1 in 7 ILD cases. In 60-70% of people, it clears up on its own within two years.
- Drug-induced ILD can reverse if you stop the medicine-antibiotics like nitrofurantoin, chemotherapy drugs, or even some heart medications can trigger it.
- Asbestosis comes from long-term exposure to asbestos. It progresses slowly-about 100-150mL of lung function lost per year-but it’s permanent.
- Acute interstitial pneumonitis is rare but deadly. Half of patients die within three months, even in intensive care.
How Doctors Diagnose It
There’s no single blood test for ILD. Diagnosis takes time-on average, 11 months from first symptom to confirmed diagnosis. That’s because it’s easy to miss. The gold standard is a high-resolution CT scan (HRCT), done with 1mm slices. It shows the pattern of scarring. But even expert radiologists miss early signs 20% of the time. That’s why most hospitals now use a multidisciplinary team-a pulmonologist, a radiologist, and a pathologist-reviewing the scan together. If the picture is unclear, they may take a small lung biopsy. Pulmonary function tests also help. A drop in FVC (forced vital capacity) by more than 10% in six months is a red flag. DLCO (diffusing capacity) falling by over 30% means oxygen transfer is seriously impaired. The 6-minute walk test is simple but telling: if you can’t walk more than 350 meters without stopping, your risk of dying in the next year doubles.Treatment Beyond Drugs
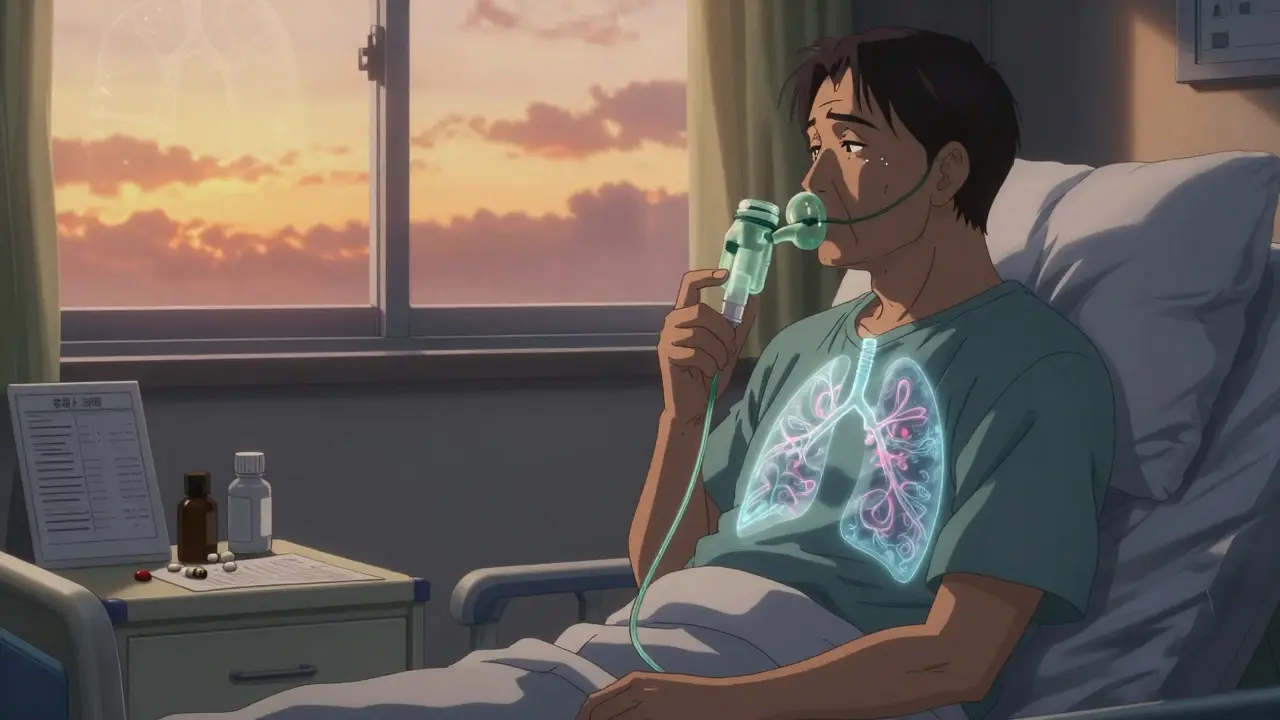
Medications are only part of the story. Pulmonary rehabilitation is just as important. It’s not just exercise-it’s training your body to use less oxygen. You learn breathing techniques, pacing yourself, energy-saving moves. Most programs last 8 to 12 weeks, with two to three sessions per week. People who complete them walk 45 to 60 meters farther on the 6-minute test. Their anxiety drops. They sleep better. They feel less alone. Oxygen therapy becomes necessary when your resting oxygen saturation drops below 88%. For many with IPF, that happens within two years. Portable oxygen concentrators let people leave the house again. But managing the tubing, refilling tanks, and avoiding fire hazards adds a heavy burden. One study found caregivers spend over 20 hours a week helping with oxygen equipment.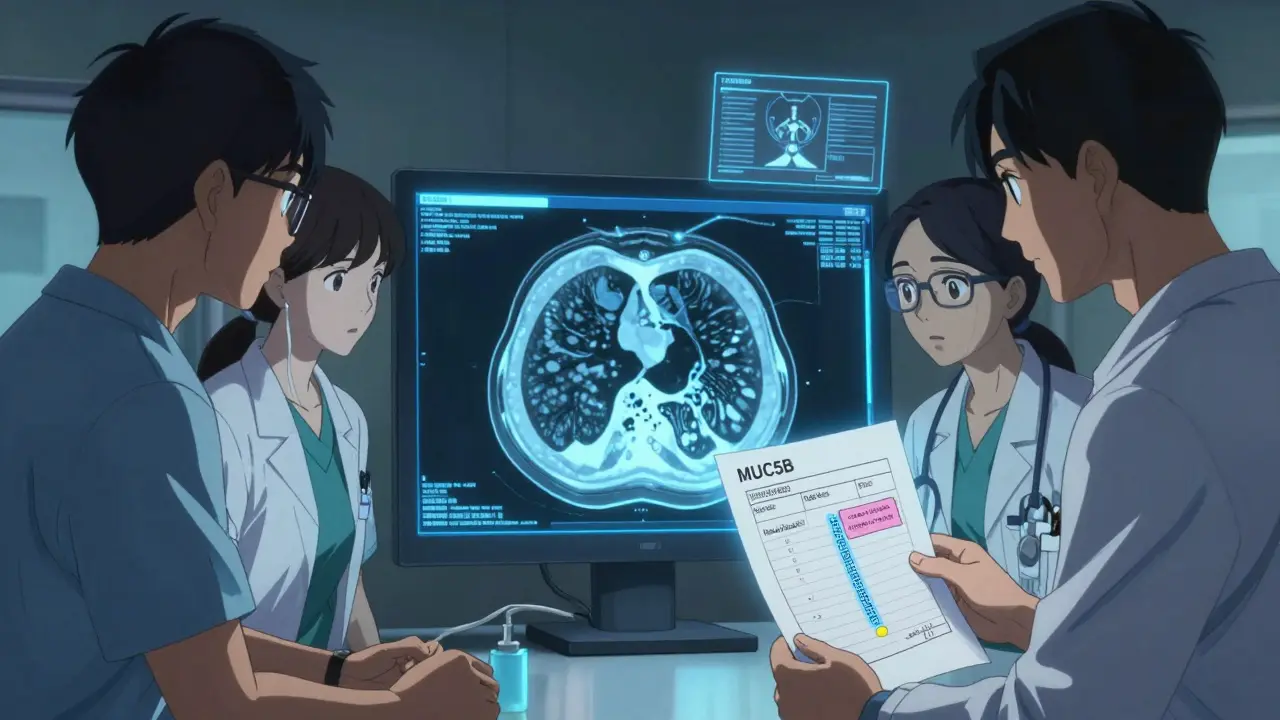
