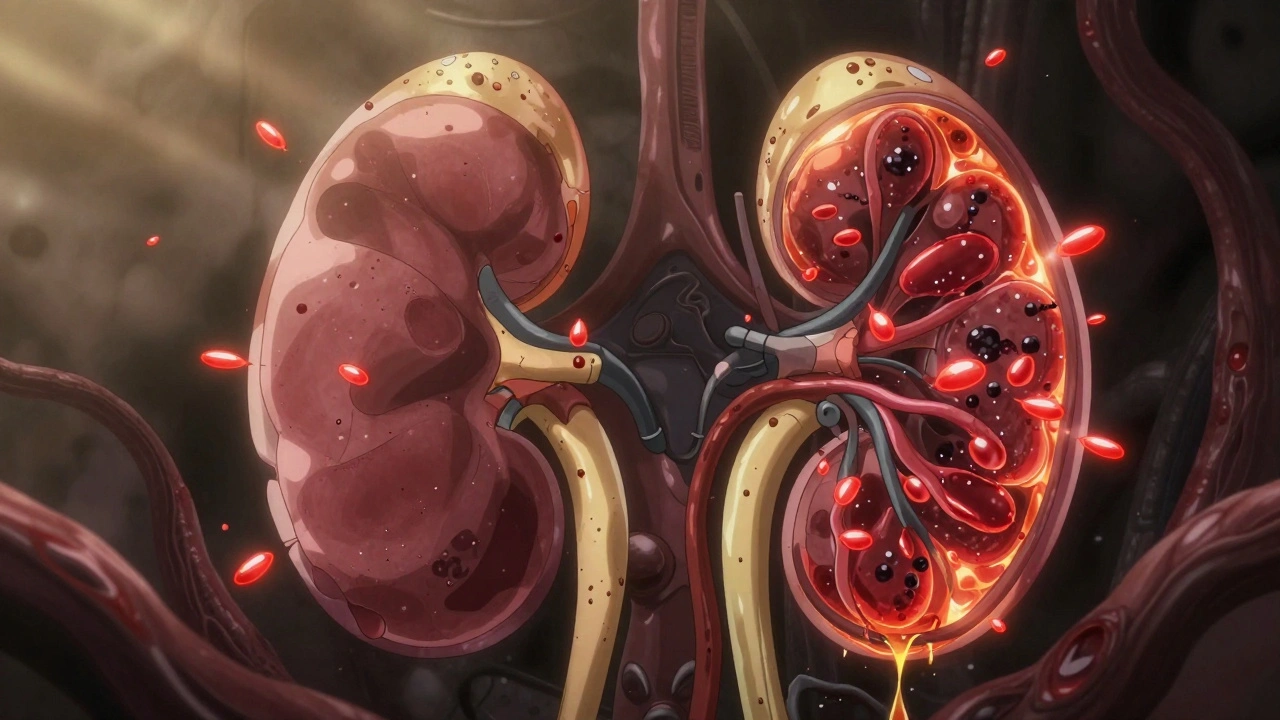
When your kidneys start to fail, it doesn’t happen overnight. It’s a slow leak - a quiet breakdown you might not notice until it’s too late. About one in three adults in the U.S. has risk factors for kidney failure, and most don’t know it. The top three causes? Diabetes, high blood pressure, and glomerulonephritis. These aren’t just random conditions. They’re direct attackers of your kidneys, each with its own path of destruction.
Diabetes: The Silent Kidney Killer
Diabetes is the number one cause of kidney failure worldwide. In the U.S., it’s responsible for nearly half of all new cases of end-stage renal disease (ESRD). That’s not a coincidence. High blood sugar doesn’t just mess with your nerves or eyes - it wrecks your kidneys from the inside.
Here’s how it works: When glucose levels stay high, your kidneys work overtime to filter it out. This forces the tiny filtering units - called glomeruli - to stretch and strain. Within the first year of uncontrolled diabetes, these filters start to thicken. The basement membrane, normally 300-400 nanometers thick, swells to 450-650 nm. That’s like turning a fine sieve into a clogged coffee filter.
Early signs are easy to miss. You might not feel anything. But your urine starts leaking protein - albumin. That’s the first red flag. Doctors call it microalbuminuria when levels hit 30-300 mg/g. At this stage, there’s still time to stop the damage. If it climbs to macroalbuminuria (over 300 mg/g), your risk of full kidney failure in five years jumps to 44%.
