Rifampin Interaction Calculator
Calculate Your Medication Risk
Rifampin can significantly reduce the effectiveness of anticoagulants and antivirals. Enter your medication to see the potential interaction and management recommendations.
When you’re on rifampin for tuberculosis or to prevent meningitis, you might not think twice about your other meds-until your blood clotting levels drop suddenly, or your antiviral stops working. That’s not a coincidence. Rifampin is one of the most powerful drug inducers in clinical use, and it can slash the effectiveness of anticoagulants and antivirals by more than half. This isn’t theoretical. It’s happened in real patients, leading to strokes, clots, and treatment failures. If you’re taking rifampin along with blood thinners or antivirals, you need to know exactly what’s happening inside your body-and what to do about it.
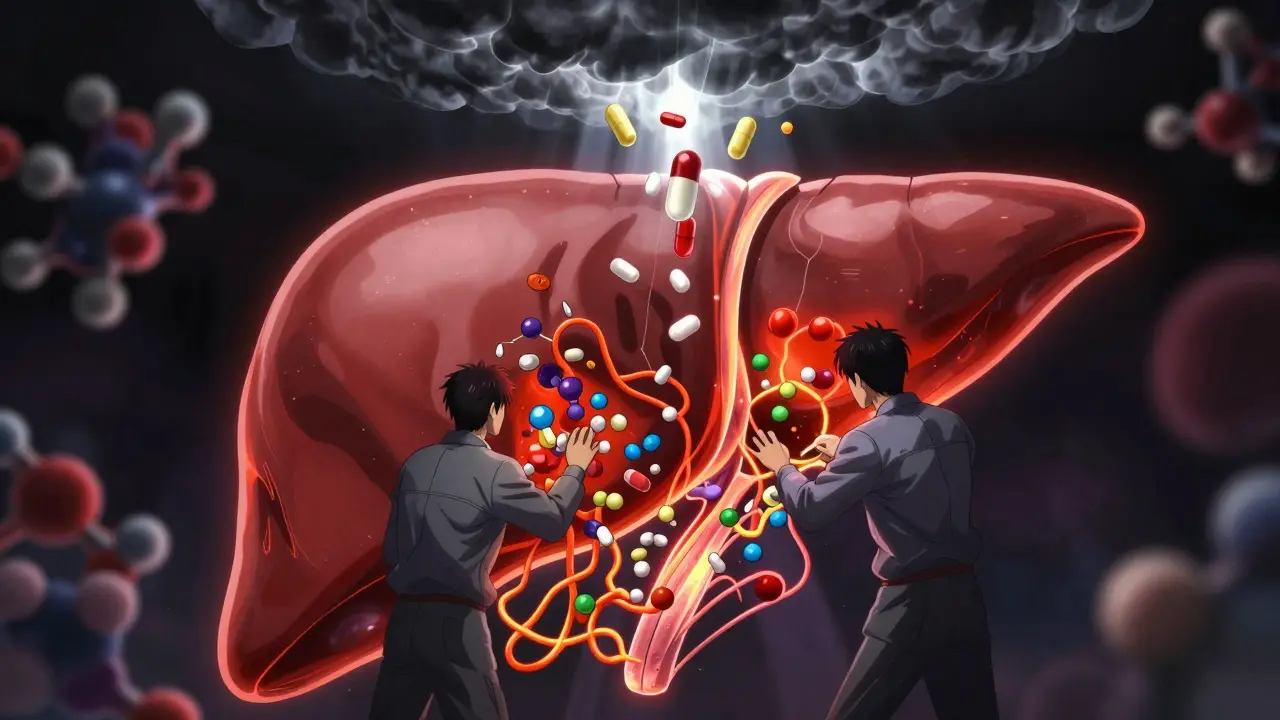
How Rifampin Turns Off Your Medications
Rifampin doesn’t block your drugs. It makes your liver work too hard. It activates a protein called the pregnane X receptor (PXR), which tells your liver to produce more of the enzymes that break down medications. The main ones affected are CYP3A4 and CYP2C9. These enzymes are like factory workers that process drugs so your body can get rid of them. When rifampin turns up their production, your anticoagulants and antivirals get broken down faster than normal. The result? Less drug in your bloodstream. Less protection.
The effect starts within 24 to 48 hours of taking rifampin. By day five or seven, it’s at full strength. And here’s the catch: it doesn’t stop when you stop rifampin. Enzymes stick around for two to three weeks after you finish the course. That means your medication levels stay low even after you’re done with antibiotics. Many patients don’t realize this-and end up with dangerous gaps in protection.