What’s New in 2025?
The last big breakthrough was in 2014. But 2023 brought the first new drug in nearly a decade: zampilodib. It targets a different pathway than pirfenidone or nintedanib. In trials, it cut lung function decline by 48% compared to placebo. It’s now approved in the U.S. and under review in Europe. AI is changing diagnosis too. Mayo Clinic’s new AI tool looks at CT scans and spots ILD patterns with 92% accuracy-better than most radiologists. It can tell the difference between IPF and other types faster, helping patients get the right treatment sooner. Blood tests are getting smarter. Testing for the MUC5B gene variant now helps predict who’s likely to develop aggressive IPF. If you have it, your doctor might start treatment earlier-even before symptoms get bad.What You Can Do Now
If you’ve been told you have ILD, or if you’re struggling with unexplained breathlessness:- Get a high-resolution CT scan. Don’t accept a regular chest X-ray as enough.
- Ask for a multidisciplinary team review. If your hospital doesn’t have one, ask to be referred to a specialty ILD center.
- Start pulmonary rehab-even if you feel too tired. The first week is hard, but it gets easier.
- Stop smoking. If you’ve never smoked, avoid secondhand smoke. Exposure increases risk.
- Get vaccinated. Flu, pneumonia, and COVID-19 can trigger deadly flare-ups in ILD patients.
- Join a support group. People who talk with others who have ILD report less anxiety and better coping.
Hope Is Real-But Time Matters
There’s no magic cure yet. But the tide is turning. Five years ago, many doctors thought ILD was untreatable. Now, we have drugs that slow it. We have tools that catch it earlier. We have programs that help people live better, longer. The key is not waiting. If you’re breathing harder than you used to, don’t brush it off. Don’t let someone tell you it’s just age. Get checked. Push for a CT scan. Ask about ILD. Early action doesn’t guarantee a cure-but it gives you the best shot at keeping your life.Can interstitial lung disease be cured?