What helps? Tight blood sugar control. Getting your HbA1c under 7% within five years of diagnosis cuts kidney disease risk by over half. New drugs like SGLT2 inhibitors (e.g., empagliflozin) don’t just lower sugar - they protect your kidneys directly. The EMPA-KIDNEY trial showed a 32% drop in kidney failure risk. Even better, they reduce heart attacks and death. These aren’t just diabetes drugs anymore - they’re kidney-saving tools.
Hypertension: The Pressure That Crushes Your Filters
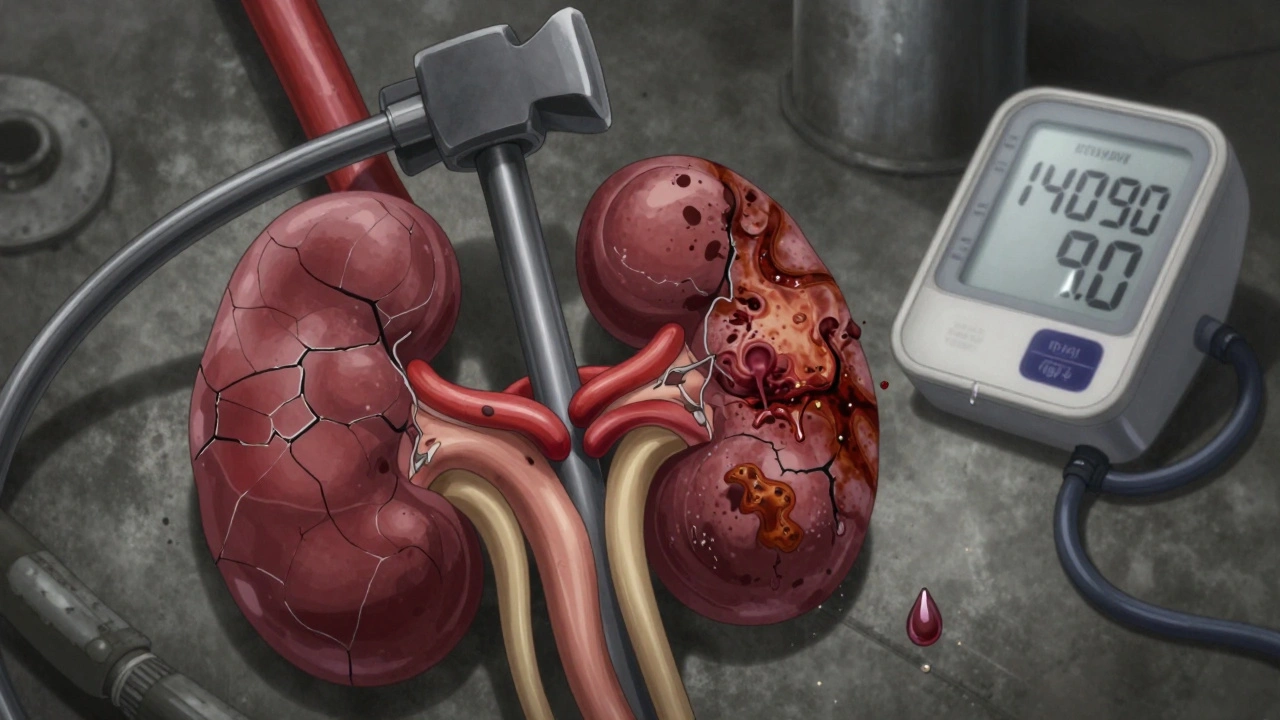
High blood pressure is the second leading cause of kidney failure. It’s not just a number on a machine. Every time your blood pressure stays above 140/90 mmHg, it’s like constant hammering on your kidney’s blood vessels. Over time, the small arteries inside your kidneys harden and narrow. This is called nephrosclerosis.
The result? Less blood flow to the glomeruli. Without enough blood, those filters starve. About 60-70% of people with long-term high blood pressure show scarring in 25-40% of their glomeruli. And here’s the kicker: if you have both diabetes and high blood pressure, your kidneys decline 3.2 mL/min/1.73m² faster each year than if you had diabetes alone.
Many people don’t realize their blood pressure is high because there are no symptoms. That’s why it’s called the silent killer. You might feel fine, but your kidneys are slowly dying. The good news? Lowering your systolic pressure to under 120 mmHg reduces kidney failure progression by 27%. But it’s not one-size-fits-all. For older adults, pushing too low can cause dizziness or falls. The target? <130/80 mmHg for diabetics, <120/80 for those with protein in the urine.
