Every time a pharmacist swaps a brand-name drug for a generic, they’re making a decision that could land them in court. It’s not just about saving money-it’s about who pays when something goes wrong. In 2026, with 90% of prescriptions filled as generics, this isn’t a rare edge case. It’s daily practice. And the legal landscape? It’s a maze with no clear exit.
Why Generic Substitution Comes With Legal Traps
The 1984 Hatch-Waxman Act made generic drugs possible by letting manufacturers skip expensive clinical trials. All they had to prove was bioequivalence: their version of the drug hits the bloodstream within 80-125% of the brand’s levels. Sounds fair, right? But here’s the catch: bioequivalence doesn’t mean therapeutic equivalence. For drugs like warfarin, levothyroxine, or antiepileptics, even a 5% difference in absorption can trigger seizures, strokes, or heart rhythm problems. The real legal trap came in 2011, when the Supreme Court ruled in PLIVA v. Mensing that generic drug makers can’t be sued for failing to update warning labels. Why? Because federal law forces them to use the exact same label as the brand-name version. They can’t change it-even if new safety data emerges. That means if a patient has a bad reaction to a generic, the manufacturer can’t be held accountable under state law. And since pharmacists are just dispensing what’s legally approved, they’re often left holding the bag.State Laws Are a Wild West
There’s no national rulebook. Each state sets its own rules for substitution, and the differences are huge. - In 27 states, pharmacists must substitute unless the doctor says no. - In 23 states, substitution is optional. - 18 states require pharmacists to tell patients directly-beyond just the label. - 32 states let patients refuse substitution. - 27 states shield pharmacists from extra liability if they substitute. - 23 states? No protection at all. Connecticut even says pharmacists could face more liability for substituting. This creates a nightmare for pharmacists who work across state lines or handle prescriptions from out-of-state prescribers. One day you’re following California’s strict consent rules. The next, you’re in Texas where substitution is automatic. One mistake-and you’re on the hook.The High-Risk Drugs You Can’t Afford to Guess On
Not all generics are equal. For drugs with a narrow therapeutic index (NTI), tiny changes in blood levels can be deadly. - Levothyroxine: A 2022 Reddit thread with over 4,000 upvotes detailed how patients switched to generic versions and developed fatigue, weight gain, and brain fog-symptoms that vanished after switching back. - Antiepileptics: The American Epilepsy Society found a 7.9% increase in seizure risk after generic switches. A 2017 study showed 18.3% of patients had therapeutic failure. - Warfarin: Even small variations in absorption can lead to clots or dangerous bleeding. - Immunosuppressants: Transplant patients can reject organs if levels dip slightly. Yet in 2022, 98% of statin prescriptions were filled as generics. Only 37% of antiepileptic prescriptions were. Why? Pharmacists know the risk. Many refuse to substitute NTI drugs even when the law allows it-just to stay safe.
What Pharmacists Are Doing to Protect Themselves
The smart ones aren’t waiting for lawmakers to fix this. They’re building their own safety nets.- Electronic alerts in their pharmacy software flag NTI drugs. If a prescription for levothyroxine comes in, the system pops up: “Check state law. Patient consent required.”
- Standardized consent forms are now common. Patients sign before substitution, acknowledging they understand the switch and have the right to refuse.
- Substitution logs track batch numbers. If a patient reports side effects, pharmacists can trace exactly which generic was dispensed.
- Communication with prescribers is key. Many pharmacists now call doctors directly if they’re unsure-especially for high-risk patients.
- Supplemental malpractice insurance specifically covering substitution risks is no longer optional. Premiums rose 18% since 2011, but the cost of a lawsuit is far higher.
The Patient Perspective: Confused, Uninformed, and Angry