Warfarin and Other VKAs: The Classic Danger Zone
Warfarin has been the go-to anticoagulant for decades. But it’s also one of the most vulnerable to rifampin. Studies show that when rifampin is added, warfarin’s concentration in the blood drops by 15% to 74%. That’s not a small change-it’s enough to make INR levels plunge from therapeutic (2.0-3.0) to dangerously low (below 1.5).
One case report followed a 57-year-old woman with a mechanical heart valve. She was stable on phenprocoumon, another vitamin K antagonist. When rifampin was started for suspected endocarditis, her INR dropped to normal-despite her continuing the same dose. She was at high risk for a life-threatening clot. Only after switching to heparin injections and waiting 15 days after stopping rifampin did her INR return to safe levels.
Why is this so unpredictable? Because warfarin has two forms: S-warfarin and R-warfarin. S-warfarin is the stronger one, and it’s broken down almost entirely by CYP2C9-the very enzyme rifampin induces. So even if you increase your warfarin dose, you might still not get consistent control. Some patients need three to five times their original dose just to stay in range. And even then, the risk of bleeding or clotting stays high.
Direct Oral Anticoagulants (DOACs): Even More Unpredictable
DOACs like rivaroxaban, apixaban, dabigatran, and edoxaban were supposed to be easier to manage than warfarin. No more frequent blood tests. No dietary restrictions. But they’re not safe with rifampin. In fact, they’re often worse.
Studies show that when rifampin is taken with rivaroxaban, its blood levels drop by 50-67%. Same with apixaban and dabigatran. Edoxaban drops by about 35%, but its active metabolites rise, making the interaction even harder to predict. The European Heart Rhythm Association says combining DOACs with rifampin “necessitates vigilance and monitoring”-which is medical code for “don’t do this unless you have no choice.”
Here’s the problem: unlike warfarin, DOACs don’t have a simple test like INR to check if they’re working. You can’t just draw blood and know if your dose is right. If your rivaroxaban level drops 60%, you won’t feel it. You won’t bleed. You won’t know you’re unprotected until you have a stroke.
A 2021 study tracked six patients with prosthetic joint infections who needed both rifampin and rivaroxaban. Researchers found that simply increasing the dose didn’t help-it led to unpredictable spikes and drops. The safest approach? Adjust slowly, monitor closely, and avoid abrupt changes when starting or stopping rifampin.

Antivirals: Hidden Risks in HIV and Hepatitis Treatment
Rifampin doesn’t just mess with blood thinners. It also wrecks antivirals. For people with HIV or hepatitis C, this can be deadly. Many antivirals-especially those based on protease inhibitors or non-nucleoside reverse transcriptase inhibitors-are metabolized by CYP3A4. Rifampin can cut their levels by 70-90%.
Take darunavir, a common HIV drug. When paired with rifampin, its concentration drops so low that the virus can bounce back, leading to drug resistance. Same with sofosbuvir/velpatasvir for hepatitis C. Studies show a 60% drop in sofosbuvir levels when taken with rifampin. That’s enough to make the cure fail.
There are exceptions. Some newer antivirals, like cabotegravir, are less affected. But most aren’t. That’s why HIV guidelines from the U.S. Department of Health and Human Services say rifampin should never be used with most antiretroviral regimens. If a patient has TB and HIV, doctors must switch to alternative TB drugs like rifabutin-which is a weaker inducer-or use boosted antivirals with higher doses. But even then, it’s risky.
What Doctors Do When Rifampin Is Necessary
When someone needs rifampin-say, for TB or a stubborn infection-and they’re already on anticoagulants, the standard advice is simple: switch away from oral anticoagulants entirely.
The American College of Chest Physicians recommends switching from warfarin or DOACs to low molecular weight heparin (LMWH), like enoxaparin. These are injected under the skin and aren’t broken down by liver enzymes. They’re not perfect-still need monitoring, still carry bleeding risks-but they’re safe with rifampin.
After rifampin is stopped, you wait two to three weeks before restarting an oral anticoagulant. Then you start low and titrate up slowly. INR checks every few days. For DOACs, there’s no clear protocol. Some hospitals use specialized blood tests to measure drug levels, but only 12% of U.S. hospitals have those capabilities as of 2022.