Medications like ACE inhibitors and ARBs are the first line of defense. They don’t just lower blood pressure - they reduce protein leakage and slow scarring. But adherence is a problem. Only 58% of patients take them consistently after a year. Missing doses means faster decline. And it’s not just pills - salt intake matters. Cutting back to under 5 grams a day helps more than most people realize.
Glomerulonephritis: When Your Immune System Turns on Your Kidneys
Glomerulonephritis is less common than diabetes or hypertension, but it’s more complex. It’s not caused by lifestyle - it’s caused by your own immune system attacking your kidneys. Think of it like an autoimmune civil war inside your body.
The most common type is IgA nephropathy. It’s where immune proteins called IgA build up in the glomeruli, causing inflammation. It’s more common in Asia than in the West, and it often flies under the radar. One patient on Reddit said they saw seven doctors over 18 months before getting diagnosed. That’s not unusual. Symptoms like foamy urine or blood in the urine are often dismissed as a “bad cold” or “strep throat.”
Another form is lupus nephritis, which affects up to 60% of people with systemic lupus. Class IV lupus nephritis - the most aggressive - leads to kidney failure in nearly 30% of cases within 10 years. Diagnosis requires a kidney biopsy. No blood test can confirm it.
Treatment is different here. You don’t just control blood pressure or sugar. You need to suppress the immune system. Drugs like rituximab cut the risk of kidney failure by 48% in high-risk IgA patients. But there’s debate. Some experts warn that aggressive treatment in older patients increases infection risk without clear benefit. Others say early intervention saves years of dialysis.
There’s new hope. Sparsentan, a dual-acting drug approved in 2024, reduced proteinuria by nearly 48% in trials - far better than older drugs. It’s not a cure, but it’s a major step forward.
How Fast Do They Progress?
Not all kidney failure is the same. The speed varies wildly.
- Diabetic kidney disease: From first signs of albuminuria to full failure, it takes about 8.7 years on average.
- Hypertensive kidney disease: Slower. Around 12.3 years from diagnosis to ESRD.
- Glomerulonephritis: Highly unpredictable. Some people hold off for 20 years. Others crash in 5.
What makes the difference? Early detection. If you catch albuminuria early and start an SGLT2 inhibitor, you might never reach dialysis. If you ignore high blood pressure for a decade, you’re already on the path.

What You Can Do - Right Now
You don’t need a PhD to protect your kidneys. You just need to act.
- If you have diabetes: Get your urine tested for albumin at least once a year. Ask your doctor about SGLT2 inhibitors if your levels are above 30 mg/g.
- If you have high blood pressure: Check it regularly. Don’t wait for symptoms. Aim for under 130/80. Cut salt. Take your meds - even when you feel fine.
- If you notice foamy urine, swelling in your legs, or unexplained fatigue: Don’t brush it off. Ask for an eGFR test and a urine albumin-to-creatinine ratio. These are simple, cheap, and life-changing.
- If you have autoimmune disease like lupus: Monitor kidney function every 3-6 months. Don’t assume you’re fine just because you’re not sick.
The biggest mistake? Waiting until you feel bad. By then, it’s often too late. Kidneys don’t scream. They whisper. And if you’re not listening, you’ll miss it.
What’s Next for Kidney Care?
Science is moving fast. New biomarkers like urinary TNF receptor-1 can predict kidney failure with 89% accuracy - years before traditional tests. Finerenone, a newer drug approved in 2023, reduces kidney failure risk by 18% in diabetics. And global efforts are pushing for universal screening in high-risk groups.
But the real breakthrough isn’t a drug. It’s awareness. If 30-50% of projected kidney failures can be prevented with current tools, then the problem isn’t lack of solutions. It’s lack of action.
Diabetes, hypertension, glomerulonephritis - they’re not just diseases. They’re warning signs. Your kidneys are telling you something. Listen before it’s too late.
Can kidney failure be reversed?
Once kidneys reach end-stage failure (ESRD), they can’t heal themselves. But early damage - like protein leakage or mild eGFR drop - can often be slowed or even reversed with tight control of blood sugar, blood pressure, and immune activity. The key is catching it before scarring sets in.
Do I need a kidney biopsy if I have protein in my urine?
Not always. If you have diabetes or high blood pressure, protein in the urine usually points to those causes. But if you’re young, have blood in your urine, or no clear risk factors, a biopsy is often needed to rule out glomerulonephritis or other immune-related diseases.
Are SGLT2 inhibitors safe for everyone?