Most patients have no idea their prescription was switched. A 2021 Patient Advocacy Foundation survey found 41% didn’t realize they’d been given a generic until they felt worse. Only 28% said their pharmacist gave them the legally required notification in their state. On GoodRx, 82% of users are happy with generics for common drugs like metformin or lisinopril-they save $327 a year on average. But for NTI drugs, trust evaporates. One patient wrote: “I’ve been on the same brand of levothyroxine for 12 years. My pharmacist switched me without asking. I went from feeling fine to needing a wheelchair. They told me it was ‘the same thing.’ It wasn’t.” Patients aren’t against generics. They’re against being treated like a cost-saving experiment.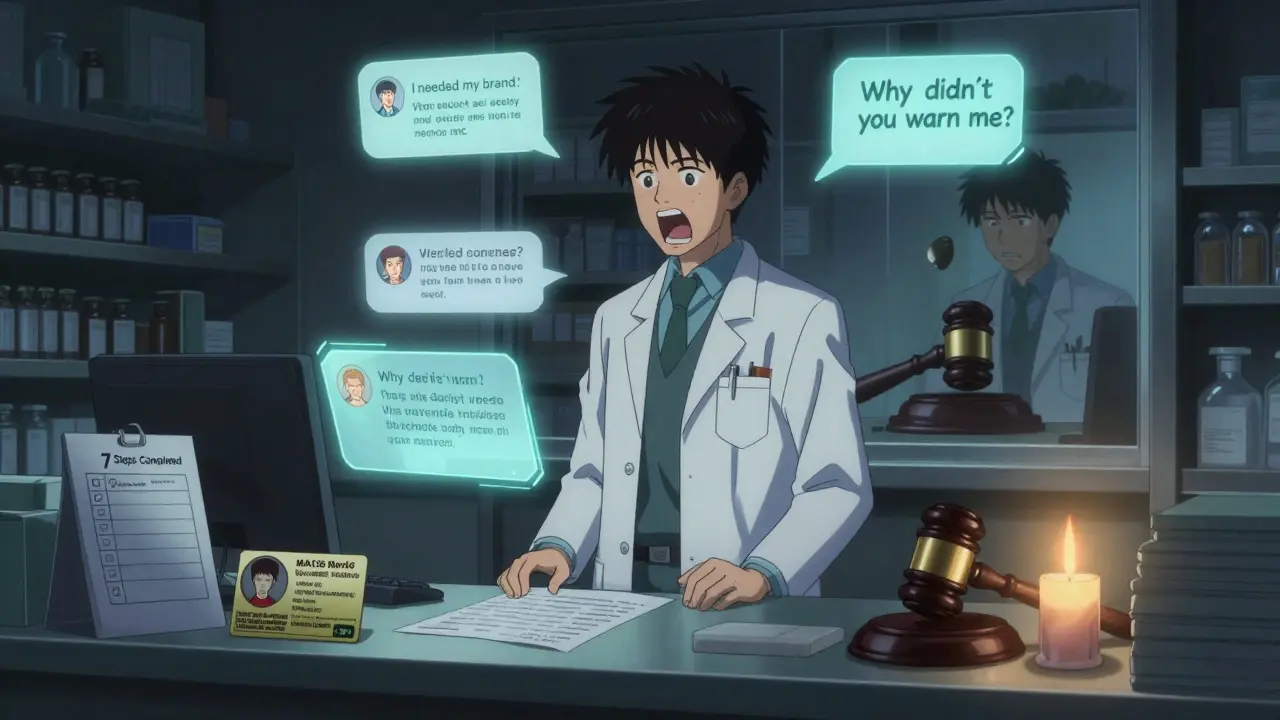
What’s Changing-And What’s Not
In 2023, 11 states introduced the Generic Drug Safety Act. It would require brand-name manufacturers to update labels within 30 days of new safety data-and force generic makers to adopt those changes within 60. That’s a big deal. Right now, generic companies don’t even initiate label updates. They wait for the brand to act. The FDA’s pilot program for label changes has approved 68% of requests, but generic manufacturers only started 12% of them. That’s not a system designed for safety-it’s a system designed to keep prices low. The Congressional Budget Office estimates the current liability gap costs $4.2 billion a year in untreated adverse events. Fixing it could raise generic prices by 7-12%. But it could also prevent 14,000 serious injuries each year.What You Need to Do Today
If you’re a pharmacist, here’s your checklist:- Know your state’s laws-and check them every January. The National Association of Boards of Pharmacy updates them yearly.
- Use your EHR to auto-flag NTI drugs. Don’t rely on memory.
- Get written consent for any substitution of levothyroxine, warfarin, antiepileptics, or immunosuppressants-even if your state doesn’t require it.
- Document everything. The date, the drug, the batch number, the patient’s verbal consent, your call to the prescriber. Paper trails save careers.
- Don’t substitute NTI drugs unless you’re 100% sure the patient understands. When in doubt, call the doctor. Or don’t substitute at all.
Can a pharmacist be sued for substituting a generic drug?
Yes, but it depends on the state and the drug. In 23 states, pharmacists have no legal protection from liability for substitution. If a patient has a bad reaction to a generic-especially a narrow therapeutic index drug like levothyroxine or warfarin-they can sue the pharmacist for not obtaining consent, not documenting properly, or substituting when it was medically inappropriate. Federal law protects generic manufacturers, but not pharmacists.
Are all generic drugs safe to substitute?
No. Generic drugs are required to be bioequivalent, meaning they deliver similar levels of the active ingredient into the bloodstream. But for drugs with a narrow therapeutic index-like antiepileptics, warfarin, levothyroxine, and immunosuppressants-small differences in absorption can cause serious harm. Studies show increased seizure risk, thyroid instability, and bleeding events after substitution. These are not interchangeable without caution.
Do I have to tell my patients when I substitute a generic?
In 18 states, yes-by law, you must give patients independent notice beyond the label. In many other states, it’s not required, but it’s still a best practice. Patients who aren’t informed often blame the pharmacist when side effects occur. Clear communication reduces complaints, builds trust, and lowers your legal risk.
What’s the biggest mistake pharmacists make with generic substitution?
Assuming bioequivalence means therapeutic equivalence. Just because a generic meets FDA standards doesn’t mean it’s safe to swap for every patient. The biggest errors happen with high-risk drugs like levothyroxine or antiepileptics, where pharmacists substitute automatically without checking the patient’s history, consulting the prescriber, or getting consent. That’s how lawsuits start.
Is there a way to reduce my liability insurance costs?
Yes. Pharmacies that implement documented consent protocols, use electronic alerts for high-risk drugs, maintain substitution logs, and complete annual risk assessments often qualify for lower premiums. Some insurers offer discounts for following the American Society of Health-System Pharmacists’ 7-step safety framework. The upfront work pays off in lower premiums and fewer claims.
Write a comment
Your email address will not be published.




1 Comments
So basically pharmacists are the new scapegoats? 😩 I just got my levothyroxine switched and I felt like a zombie for 3 weeks. No one told me. No one asked. Now I’m stuck paying extra to get the brand back. Thanks, system.