For antivirals, the approach is similar. If possible, replace rifampin with rifabutin, which is less potent at inducing enzymes. Or switch the antiviral to something less affected. For HIV, dolutegravir-based regimens are often used with rifampin because they’re more stable. For hepatitis C, newer regimens like glecaprevir/pibrentasvir may be safer-but only if dosed correctly and monitored.

What You Can Do If You’re on Both
If you’re taking rifampin and an anticoagulant or antiviral, here’s what you need to do:
- Don’t change your dose on your own. Even small changes can be dangerous.
- Ask your doctor about switching to heparin injections during rifampin treatment.
- If you’re on a DOAC, ask if switching to warfarin with frequent INR checks is safer.
- Use a home INR monitor if you’re on warfarin. Accuracy is 95% within ±0.5 INR units-close enough to catch problems early.
- Track every medication you take. Even over-the-counter supplements like St. John’s wort can add to the problem.
- Don’t stop rifampin early, even if you feel better. Stopping early can cause drug-resistant TB.
- After rifampin ends, wait at least two weeks before restarting your anticoagulant or antiviral-and do it under close supervision.
The Future: Anticoagulants That Don’t Care About Rifampin
Drug makers are learning from this. New anticoagulants like milvexian, which targets factor XIa instead of thrombin or factor Xa, are being designed to avoid CYP metabolism entirely. Early studies show they’re not affected by rifampin. That’s a big deal. If they work as planned, future patients won’t have to choose between treating TB and preventing strokes.
The FDA now requires new drugs to be tested against strong inducers like rifampin before approval. That means labels for newer anticoagulants and antivirals are clearer. But for the millions already on these drugs, the risk remains. Rifampin isn’t going away. TB is still deadly. And in many parts of the world, it’s the only affordable option.
Until better drugs are widely available, the key is awareness. If you’re on rifampin, your anticoagulant or antiviral isn’t working the way it should. That’s not your fault. It’s a known, predictable interaction. But it’s one that can kill you if no one’s watching.
Can I take rifampin with warfarin if I increase the dose?
Increasing the warfarin dose may help temporarily, but it’s risky. Rifampin causes unpredictable drops in warfarin levels, especially for S-warfarin, which is the more active form. Even with higher doses, INR can still fall below therapeutic range. The safest approach is to switch to heparin injections during rifampin treatment and only restart warfarin after waiting 2-3 weeks post-rifampin, with close INR monitoring.
Are DOACs safer than warfarin when taking rifampin?
No. DOACs like rivaroxaban, apixaban, and dabigatran are just as vulnerable to rifampin as warfarin-sometimes more so. They can lose 50-67% of their effectiveness. The big problem? There’s no simple test like INR to check if they’re working. You might not realize your anticoagulation has failed until you have a stroke or clot. Most guidelines recommend avoiding DOACs entirely when rifampin is needed.
How long does rifampin affect my medications after I stop taking it?
Rifampin’s effects last for 2 to 3 weeks after you stop taking it. That’s because the liver enzymes it induces take time to break down. Restarting anticoagulants or antivirals too soon can lead to dangerously low levels. Always wait at least two weeks after your last rifampin dose before resuming these drugs, and do so under medical supervision.
Can I use rifabutin instead of rifampin to avoid this interaction?
Yes, rifabutin is a weaker inducer of CYP3A4 and is often used as an alternative to rifampin in patients on HIV medications or anticoagulants. While it still causes some interaction, it’s less severe. Dose adjustments are still needed, but it’s a safer option when available and appropriate for the infection being treated.
Why don’t doctors always catch this interaction?
Many clinicians don’t realize how strong rifampin’s effect is-or how long it lasts. It’s also complicated by the fact that newer DOACs are often prescribed without routine monitoring. A 2022 survey found only 12% of U.S. hospitals had protocols for managing rifampin-DOAC interactions. Without clear guidelines and awareness, these dangerous combinations slip through the cracks.
Bottom Line: Don’t Guess. Test. Switch. Wait.
If you’re on rifampin, your anticoagulant or antiviral is probably not working right. This isn’t a minor adjustment-it’s a major clinical risk. The safest path isn’t to tweak doses. It’s to switch to an alternative that won’t interact. Use heparin. Wait. Then restart carefully. The goal isn’t just to keep your INR in range. It’s to avoid a stroke, a clot, or a treatment-resistant infection. That’s not something you can afford to gamble on.