Most people tolerate them well, but they’re not for everyone. They’re not recommended if your eGFR drops below 20 mL/min/1.73m². They can also increase the risk of genital yeast infections or rare but serious conditions like Fournier’s gangrene. Talk to your doctor about your risks and benefits.
Can I prevent kidney failure if I have high blood pressure but no diabetes?
Yes. Controlling your blood pressure is the single most effective step. Combine it with a low-salt diet, regular exercise, and avoiding NSAIDs like ibuprofen. Taking an ACE inhibitor or ARB can cut your kidney failure risk by up to 30%, even without diabetes.
How often should I get my kidneys checked?
If you have diabetes or high blood pressure: test your urine for albumin and your blood for eGFR at least once a year. If you have a family history of kidney disease or autoimmune conditions like lupus, get tested every 6 months. If you’re healthy with no risk factors, testing every 2-3 years is fine.
If you’re managing diabetes, high blood pressure, or an autoimmune condition, your kidneys are your silent partners. They work 24/7, filtering toxins, balancing fluids, and regulating blood pressure - all without asking for thanks. The least you can do is check on them. A simple urine test, a blood pressure check, and a conversation with your doctor might save you from dialysis. Don’t wait for symptoms. The damage is already happening.
Write a comment
Your email address will not be published.





14 Comments
lol so diabetes is the #1 cause?? 😂 like duh. But have u heard about the big pharma pumpin' out SGLT2 inhibitors to keep us hooked? They're not saving kidneys... they're just makin' sure we keep buyin' meds. 🤡 #BigPharmaLies
Seriously though, if you're diabetic and your HbA1c is over 7%, you're basically playing Russian roulette with your kidneys. 🚨 SGLT2 inhibitors? Game-changer. Empagliflozin isn't just a drug-it's a lifeline. Pair it with low-carb + daily walks and you're lookin' at a 60% risk drop. 💪肾
Wait, so you're telling me high BP crushes your glomeruli? Bro, I've been told that since med school. But here's the thing-most docs don't even check urine albumin till it's too late. You need a dipstick test every 6 months if you're hypertensive. Period. 🤓
I'm from Australia and we've got a killer national kidney screening program-free urine tests for anyone over 50 with diabetes or HTN. Why can't the US do this? We don't wait for people to collapse before we act. It's not rocket science-it's public health. 🇦🇺❤️
There's a quiet revolution happening here. It's not just about drugs or numbers-it's about shifting from crisis mode to prevention mode. Your kidneys aren't broken because you're weak. They're broken because we treat symptoms, not systems. Change your habits, not just your meds.
I don't trust any of this. I read on a forum that the CDC is hiding the real cause-EMFs from 5G towers are frying kidney cells. And the SGLT2 drugs? They're just cover-ups. My cousin's uncle's neighbor had kidney failure after his phone got too hot. Coincidence? I think not. 📱💀
It is, indeed, a matter of considerable scientific consensus that diabetic nephropathy constitutes the principal etiology of end-stage renal disease in the contemporary Western milieu. However, one must also acknowledge the confounding influence of socioeconomic determinants upon therapeutic adherence.
You people act like this is some new revelation. I've been telling my friends for years: if you're eating processed carbs and sitting on your ass, you're not 'at risk'-you're already dead inside. Your kidneys are just the first to scream. Stop blaming the system. Start blaming yourself.
I just lost my mom to kidney failure... she never felt sick until she was on dialysis. I wish someone had told her about the urine test. I'm so glad this post is out there. 🫂
This is all just feel-good fluff. You think a 7% HbA1c is enough? Try 5.5%. You think SGLT2 inhibitors are magic? They cost $800 a month. Most people can't afford them. This isn't medicine-it's privilege. Wake up.
Glomeruli are like the kidneys' tiny espresso machines-clog 'em with sugar and pressure, and they start spitting out protein like a broken latte foam wand. 🤯 And SGLT2 inhibitors? They're the barista who fixes the machine before it explodes. This isn't science-it's poetry.
I'm so glad someone finally said this. My husband's BP was 150/95 for years. We thought he was fine because he didn't have headaches. Then his creatinine spiked. We were lucky. So many aren't. Please get checked. Even if you feel fine.
so like... diabetes = bad? wow. mind blown. 🤡 also why is everyone acting like this is new info? i learned this in 8th grade health class. also my cousin's dog has better kidneys than me.
To everyone panicking: you're not doomed. Start with one change. Walk 15 minutes a day. Cut out soda. Get a urine test. Small steps save kidneys. You got this. 💙