No, the scarring in interstitial lung disease is permanent. But treatments like pirfenidone and nintedanib can slow the progression significantly. Pulmonary rehab, oxygen therapy, and lifestyle changes help manage symptoms and improve quality of life. Early diagnosis is the best way to preserve lung function for as long as possible.
How long do people live with ILD?
It depends on the type. Idiopathic pulmonary fibrosis (IPF) has a median survival of 3 to 5 years without treatment. With antifibrotic drugs, many live 5 to 7 years or longer. Other forms, like sarcoidosis or connective tissue-related ILD, may progress slowly and allow people to live 10+ years. Acute forms can be fatal within months. Prognosis is tied to how early treatment starts and how fast lung function declines.
What are the side effects of ILD medications?
Pirfenidone often causes nausea, loss of appetite, and sun sensitivity-patients must avoid direct sunlight and use high-SPF sunscreen. Nintedanib commonly causes diarrhea, which may require dose reduction or anti-diarrheal meds. Both drugs require monthly liver function tests. Side effects are manageable for most, but about 15% of patients stop taking them due to intolerance.
Is oxygen therapy permanent for ILD patients?
For many with advanced ILD, especially IPF, oxygen therapy becomes a long-term need. About 55% of IPF patients require supplemental oxygen within two years of diagnosis. It’s not always 24/7-many use it only during activity or sleep. But as the disease progresses, most will need it continuously. Portable devices now allow people to stay active while on oxygen.
Can lifestyle changes help with ILD?
Yes. Quitting smoking is critical-even if you’ve smoked for decades. Avoiding air pollution and secondhand smoke helps. Eating well and maintaining a healthy weight reduces strain on your lungs. Pulmonary rehab teaches energy-saving techniques and breathing control, which improve daily function. Staying active within your limits slows muscle loss and keeps your heart stronger, which helps your body use oxygen more efficiently.
How do I know if I have ILD and not asthma?
Asthma causes wheezing and reversible airflow blockage-you respond to inhalers. ILD causes dry cough, progressive shortness of breath, and low oxygen levels that don’t improve with inhalers. Pulmonary function tests show a restrictive pattern in ILD (low lung volume), not obstructive like asthma. A high-resolution CT scan will show scarring in ILD, which asthma never does. If your symptoms don’t improve with asthma meds, ask for a CT scan and referral to a lung specialist.
Write a comment
Your email address will not be published.





8 Comments
lol so now they're saying scarring is permanent but also 'early detection changes everything'? sounds like they just want you to pay for 9k/month drugs and then tell you you should've done it sooner. i bet the pharma execs are laughing all the way to the bank while we're choking on oxygen tubes. 🤡
Bro the real conspiracy? They don't want you to know that vitamin D and turmeric can reverse fibrosis. 🤫 I had my buddy's uncle who had IPF and he just took 10k IU of D3 daily and now he's hiking in Colorado. The FDA banned the studies because Big Pharma doesn't profit from sunlight. 😤💊
Interesting post. I live in Delhi and we see many cases here from air pollution. The scarring is real, but I've noticed people who walk daily, even slowly, seem to hold on longer. Not sure if science backs it, but movement helps. No need for drama. Just breathe.
why are we even talking about this? i mean, if you're gonna die from lung scarring, just accept it. why waste money on $9k pills? just get a nice recliner, watch netflix, and chill. they're just trying to scare you into buying stuff. i'm not falling for it.
The data is cherry-picked. Pirfenidone’s 50% slowdown? Compared to placebo, which had a 15% annual decline. That’s not a miracle-it’s a 35% relative improvement, which translates to maybe 6 extra months over 5 years. And the side effects are brutal. This isn’t progress. It’s profit-driven palliation dressed as medicine.
In India, we have been watching this for decades. The West has always had the luxury of expensive drugs and CT scans. Here, people die quietly because they can't afford oxygen concentrators or even basic spirometry. The real disease isn't fibrosis-it's inequality. They write these articles to make rich people feel good about their insurance while the poor cough themselves to death in villages with no doctors. This isn't science. It's colonialism with a stethoscope.
You missed a critical point: the MUC5B gene variant isn't just a predictor-it's a diagnostic marker with 87% specificity for aggressive IPF. If you're reading this and you have a family history of unexplained lung decline, get tested. Not 'maybe,' not 'if you feel like it.' This isn't speculation. It's evidence-based medicine. And if you're still using 'just breathe' as a coping mechanism, you're endangering yourself and your loved ones.
While the pharmacological interventions described are indeed noteworthy, one must not overlook the fundamental anthropological and socioeconomic determinants that underpin the dissemination and accessibility of such therapeutic modalities. In many developing nations, the absence of infrastructure renders even the most efficacious pharmaceuticals inaccessible. Thus, the narrative of 'early detection' remains, in practice, a privilege of the affluent. The true challenge lies not in the biology of fibrosis, but in the architecture of global healthcare equity.